Uterine smooth muscle tumor of uncertain malignant potential: A rare cause of multiple pulmonary nodules
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2012; 33(03): 176-178
DOI: DOI: 10.4103/0971-5851.103148
Abstract
Smooth muscle tumors of uncertain malignant potential (STUMP) are mesenchymal uterine tumors lying between benign leiomyomas and leiomyosarcomas. Although lung metastases from uterine leiomyosarcoma are common, ′′STUMP′′ usually does not metastasize. A case of a 51-year-old woman with progressive dyspnea on exertion and multiple space-occupying lesions in both lungs is presented. She had a history of a total abdominal hysterectomy 3 years ago. Lung biopsy through video-assisted thoracic surgery was consistent with metastatic malignant smooth muscle cell tumor. She received multiple cycles of chemotherapy and died 11 months later. Cell necrosis, atypia and mitotic count are important criteria determining the malignant potential of a uterine smooth muscle tumor. The diagnosis and clinical course of STUMP are not totally and clearly known, and metastasis, especially pulmonary with pleural effusion, is not a common phenomenon. When this occurs, prognosis seems to be poor. Surveillance of these patients should be close and long term.
Publication History
Article published online:
02 August 2021
© 2012. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Smooth muscle tumors of uncertain malignant potential (STUMP) are mesenchymal uterine tumors lying between benign leiomyomas and leiomyosarcomas. Although lung metastases from uterine leiomyosarcoma are common, “STUMP” usually does not metastasize. A case of a 51-year-old woman with progressive dyspnea on exertion and multiple space-occupying lesions in both lungs is presented. She had a history of a total abdominal hysterectomy 3 years ago. Lung biopsy through video-assisted thoracic surgery was consistent with metastatic malignant smooth muscle cell tumor. She received multiple cycles of chemotherapy and died 11 months later. Cell necrosis, atypia and mitotic count are important criteria determining the malignant potential of a uterine smooth muscle tumor. The diagnosis and clinical course of STUMP are not totally and clearly known, and metastasis, especially pulmonary with pleural effusion, is not a common phenomenon. When this occurs, prognosis seems to be poor. Surveillance of these patients should be close and long term.
INTRODUCTION
Smooth muscle tumors of uncertain malignant potential (STUMP) are mesenchymal uterine tumors lying between benign leiomyomas and leiomyosarcomas. The term “STUMP” contains a heterogeneous group of rare tumors.[1] There is lack of clinicopathologic details and follow-up data of these neoplasms. Histological diagnosis is challenging and usually problematic. The value, in the differential diagnosis, of a number of surface markers, like p16 and p21, has been studied.[2] Natural history of the disease as well as the malignant potential remains uncertain.[3] They are usually clinically benign but, in some cases, recurrence can occur many years following hysterectomy.[1] Little is known about metastasis of these tumors and, until March 2011, there was no case reporting lung metastasis and especially multiple pulmonary nodules and pleural effusion due to STUMP.
On the other hand, “benign metastasizing leiomyomas” is a clinicopathologic condition where pathologically benign smooth muscle neoplasms derived from uterine leiomyomas metastasize to extrauterine sites, like lung, pelvic lymph nodes or abdomen surfaces.[4]
CASE REPORT
A case of a 51-year-old woman, gravida 0 - para 0, who was admitted with progressive dyspnea on exertion is presented. The past medical history revealed that 3 years ago and due to persisting menorrhagia, the patient underwent dilatation and curettage. Histopathology report indicated the presence of abnormal endometrial hyperplasia. As the symptoms were persisting, the woman underwent total abdominal hysterectomy. Histopathologically, after thorough gross processing of the specimen, an intramural smooth muscle tumor of the uterus with a diameter measuring 5 cm was identified and six (6) sections from the tumor were obtained. Microscopy showed mild mitotic activity (2–6 MF/10 HPF), moderate nuclear atypia and lack of tumor necrosis [Figure 1]. A second typical leiomyoma, adenomyosis and sparse areas of thin-walled arteriolar type (plexiform) vessels were also identified but with no typical indication of endometrial malignancy present. Immunohistochemistry revealed focally mild immunopositivity regarding Vimentin and CD10. Extensive sampling was done to exclude the possibility of leiomyosarcoma. The absence of necrosis and atypical mitosis made pathologists consider that the tumor belongs to the so-called “grey zone” or STUMP. Therefore, no further treatment was applied and close follow-up was decided.
