Unusual Presentation of Wilms' Tumor as Umbilical Granuloma
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2018; 39(03): 413-414
DOI: DOI: 10.4103/ijmpo.ijmpo_245_17
Abstract
We report an unusual presentation of a Wilms' tumor in an 8-month-old child, incidentally detected by ultrasonography for an umbilical granuloma. A patent vitellointestinal duct anomaly required surgical excision in the same sitting as the nephroureterectomy. The case is reported for the unusual coexistence and the management implications.
Publication History
Article published online:
17 June 2021
© 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
We report an unusual presentation of a Wilms' tumor in an 8-month-old child, incidentally detected by ultrasonography for an umbilical granuloma. A patent vitellointestinal duct anomaly required surgical excision in the same sitting as the nephroureterectomy. The case is reported for the unusual coexistence and the management implications.
Introduction
Umbilical granuloma is common in infants and usually responds to common salt local application. It is to be borne in mind that not all umbilical lesions are granulomas and when not responding to treatment getting ultrasonography (USG) to rule out vitellointestinal duct (VID) or urachal anomalies is prudent.[1] In the index case, the USG also picked up a Wilms' tumor in the right kidney which has not been reported in literature previously.
Case Report
A full-term male child had a persistent red fleshy mass at the umbilicus not responding to local application of antibiotic ointment and silver nitrate. He was well with no complaints other than a minimal serosanguinous discharge from the umbilicus. At 7 months of age, he was referred for surgical excision of the umbilical mass. An USG of the abdomen done just before referral, however, picked up a large right renal tumor. A Wilms' tumor was diagnosed on fine-needle aspiration cytology at our center. Contrast-enhanced computed tomography of the abdomen revealed a 9 cm × 6 cm × 8 cm tumor arising from the lower pole of the right kidney [Figure 1]a. The tumor showed a significant reduction in size after four cycles of chemotherapy with Actinomycin D and vincristine. At laparotomy, a broad-based Meckel's diverticulum with a patent duct leading up to the umbilical granuloma [Figure 1]b was found. Wedge resection of the Meckel's diverticulum was done along with a right radical nephroureterectomy. The child had an uneventful postoperative period. Histopathology confirmed triphasic Wilms' tumor [Figure 2]. He is doing well at 6 months of follow-up.
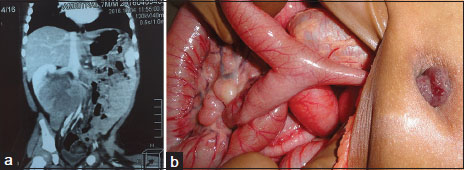
| Figure 1:(a) Contrast-enhanced computed tomography scan of the abdomen shows a large right renal tumor. (b) Intraoperative photograph of the umbilical granuloma connected with a patent vitellointestinal duct
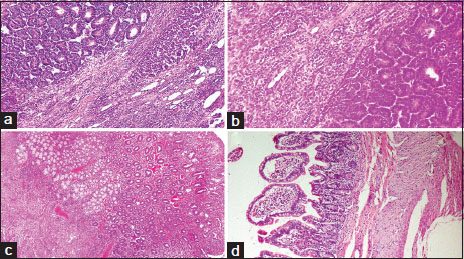
| Figure.2:Histopathological picture (H and E, ×200) shows (a) Part of renal tumor with epithelial and focal stromal component. (b) Blastemal components with focal stromal component. (c) Umbilical granuloma showing colonic mucosa with heterotopic Brunner’s glands in submucosa and (d) Diverticulum with small intestinal lining epithelium. No heterotropia was noted
Discussion
Wilms' tumor is the most common childhood abdominal malignancy forming 6% of all childhood cancers with a 5-year survival rate of nearly 90%.[2] Presenting features include abdominal mass, pain, hematuria, and fever. In the normal population, there is a 2% incidence of VID anomalies which may remain silent throughout life. The spectrum of anomalies includes fistula, sinus tract, cyst, mucosal remnants, and congenital bands. A study of 16 infants with VID revealed the most common presentation to be patent VID with visible bowel loop and/or fecal discharge with an umbilical granuloma seen only in 12.25% of patients.[3]
Intra-abdominal malignancy is known to cause umbilical deposits in adults, also called Sister Mary Joseph's nodule, secondary to spread through the lymphatics and venous channels draining along the abdominal wall.[4] This phenomenon is not known in children, and the umbilical mass, in this case, was soft and granulomatous as opposed to hard and skin covered. It would appear that the two conditions existed coincidentally but the persistence of the granuloma at 7 months age led to the USG detection of the VID and the renal tumor which could be excised in the same sitting without any additional morbidity.
