Unilateral Vocal Cord Paralysis Secondary to Central Bronchogenic Carcinoma
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2018; 39(01): 91-92
DOI: DOI: 10.4103/ijmpo.ijmpo_170_16
Abstract
Vocal cord paralysis may arise from neurogenic paralysis or mechanical fixation. It is sometimes the only sign of an underlying disease. Thus, it is clinically important to diagnose the primary disease in cases of vocal cord paralysis because many of its potential causes, such as symptom-free malignant tumors, can be fatal or cause serious morbidity if detected late. Radiologic evaluation is often useful for determining the etiology of vocal cord paralysis.
Keywords
Aortopulmonary window - bronchogenic carcinoma - computed tomography - unilateral vocal cord paralysis
Publication History
23 June 2021
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Vocal cord paralysis may arise from neurogenic paralysis or mechanical fixation. It is sometimes the only sign of an underlying disease. Thus, it is clinically important to diagnose the primary disease in cases of vocal cord paralysis because many of its potential causes, such as symptom-free malignant tumors, can be fatal or cause serious morbidity if detected late. Radiologic evaluation is often useful for determining the etiology of vocal cord paralysis.
Keywords
Aortopulmonary window - bronchogenic carcinoma - computed tomography - unilateral vocal cord paralysisIntroduction
Lung cancer is the most common cancer in the world and a leading cause of death. Signs and symptoms of lung cancers may be due to the primary tumor, locoregional spread, metastatic disease, or ectopic hormone production. Symptoms due to locoregional spread can include superior vena cava obstruction, paralysis of the recurrent laryngeal nerve, and phrenic nerve palsy, causing hoarseness and paralysis of the diaphragm; pressure on the sympathetic plexus, causing Horner syndrome; dysphagia resulting from esophageal compression and pericardial effusion. Here, we see a case of left parahilar and upper lobe bronchogenic carcinoma causing ipsilateral vocal cord paralysis.
Description
A 61-year-old man with hoarseness of voice for 3 weeks to the ent outpatient department. Contrast-enhanced computed tomography (CT) of the neck and chest revealed an ill-defined heterogeneously enhancing soft tissue density lesion (HU 40) measuring 6.9 cm ? 6.2 cm ? 9.0 cm (AP ? ML ? CC) with spiculated margins involving the hila, apical, anterior, and superior lingular segments of the left lung [Figure 1] displaying loss of fat planes with the aortopulmonary window, descending aorta, anterior chest wall [Figure 2]. Paramedian position of the left vocal cord with dilated left pyriform sinus, laryngeal ventricle, and anteromedial deviation of the left arytenoid cartilage [Figure 3]. Compensation by the right vocal cord was present. Bilateral cervical and mediastinal lymphadenopathy were present. A diagnosis of central bronchogenic carcinoma causing secondary left-sided vocal cord paralysis was made.{Figure 1}{Figure 2}{Figure 3}