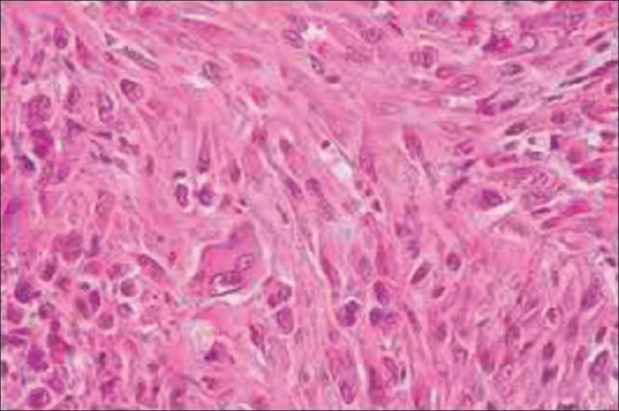
| Fig. 1 Uterine smooth muscle tumor with mild mitotic activity (smooth muscle tumors of uncertain malignant potential tumor)
Chest X-ray and chest computed tomography (CT) confirmed the presence of bilateral pulmonary nodules [Figure 2]. As multiple metastases due to tumor of unknown origin were suspected, the patient underwent a series of diagnostic tests: brain and abdomen CTs, gastroscopy, colonoscopy, bronchoscopy, mammography, thyroid ultrasound and skeletal scintigraphy, none of which indicated primary extrapulmonary tumor. The patient underwent video-assisted thoracoscopy and multiple lung biopsies were performed. Histopathology and immunohistochemical examination of the specimens showed pulmonary parenchyma with focuses of sarcoma. A metastatic malignant smooth muscle cells neoplasm with uterine origin was diagnosed [Figure 3]. Cell nuclei presented diffuse moderate mitotic activity (6 MF/10 HPF), but there were also some atypical mitoses. The immunohistochemical examination revealed that the tumor was positive in Desmin and smooth muscle actin (SMA) and negative in CD117 and CD34. Pleural fluid was also found positive for metastatic malignancy. Both pathology and cytopathology reports excluded that the condition was associated with benign metastasizing leiomyoma.
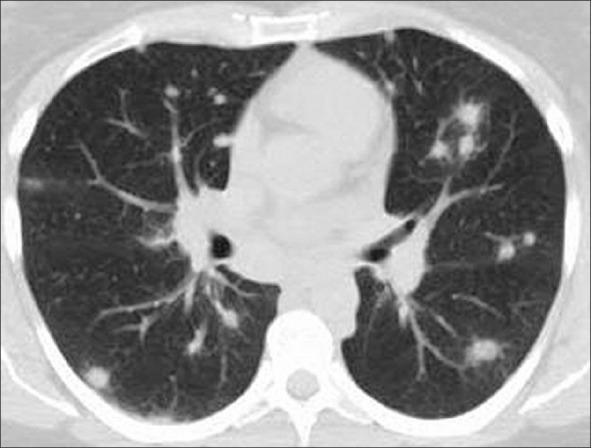
| Fig. 2 Chest computed tomography was consistent with multiple pulmonary nodules and pleural effusion
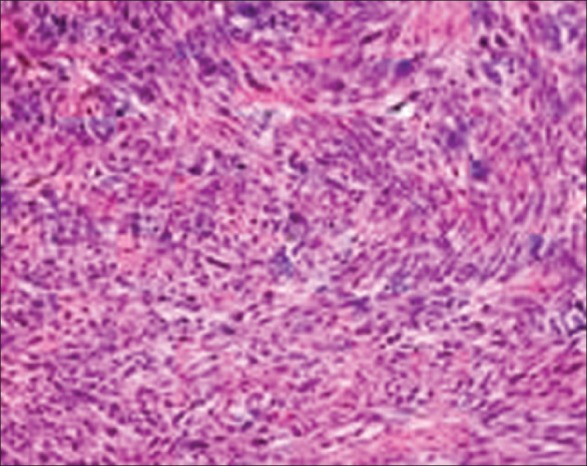
| Fig. 3 Pathology was consistent with a metastatic pulmonary leiomyosarcoma
The patient underwent 14 cycles of chemotherapy, with multiple drug combinations, including ifosfamide, epirubicin, docetaxel, gemcitabine, bevacizumab, cisplatin, cyclophosphamide and vincristine. She died 11 months later due to disease progression.
DISCUSSION
Leiomyomas are uterine mesenchymal benign tumors derived from smooth muscle cells. These tumors are the most common neoplasm of the uterus.[4] On the other hand, leiomyosarcomas are the most common type of uterine sarcomas, accounting for approximately 30% of them. They usually arise de novo and, only in rare cases, a leiomyoma can be transformed into leiomyosarcoma.[5] Differential diagnostic criteria distinguishing these tumors from benign myomas include coagulative cell necrosis, moderate to severe cytologic atypia and numerous mitotic figures.[4] Furthermore, “STUMP” cannot be classified as benign or malignant.[4] Some researchers described that this heterogeneous category of neoplasms contains more groups like “atypical leiomyomas with limited experience,” “smooth muscle tumor of low malignant potential,” “atypical leiomyoma with low risk of reccurence” and “mitotically active leiomyoma.”[1] “STUMP” diagnosis should be used sparingly and after a detailed clinical, histopathological and immunohistochemical examination.[6]
Hematogenous dissemination of uterine leiomyosarcomas is the most common pattern of spread, and lung metastasis occurs in more than half of the patients.[6] However, there is only one case reporting pleural effusion due to sarcoma of the uterine smooth muscle.[7] On the other hand, there is no data about the possible metastatic behavior of uterine “STUMP.”
