Unicystic Ameloblastoma of Mandible- Imaging Features: A Case Report and Literature Review
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(03): 401-405
DOI: DOI: 10.4103/ijmpo.ijmpo_140_18
Abstract
Ameloblastoma are benign tumors whose importance lies in its potential to grow into enormous size with resulting bone deformity. They are typically classified as unicystic, multicystic, peripheral, and malignant subtypes. Unicystic ameloblastoma (UA) refers to those cystic lesions that show clinical, radiographic, or gross features of an odontogenic cyst but on histological examination show a typical ameloblastomatous epithelium lining, with or without luminal and/or mural tumor growth. We present a very rare case of unicystic ameloblastoma in a girl child with an age of 10 years; clinical and radiographic features of UCA, its differential diagnosis, histopathology, and current concepts of management have also been discussed in the present paper.
Publication History
Received: 24 June 2018
Accepted: 29 December 2018
Article published online:
28 June 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Ameloblastoma are benign tumors whose importance lies in its potential to grow into enormous size with resulting bone deformity. They are typically classified as unicystic, multicystic, peripheral, and malignant subtypes. Unicystic ameloblastoma (UA) refers to those cystic lesions that show clinical, radiographic, or gross features of an odontogenic cyst but on histological examination show a typical ameloblastomatous epithelium lining, with or without luminal and/or mural tumor growth. We present a very rare case of unicystic ameloblastoma in a girl child with an age of 10 years; clinical and radiographic features of UCA, its differential diagnosis, histopathology, and current concepts of management have also been discussed in the present paper.
Introduction
Ameloblastoma is the most common benign odontogenic tumor accounting for approximately 1%-of tumors and cysts of the jaw and 10%-of all the odontogenic tumors.[1] It is a slow-growing, persistent, and locally aggressive neoplasm that may originate from the epithelium involved with the formation of teeth such as enamel organ, odontogenic rests of Malassez, reduced enamel epithelium, and odontogenic cyst lining.[2]
Ameloblastoma may occur centrally within the bone or peripherally, without an intraosseous component in the soft tissues overlying the alveolar ridge. Intraosseous lesions are of two types solid/conventional/multicystic and unicystic.[3] Unicystic ameloblastoma (UA), a variant of ameloblastoma first described by Robinson and Martinez[4] in 1977, refers to those cystic lesions that show clinical and radiologic characteristics of an odontogenic cyst but in histologic examination show a typical ameloblastomatous epithelium lining part of the cyst cavity with or without luminal and/or mural tumor proliferation. Before the report by Robinson and Martinez, this variant had been referred to as a mural or intraluminal ameloblastoma. Recognition of this growth pattern is very important because of its unicystic radiographic appearance, histologic findings, association with an unerupted tooth, occurrence in the mandible of younger patients, and a recurrence rate after conservative surgical treatment lower than that of its conventional counterpart.[5]
We present a case of a unicystic ameloblastoma in a 10-year-old child patient who reported with a complaint of swelling of her right lower jaw.
Case Report
A 10-year-old female child came with a complaint of swelling on the right lower side of her jaw for 1 month which was insidious in onset and got gradually progressed to the present size. It was associated with severe, intermittent, and dragging type of pain which radiates to the right ear. Pain relieved with medication. It was also associated with extraoral swelling for 15 days. On extraoral examination, facial asymmetry was seen in the right lower third of the face. On intraoral examination, a solitary diffuse swelling was seen in the buccal vestibular region of 85 and 46, extending anteroposteriorly from middle third of 85 to distal surface of 46. Superiorly the swelling of the lesion is extending from attached gingiva of 85 and 46 to inferiorly into the buccal vestibule. Sinus opening with pus discharge was seen on the attached gingiva of 85 (buccal or lingual). On palpation, swelling was tender, hard in consistency, noncompressible, and nonreducible. Expansion of buccal cortical plate was felt in relation to 85 and 46.
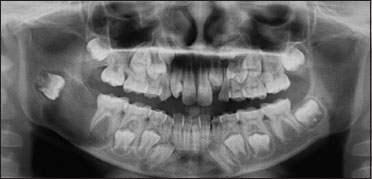
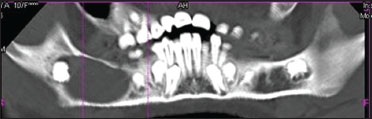
Based on the history and clinical examination, a provisional diagnosis of ameloblastoma was made. Under differential diagnosis, ameloblastic fibroma and odontogenic keratocyst were considered. Intaoral periapical view (IOPA), occlusal view,orthopantomogram (OPG), and computed tomography (CT) scan were taken. IOPA taken in relation to 85 and 46 [Figure 1] showed diffuse radiolucency distal to 46 with the absence of 47 tooth bud. OPG [Figure 2] view showed a solitary, well-defined radiolucency of size 3 cm × 2 cm extending anteroposteriorly from mesial root of the tooth number 46 is 1 cm from the posterior border of the ramus of the mandible, superoinferiorly 1 cm below the sigmoid notch, to the inferior border of the mandible thinning the inferior cortical margin. Internal structure was radiolucent with the displaced tooth bud of 47 in the ramus region.

