Tobacco-related knowledge, attitudes, and practices among urban low socioeconomic women in Mumbai, India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2015; 36(01): 32-37
DOI: DOI: 10.4103/0971-5851.151777
Abstract
Context: Tobacco use is an important health issue globally. It is responsible for a large number of diseases and deaths in India. Female tobacco users have additional health risks. Aims: The aim was to assess changes in pre and post-intervention tobacco-related knowledge, attitudes, and practices among women from urban low socioeconomic strata, after three rounds of interventions. Subjects and Methods: A structured questionnaire was used to interview women living in low socioeconomic housing clusters in Mumbai, regarding their tobacco consumption, attitudes, and practices, by Medical Social Workers. These data were entered into IBM SPSS Statistics, version 20 and analysed. Interventions for tobacco cessation were provided 3 times over a span of 9 months, comprising of health education and counseling. Post-intervention questionnaire was introduced at 12 months. Results: There was statistically significant improvement in the knowledge of women, following the interventions, with particular reference to poor oral hygiene and tobacco use being main cause of oral cancer (P = 0.007), knowledge of ill effects of second hand smoke (P = 0.0001), knowledge about possibility of early detection of oral cancer (P = 0.0001), perception of pictorial and written warnings on tobacco products (P = 0.0001), and availability of help for quitting tobacco (P = 0.024). Conclusion: The prevalence of smokeless tobacco use is very high among urban women from lower socioeconomic strata. Therefore, tobacco awareness programs and tobacco cessation services tailor made for this group of women must be planned and implemented.
Publication History
Article published online:
12 July 2021
© 2015. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Context:
Tobacco use is an important health issue globally. It is responsible for a large number of diseases and deaths in India. Female tobacco users have additional health risks.
Aims:
The aim was to assess changes in pre and post-intervention tobacco-related knowledge, attitudes, and practices among women from urban low socioeconomic strata, after three rounds of interventions.
Subjects and Methods:
A structured questionnaire was used to interview women living in low socioeconomic housing clusters in Mumbai, regarding their tobacco consumption, attitudes, and practices, by Medical Social Workers. These data were entered into IBM SPSS Statistics, version 20 and analysed. Interventions for tobacco cessation were provided 3 times over a span of 9 months, comprising of health education and counseling. Post-intervention questionnaire was introduced at 12 months.
Results:
There was statistically significant improvement in the knowledge of women, following the interventions, with particular reference to poor oral hygiene and tobacco use being main cause of oral cancer (P = 0.007), knowledge of ill effects of second hand smoke (P = 0.0001), knowledge about possibility of early detection of oral cancer (P = 0.0001), perception of pictorial and written warnings on tobacco products (P = 0.0001), and availability of help for quitting tobacco (P = 0.024).
Conclusion:
The prevalence of smokeless tobacco use is very high among urban women from lower socioeconomic strata. Therefore, tobacco awareness programs and tobacco cessation services tailor made for this group of women must be planned and implemented.
INTRODUCTION
Tobacco use is an emerging serious health concern globally. There were 6 million deaths worldwide, attributed to tobacco use, in the year 2011. [1] In India, tobacco has been responsible for 0.8-0.9 million deaths annually. [2]
Tobacco use is a risk factor for several illnesses affecting almost every organ of the human body. Female tobacco users bear additional health risks. They need to be specifically protected, as the tobacco industry is targeting women for initiating the tobacco habit. [1,3] Women generally do not recognize health as a felt need and the other day to day matters take priority.
SUBJECTS AND METHODS
This tobacco control program was implemented in Trombay, an urban slum in Mumbai. This was also one of the project clusters where our group had recently implemented a cancer screening program for women. During this former program, we had enlisted and enrolled women using any form of tobacco for oral cancer screening. We obtained this list and enrolled only the current tobacco users in the present program. Current tobacco users were defined as women using tobacco at the time of enrollment or having used tobacco within 6 months prior to enrollment in the former program. Accordingly, 340 women were identified as current tobacco users. Amongst these, 25 women could not be contacted as they had shifted their residence outside of the project cluster. Furthermore, 36 women had quit tobacco due to the health awareness created during the former program. Thus, overall 279 women were eligible as current tobacco users for the present tobacco cessation program. Among these, 260 women were available for post-intervention follow-up at the end of 1-year.
The Medical Social Workers (MSWs) went to the house of each eligible woman, explained the program, and invited them to participate. A written informed consent was administered in local language. The women, who agreed to participate, signed or put their left thumb impression on the consent form. Another woman/family member from the same area was invited to witness the procedure and signed as a witness. These women were then enrolled as participant women in the current program.