In the case presented here, “STUMP” was the initial diagnosis of the uterine tumor. The possibility that the neoplasm was leiomyosarcoma cannot be excluded as the zone between the benign and malignant nature of STUMP is not clear. Also, the hypothesis that the metastatic lung focuses derived from malignant transformation of benign uterine metastasizing leiomyomas cannot be proved but seems to be extremely unlikely. However, all clinical, histopathological and immunohistochemical indications incline to the “STUMP” diagnosis. Furthermore, research on new immunohistochemical markers and histopathological characteristics could have some value in the diagnosis of problematic cases.
Finally, considering the unpredictable clinical behavior of “STUMP” and the fact that the malignant potential of some of them is substantial, patients should receive close and long-term follow-up. Metastasis cannot be excluded and, considering the pattern of metastatic spread of leiomyosarcomas, the lung could be the most common target organ. Clinical history, clinical outcome and treatment approach of these patients are uncertain. Prognosis cannot be determined due to the relative rarity of these tumors and the low experience on chemotherapy effect. However, when metastases occur, prognosis seems to be poor.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
REFERENCES
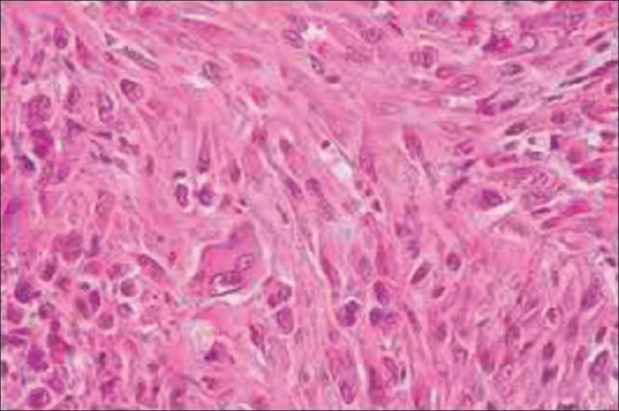
| Fig. 1 Uterine smooth muscle tumor with mild mitotic activity (smooth muscle tumors of uncertain malignant potential tumor)
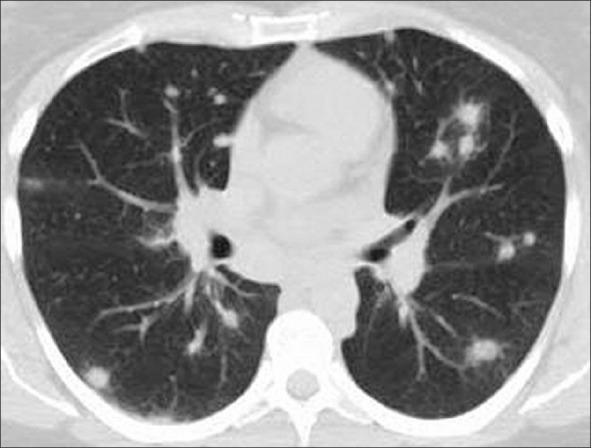
| Fig. 2 Chest computed tomography was consistent with multiple pulmonary nodules and pleural effusion
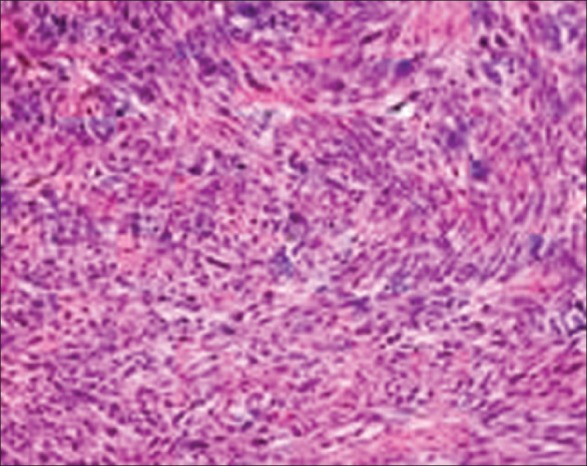
| Fig. 3 Pathology was consistent with a metastatic pulmonary leiomyosarcoma


 PDF
PDF  Views
Views  Share
Share