| Figure 1:Intraoral periapical radiograph showing diffuse radiolucency distal to 46 with the absence of 47 tooth bud
| Figure.2:Preoperative orthopantomogram showing solitary, well‑defined radiolucency of size 3 cm × 2 cm surrounding the crown of 47 tooth bud which got displaced into the ramus region with thinning of the inferior border of the mandible
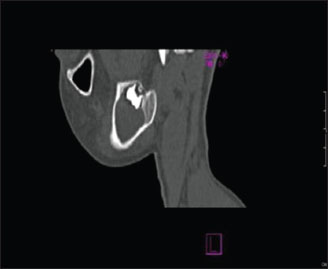
Panoramic CT section [Figure 3] and sagittal CT section [Figure 4] showed hypodense area of size 2.5 cm × 3 cm surrounding the developing tooth bud of 47. Axial CT section [Figure 5]a showed tooth within the hypodense area, and axial CT section [Figure 5]b showed buccal cortical plate expansion with breakdown of lingual cortical plate.
| Figure.3:Panoramic computed tomography section showing complete extension of the lesion
| Figure.4:Sagittal computed tomography section showing hypodense area surrounding the developing tooth bud of 47

| Figure.5:(a) Axial computed tomography section showing tooth within the hypodense area (b) Axial computed tomography section showing buccal cortical plate expansion with breakdown of lingual cortical plate
An incisional biopsy was done and it showed epithelial lining with ameloblast-like cells and adjacent connective tissue stroma. There was no luminal proliferation of epithelium, suggestive of intraluminal ameloblastoma [Figure 6]. Following the diagnosis, the parents were informed about the condition and proposed treatment. Surgical enucleation along with chemical cauterization with Carnoy's solution [Figure 7] was done under general anesthesia along with extraction of 47 [Figure 8] considering age of the patient. The patient is under follow-up, with no functional or esthetic complaints. Six months posttreatment, OPG shows signs of new bone formation [Figure 9].

| Figure.6:Low-power histopathological picture of unicystic ameloblastoma showing intraluminal proliferation