Meetings were held with the local community leaders to explain the program and their help was garnered in the various program activities. They made available premises within the community where this program could be conducted. These premises were well known and easily accessible for the women. They also appealed the community women to actively participate in the tobacco cessation program. The MSWs went to the house of participant women and personally interviewed them to record their pre-intervention details on a questionnaire [Figure 1]. This included particulars of their tobacco habits, knowledge of cancer, attitudes toward quitting tobacco and any efforts for the same. Women were then invited at a community camp place for group intervention. We involved the family members to encourage the eligible women to participate in the program.
.jpg)
| Fig. 1 Personal interviews being conducted at the house of participant woman to collect the pre-intervention data
The women in Trombay are predominantly housewives or engaged in part-time occupation of selling fish. Hence, most of the participant women were available for the counseling interventions. Throughout the program, all efforts were made to maximize compliance. In the case of nonavailability of participant women, multiple visits were made to their houses to contact and invite them to participate in the program activities.
The objectives of the study were to assess the knowledge, attitudes, and practices (KAP) of tobacco among women tobacco users residing in urban slums, provide tobacco cessation interventions at the community level enabling them to quit tobacco, identify factors associated with quitting and to evaluate the quit rates at the end of the program. The program was implemented as three intervention sessions spread over 9 months period followed by a post-intervention follow-up conducted at the end of 1-year to assess the changes in knowledge, attitudes and tobacco practices. The interventions included games, health education, and group counseling motivating people to quit tobacco and enabling them to cope with the challenges of quitting. Details of tobacco habits were recorded at each intervention. This paper presents the results with relation to the KAP among the tobacco users and its association with various sociodemographic factors. The details of the tobacco cessation interventions and the related outcomes in the form of tobacco quit rates are presented in another paper which will be soon published. This program has received institutional IRB approval and is registered with ClinicalTrials.gov.
RESULTS
The results related to KAP of tobacco, common cancers among women in India and the impact of the interventions on KAP are discussed here.
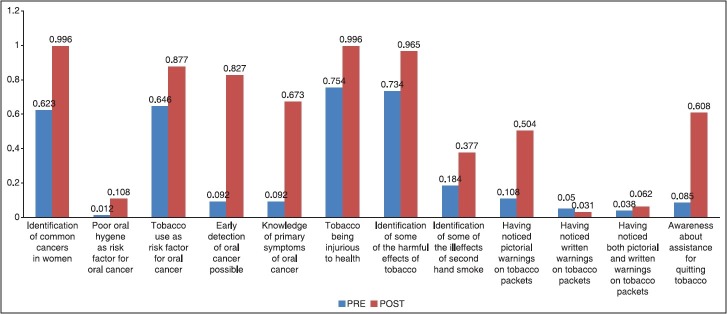
During the pre-intervention period, majority of women (66.53%) identified cancer as an important health hazard of tobacco. There was improvement in the post-intervention knowledge with regards to all the parameters as compared to the pre-intervention period [Figure 2]. Intervention in the form of health education was provided to the tobacco users. As reflected in Figure 2, the tobacco users even in pre-intervention period had a high level of awareness (75.40%) about it being dangerous to health. This further improved with the educational intervention to 99.60% in the post-intervention period. However, there was statistically significant improvement in the knowledge of women with regards to certain parameters like poor oral hygiene and tobacco use being the main cause of oral cancer (P = 0.007), knowledge of ill effects of second hand smoke (P = 0.0001), knowledge about possibility of early detection of oral cancer (P = 0.0001), perception of pictorial and written warnings on tobacco products (P = 0.0001), and availability of help for quitting tobacco (P = 0.024).
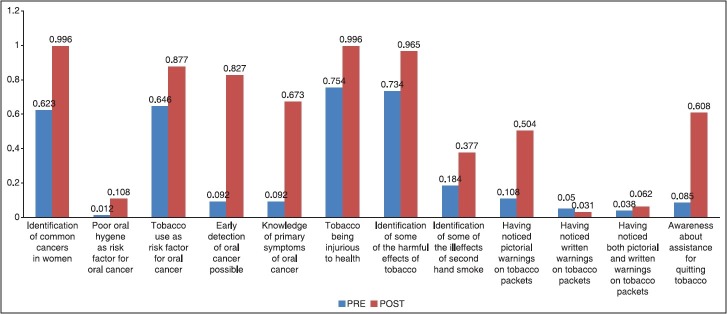
| Fig. 2 Comparison of pre and post-intervention knowledge and attitudes about tobacco among women
Women had mainly seen pictorial warnings in the form of pictures of “Scorpio” and written warnings of “Tobacco is harmful” on tobacco products. Women interpreted these as tobacco being harmful to health. Only 7.30% of the women felt health warnings on tobacco products would prevent people from using tobacco. Most women (68.46%) expressed that they gained knowledge of tobacco being injurious to health from the general public and 17.69% women reported to have obtained this information through media and other hoardings.