Wilms' tumor is less frequent in infants but associated with a better prognosis.[5] Due to an association with favorable histology, they may be treated with surgical resection alone. Early detection is possible if frequent well-child check-ups are done in the 1st year of life. If our case did not have the associated granuloma, he may have presented later with metastasis. A literature search of surgical conditions that preceded the diagnosis of Wilms' tumor revealed only one report of a 5-year-old that presented with a perforated appendix and was detected to have a renal mass on imaging. The child underwent an appendectomy followed by an open biopsy of the renal mass which revealed Wilms' tumor.[6]
Conclusion
This is an unusual presentation of Wilms' tumor in an infant which has not been reported before. It is hoped that early management will improve the long-term outlook for this patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
References
- Sarwar U, Javed M, Wright T, Dawson A, Wilson-Jones N. These umbilical lesions weren't granulomas after all. J Fam Pract 2016; 65: E1-3
- Weirich A, Ludwig R, Graf N, Abel U, Leuschner I, Vujanic GM. et al. Survival in nephroblastoma treated according to the trial and study SIOP-9/GPOH with respect to relapse and morbidity. Ann Oncol 2004; 15: 808-20
- Kadian YS, Verma A, Rattan KN, Kajal P. Vitellointestinal duct anomalies in infancy. J Neonatal Surg 2016; 5: 30
- Larbcharoensub N, Pongtippan A, Pangpunyakulchai D, Phongkitkarun S, Lertsithichai P, Dejthevaporn TS. et al. Sister mary joseph nodule caused by metastatic desmoplastic small round cell tumor: A clinicopathological report. Mol Clin Oncol 2016; 5: 557-61
- Lamb MG, Aldrink JH, O'Brien SH, Sinha H, Arnold MA, Ranalli MA. et al. Renal tumors in children younger than 12 months of age: A 65-year single institution review. J Pediatr Hematol Oncol 2017; 39: 103-7
- Li A, Asch M, Lasky J, Sieger L, Lee SL. et al. Neonatal. Neonat 2012; 34: e193-4
Address for correspondence
Publication History
Article published online:
17 June 2021
© 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2,
Noida-201301 UP, India
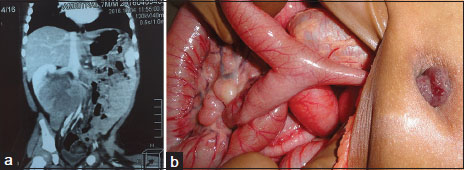
| Figure 1:(a) Contrast-enhanced computed tomography scan of the abdomen shows a large right renal tumor. (b) Intraoperative photograph of the umbilical granuloma connected with a patent vitellointestinal duct
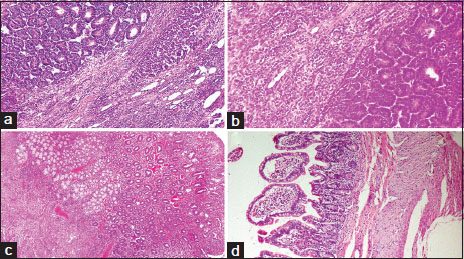
| Figure.2:Histopathological picture (H and E, ×200) shows (a) Part of renal tumor with epithelial and focal stromal component. (b) Blastemal components with focal stromal component. (c) Umbilical granuloma showing colonic mucosa with heterotopic Brunner’s glands in submucosa and (d) Diverticulum with small intestinal lining epithelium. No heterotropia was noted
References
- Sarwar U, Javed M, Wright T, Dawson A, Wilson-Jones N. These umbilical lesions weren't granulomas after all. J Fam Pract 2016; 65: E1-3
- Weirich A, Ludwig R, Graf N, Abel U, Leuschner I, Vujanic GM. et al. Survival in nephroblastoma treated according to the trial and study SIOP-9/GPOH with respect to relapse and morbidity. Ann Oncol 2004; 15: 808-20
- Kadian YS, Verma A, Rattan KN, Kajal P. Vitellointestinal duct anomalies in infancy. J Neonatal Surg 2016; 5: 30
- Larbcharoensub N, Pongtippan A, Pangpunyakulchai D, Phongkitkarun S, Lertsithichai P, Dejthevaporn TS. et al. Sister mary joseph nodule caused by metastatic desmoplastic small round cell tumor: A clinicopathological report. Mol Clin Oncol 2016; 5: 557-61
- Lamb MG, Aldrink JH, O'Brien SH, Sinha H, Arnold MA, Ranalli MA. et al. Renal tumors in children younger than 12 months of age: A 65-year single institution review. J Pediatr Hematol Oncol 2017; 39: 103-7
- Li A, Asch M, Lasky J, Sieger L, Lee SL. et al. Neonatal. Neonat 2012; 34: e193-4


 PDF
PDF  Views
Views  Share
Share