| Figure.7:Surgical site of enucleation

| Figure.8:Surgical specimen with extracted 47

| Figure.9:Postoperative orthopantomogram showing signs of new bone formation
Discussion
UA accounts for 6%–15%-of all intraosseous ameloblastomas.[1] It is less aggressive and usually occurs in an earlier age group than the solid or multicystic with about 50%-of the cases occurring in the second decade of life. As in the present case, >90%-of UA are seen affecting the mandibular region,[6] which was also seen in present case. In most cases, UA are associated with impacted tooth, mandibular third molar being the most common.[7]
The term unicystic is derived from the macroscopic and microscopic appearance, the lesion being essentially a well-defined, often large monocystic cavity with a lining, focally but rarely entirely composed of odontogenic (ameloblastomatous) epithelium.[8]
The pathogenesis of cystic ameloblastomas remains obscure. Some investigators believe that UA arises from preexisting odontogenic cysts, in particular a dentigerous cyst, while others maintain that it arises de novo. The reason why some ameloblastomas become completely cystic may be related to epithelial dysadhesion (e.g., defective desmosomes) or, more likely, to the intrinsic production of proteinases enzymes that normally degrade the central zone of the enamel organ after tooth development.[9] (e.g., metalloproteinases and serine proteinases).[9]
Radiographically, the unilocular: multilocular ratio is 13:3 when the lesion is associated with an impacted tooth. For the “nondentigerous” variant, this ratio changes to 8:7. Further, the “dentigerous” type occurs on average 8 years earlier than the “nondentigerous” variant. Finally, the mean age for unilocular, impaction-associated UAs is 22 years, whereas the mean age for the multilocular lesion unrelated to an impacted tooth is 33 years.[7]
Ackermann et al.[10] classified unicystic ameloblastoma into three types with prognostic and therapeutic implications such as:
-
Group I: Luminal UA (tumor confined to the luminal surface of the cyst)
-
Group II: Intraluminal/plexiform UA (nodular proliferation into the lumen without infiltration of tumor cells into the connective tissue wall)
-
Group III: Mural (invasive islands of ameloblastomatous epithelium in the connective tissue wall not involving the entire epithelium).
The microscopic pattern that exhibits mural invasion in UA suggests a more aggressive potential.[11]
Another histologic subgrouping by Philipsen and Reichart[12] has also been described as follows:
-
Subgroup 1: Luminal
-
Subgroup 1.2: Luminal and intraluminal
-
Subgroup 1.2.3: Luminal, intraluminal, and intramural
-
Subgroup 1.3: Luminal and intramural.
The unicystic ameloblastomas diagnosed as subgroups 1 and 1.2 can be treated conservatively (enucleation), whereas subgroups 1.2.3 and 1.3 showing intramural growths require radical resection, as for a solid or multicystic ameloblastoma. Following enucleation, vigorous curettage of the bone should be avoided as it may implant foci of ameloblastoma deeper into bone. Chemical cauterization with Carnoy's solution[13] is also advocated for subgroups 1 and 1.2. Subgroups 1.2.3 and 1.3 have a high risk for recurrence, requiring more aggressive surgical procedures.[14]
Recurrence rates for unicystic ameloblastoma after conservative surgical treatment (curettage or enucleation) are generally reported to be <25 href="https://www.thieme-connect.com/products/ejournals/html/10.4103/ijmpo.ijmpo_140_18#JR_15" xss=removed>15] Recurrence rates for solid multicystic ameloblastoma was found to be about 50%–90%.
The present analysis included only publications in English. All well-documented publications during the last 20 years were collected, and several clinicopathological features of each case were studied. The following data were recorded: age (≤10 years), sex, location, clinical features/symptoms, histological type, radiographic appearance, and treatment. Only reports of unicystic ameloblastoma in children <10 href="https://www.thieme-connect.com/products/ejournals/html/10.4103/ijmpo.ijmpo_140_18#TB_1" xss=removed>Table 1].
|
Year |
Author |
Age |
Sex |
Location |
Clinical features |
Histological features |
Radiological features |
Treatment |
|---|---|---|---|---|---|---|---|---|
|
INA – Information not available; UL – Unilocular ameloblastoma |
||||||||
|
1998 |
Li etal.[16] |
10 |
Female |
Mandible |
Mild fullness over the cheek |
Unicystic ameloblastoma |
UL |
Enucleation |
|
2000 |
Li etal.[17] |
5 |
Male |
Maxilla (premolar to second molar) |
Cystic lesion |
Mural type |
INA |
Enucleation |
|
2003 |
Al-Khateeb and Ababneh[18] |
9 |
Female |
Mandible |
Painless swelling |
Unicystic ameloblastoma |
UL |
Enucleation plus peripheral ostectomy |
|
2007 |
Huang et al.[19] |
9 |
Male |
Body-angle of INA the mandible |
INA |
UL |
Enucleation and peripheral ostectomy |
|
|
2008 |
Qureshi et al.[20] |
10 |
Female |
Mandible |
Mild fullness over the cheek |
Unicystic ameloblastoma |
UL |
Enucleation, curettage |
|
2008 |
Gulten et al.[21] |
8 |
Male |
Right mandible |
Painless hard swelling |
Unicystic ameloblastoma |
UL |
Enucleation and extraction of related teeth |
|
2011 |
Chacko and Kuriakose[22] |
9 |
Male |
Mandible |
Pain and swelling in relation to the right side of the lower jaw |
Plexiform unicystic ameloblastoma |
UL |
Enucleation, curettage |
|
2011 |
Kalaskar et al.[23] |
9 |
Male |
Right maxilla |
Painless swelling |
Unicystic ameloblastoma with intraluminal proliferations |
UL |
Enucleation + Carnoy’s solution and extraction of related teeth |
|
2011 |
Ponniah[24] |
8 |
Female |
Left ramus of the mandible |
Painless swelling on the left side of the mandible |
Unicystic ameloblastoma |
UL |
Enucleation then segmental resection |
|
2011 |
Sudhakara Reddy et al.[25] |
6 |
Female |
Anterior mandible |
Slow growing painless swelling |
Unicystic ameloblastoma |
UL |
Enucleation and extraction of related teeth followed by application of Carnoy’s solution |
|
2012 |
Scariot et al.[26] |
9 |
Female |
Right mandibular body |
Painless swelling |
Plexiform unicystic ameloblastoma |
UL |
Curettage with extraction of two adjacent teeth |
|
2013 |
Bhutia et al.[27] |
5 |
Male |
Right mandible |
painless hard swelling |
Type 1 unicystic ameloblastoma |
UL |
Enucleation of the cyst with extraction of the involved teeth followed by application of Carnoy’s solution |
|
2013 |
Arora et al.[28] |
3 |
Female |
Left maxilla |
Bony hard swelling |
Unicystic ameloblastoma (Type 1.2) |
UL |
Enucleation of the cyst with extraction of the involved teeth |
|
2014 |
Present case |
10 |
Female |
Right mandible |
Swelling with mild pain |
Unicystic ameloblastoma |
UL |
Enucleation with chemical cauterization |