|?Figure.1Axial contrast enhanced computed tomography image in lung window demonstrating a mass lesion with spiculated margins in the left upper lobe with invasion in the aorticopulmonary window (arrow)
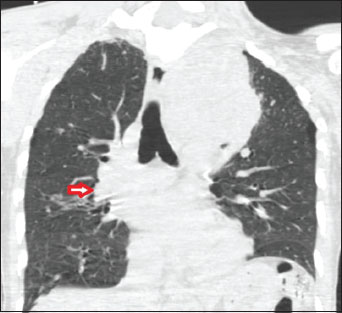
|?Figure.2A 61-year-old gentleman with a paralyzed right vocal cord. Coronal reformatted computed tomography image in lung window showing a large left parahilar and upper lobe malignant lesion. Right hilar lymphadenopathy is seen (arrow)
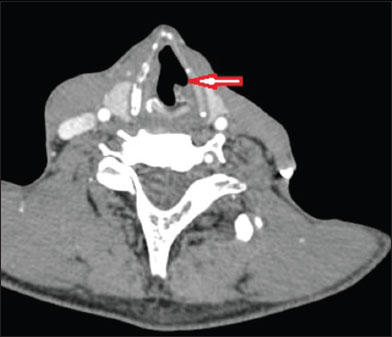
|?Figure.3Axial contrast enhanced computed tomography image of the neck at the level of vocal cords showing the paramedian position of the left vocal cord with dilated left pyriform sinus and laryngeal ventricle (arrow) suggesting left vocal cord paralysis
Discussion
The recurrent laryngeal nerves innervate the vocal cords. The right recurrent laryngeal nerve leaves the vagus nerve at the anterior surface of the right subclavian artery and runs inferiorly, looping around the subclavian artery, then ascends medially in the tracheoesophageal groove.[1] The left recurrent nerve branches more caudally from the vagus nerve on the anterior surface of the aortic arch. It passes inferiorly around the arch through the aortopulmonary window to ascend in the tracheoesophageal groove.[2] Both recurrent laryngeal nerves are intimately associated with the thyroid gland. In the thorax, the left recurrent laryngeal nerve is more vulnerable than the right because it pursues a longer intrathoracic course, coming into contact with the mediastinal surface of the left lung, continuing along the mediastinal lymph nodes, and finally looping around the aortic arch. Vocal cord paralysis has been reported to be about 1.4?2.5 times more frequent on the left side than on the right.[3] The CT scan is a very sensitive study for lesions in the neck and upper chest. Furthermore, it is now available at a moderate cost. In patients with lung carcinoma, the left recurrent laryngeal nerve is most frequently involved as it courses through the aortopulmonary window. Nevertheless, a chest CT scan was not routinely taken in this study. Caution should be taken when neck CT scans were taken for patients with right vocal cord paralysis to include an area of the skull base to the thoracic inlet, and for left vocal cord paralysis, to include the area up to the aortic triangle, most primary diseases in the chest were detectable.[4] Therefore, it might be cost-effective to scan down to the level of the aortic triangle when taking neck CT scans for vocal cord paralysis patients, regardless of the paralytic side.
Conflict of Interest
There are no conflicts of interest.
References
- Terris DJ, Arnstein DP, Nguyen HH.?Contemporary evaluation of unilateral vocal cord paralysis. Otolaryngol Head Neck Surg 1992; 107: 84-90
- Titche LL.?Causes of recurrent laryngeal nerve paralysis. Arch Otolaryngol 1976; 102: 259-61
- Chen HC, Jen YM, Wang CH, Lee JC, Lin YS.?Etiology of vocal cord paralysis. ORL J Otorhinolaryngol Relat Spec 2007; 69: 167-71
- Holinger LD, Holinger PC, Holinger PH.?Etiology of bilateral abductor vocal cord paralysis: A review of 389 cases. Ann Otol Rhinol Laryngol 1976; 85(4 Pt 1): 428-36
Address for correspondence
Publication History
23 June 2021
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor,
Sector 2, Noida-201301 UP, India

|?Figure.1Axial contrast enhanced computed tomography image in lung window demonstrating a mass lesion with spiculated margins in the left upper lobe with invasion in the aorticopulmonary window (arrow)
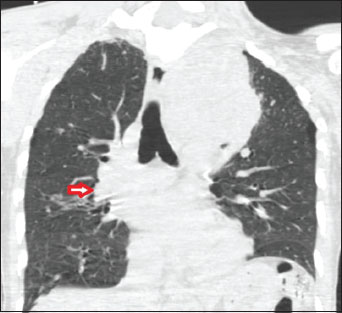
|?Figure.2A 61-year-old gentleman with a paralyzed right vocal cord. Coronal reformatted computed tomography image in lung window showing a large left parahilar and upper lobe malignant lesion. Right hilar lymphadenopathy is seen (arrow)
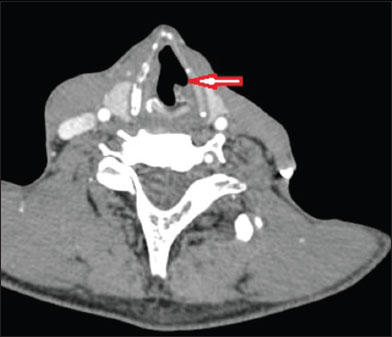
|?Figure.3Axial contrast enhanced computed tomography image of the neck at the level of vocal cords showing the paramedian position of the left vocal cord with dilated left pyriform sinus and laryngeal ventricle (arrow) suggesting left vocal cord paralysis
References
- Terris DJ, Arnstein DP, Nguyen HH.?Contemporary evaluation of unilateral vocal cord paralysis. Otolaryngol Head Neck Surg 1992; 107: 84-90
- Titche LL.?Causes of recurrent laryngeal nerve paralysis. Arch Otolaryngol 1976; 102: 259-61
- Chen HC, Jen YM, Wang CH, Lee JC, Lin YS.?Etiology of vocal cord paralysis. ORL J Otorhinolaryngol Relat Spec 2007; 69: 167-71
- Holinger LD, Holinger PC, Holinger PH.?Etiology of bilateral abductor vocal cord paralysis: A review of 389 cases. Ann Otol Rhinol Laryngol 1976; 85(4 Pt 1): 428-36


 PDF
PDF  Views
Views  Share
Share