| Figure 1:Intraoral periapical radiograph showing diffuse radiolucency distal to 46 with the absence of 47 tooth bud
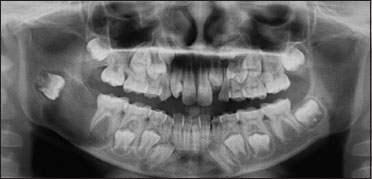
| Figure.2:Preoperative orthopantomogram showing solitary, well‑defined radiolucency of size 3 cm × 2 cm surrounding the crown of 47 tooth bud which got displaced into the ramus region with thinning of the inferior border of the mandible
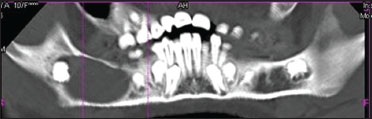
| Figure.3:Panoramic computed tomography section showing complete extension of the lesion
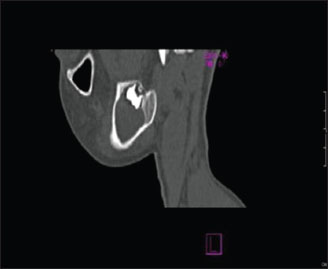
| Figure.4:Sagittal computed tomography section showing hypodense area surrounding the developing tooth bud of 47

| Figure.5:(a) Axial computed tomography section showing tooth within the hypodense area (b) Axial computed tomography section showing buccal cortical plate expansion with breakdown of lingual cortical plate

| Figure.6:Low-power histopathological picture of unicystic ameloblastoma showing intraluminal proliferation

| Figure.7:Surgical site of enucleation

| Figure.8:Surgical specimen with extracted 47

| Figure.9:Postoperative orthopantomogram showing signs of new bone formation
References
- Olaitan AA, Adekeye EO. Clinical features and management of ameloblastoma of the mandible in children and adolescents. Br J Oral Maxillofac Surg 1996; 34: 248-51
- Gerzenshtein J, Zhang F, Caplan J, Anand V, Lineaweaver W. Immediate mandibular reconstruction with microsurgical fibula flap transfer following wide resection for ameloblastoma. J Craniofac Surg 2006; 17: 178-82
- Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: Biological profile of 3677 cases. Eur J Cancer B Oral Oncol 1995; 31B: 86-99
- Robinson L, Martinez MG. Unicystic ameloblastoma: A prognostically distinct entity. Cancer 1977; 40: 2278-85
- Gardner DG, Corio RL. The relationship of plexiform unicystic ameloblastoma to conventional ameloblastoma. Oral Surg Oral Med Oral Pathol 1983; 56: 54-60
- Pizer ME, Page DG, Svirsky JA. Thirteen-year follow-up of large recurrent unicystic ameloblastoma of the mandible in a 15-year-old boy. J Oral Maxillofac Surg 2002; 60: 211-5
- Philipsen HP, Reichart PA. Unicystic ameloblastoma. A review of 193 cases from the literature. Oral Oncol 1998; 34: 317-25
- Kessler HP. Intraosseous ameloblastoma. Oral Maxillofac Surg Clin North Am 2004; 16: 309-22
- Rosenstein T, Pogrel MA, Smith RA, Regezi JA. Cystic ameloblastoma – Behavior and treatment of 21 cases. J Oral Maxillofac Surg 2001; 59: 1311-6
- Ackermann GL, Altini M, Shear M. The unicystic ameloblastoma: A clinicopathological study of 57 cases. J Oral Pathol 1988; 17: 541-6
- Ord RA, Blanchaert RHJr, Nikitakis NG, Sauk JJ. Ameloblastoma in children. J Oral Maxillofac Surg 2002; 60: 762-70
- Philpsen HP, Reichert PA. Unicystic Ameloblastoa. In: Odontogenic Tumors and Allied Lesions. London: Quintessence Pub. Co., Ltd; 2004. p. 77-86
- Lee PK, Samman N, Ng IO. Unicystic ameloblastoma – Use of Carnoy's solution after enucleation. Int J Oral Maxillofac Surg 2004; 33: 263-7
- Ramesh RS, Manjunath S, Ustad TH, Pais S, Shivakumar K. Unicystic ameloblastoma of the mandible – An unusual case report and review of literature. Head Neck Oncol 2010; 2: 1
- Gardner DG, Corio RL. Plexiform unicystic ameloblastoma. A variant of ameloblastoma with a low-recurrence rate after enucleation. Cancer 1984; 53: 1730-5
- Li TJ, Kitano M, Arimura K, Sugihara K. Recurrence of unicystic ameloblastoma: A case report and review of the literature. Arch Pathol Lab Med 1998; 122: 371-4
- Li TJ, Wu YT, Yu SF, Yu GY. Unicystic ameloblastoma: A clinicopathologic study of 33 Chinese patients. Am J Surg Pathol 2000; 24: 1385-92
- Al-Khateeb T, Ababneh KT. Ameloblastoma in young Jordanians: A review of the clinicopathologic features and treatment of 10 cases. J Oral Maxillofac Surg 2003; 61: 13-8
- Huang IY, Lai ST, Chen CH, Chen CM, Wu CW, Shen YH. Surgical management of ameloblastoma in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: 478-85
- Qureshi SS, Qureshi SS, Medhi SS, Kane SV. Unicystic ameloblastoma of the mandible masquerading as carcinoma of the oral cavity in a 10-year-old girl. Am J Surg 2008; 196: e7 -9
- Gulten U, Vedat T, Hilal A, Sarin YK. Unicystic ameloblastoma in 8 years old child: A case report review of unicystic ameloblastoma. Int Dent Med Disord 2008; 1: 29-33
- Chacko V, Kuriakose S. Conservative management of a case of plexiform ameloblastoma. Dent Update 2011; 38: 336-8
- Kalaskar R, Unawane AS, Kalaskar AE, Pandilwar P. Conservative management of unicystic ameloblastoma in a young child: Report of two cases. Contemp Clin Dent 2011; 2: 359-63
- Ponniah I. Recurrent unicystic ameloblastoma in a child. J Oral Maxillofac Pathol 2011; 15: 236-8
- Sudhakara ReddyK, Girish RaoS. Unicystic ameloblastoma in 6-year-old child and its significance. World J Dent 2011; 2: 363-6
- Scariot R, da Silva RV, da Silva Felix WJr, da Costa DJ, Rebellato NL. Conservative treatment of ameloblastoma in child: A case report. Stomatologija 2012; 14: 33-6
- Bhutia O, Roychoudhury A, Arora A, Mallick S. Management of unicystic ameloblastoma of the mandible in a 5-year old child. Natl J Maxillofac Surg 2013; 4: 232-4
- Arora S, Kumar S, Urs AB, Augustine J. Unicystic ameloblastoma in 3 year old paediatric patient – A rare entity. J Clin Exp Dent 2013; 5: e54-7


 PDF
PDF  Views
Views  Share
Share