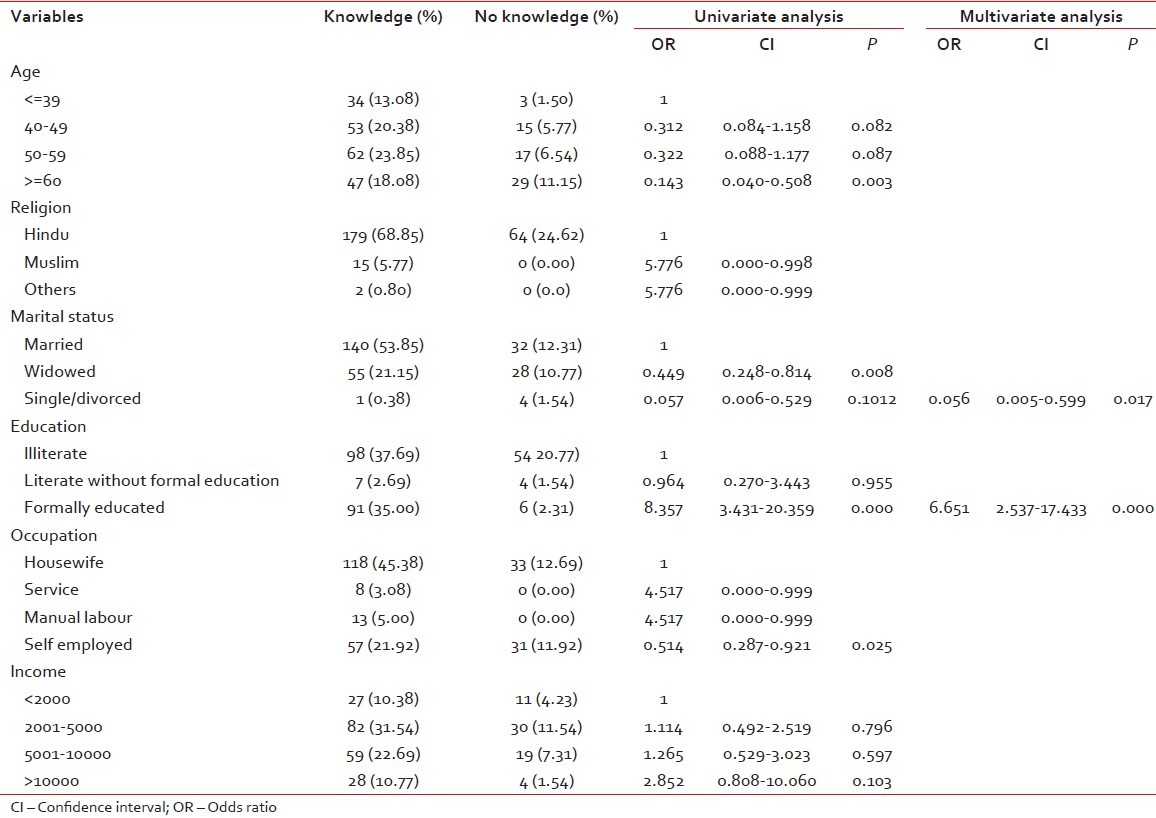
Univariate and multivariate logistic regression analysis [Table 1] were conducted to identify the relation of different socio-demographic variables with knowledge of tobacco being injurious to health. The following variables, that is, age, religion, marital status, education, occupation, and income were used in the analysis. According to the results of univariate analysis age, marital status, education, and occupation were significant and hence were included in multivariate analysis. According to the results of multivariate logistic regression analysis, only marital status and education were significantly related to the knowledge about tobacco being injurious to health. The married women had better knowledge than widowed women, and the formally educated women had better knowledge as compared to women who were illiterate and without formal education about tobacco being injurious to health.
Table 1
Univariate and multivariate logistic regression analysis identifying the relation of different sociodemographic factors with knowledge of tobacco being injurious to health
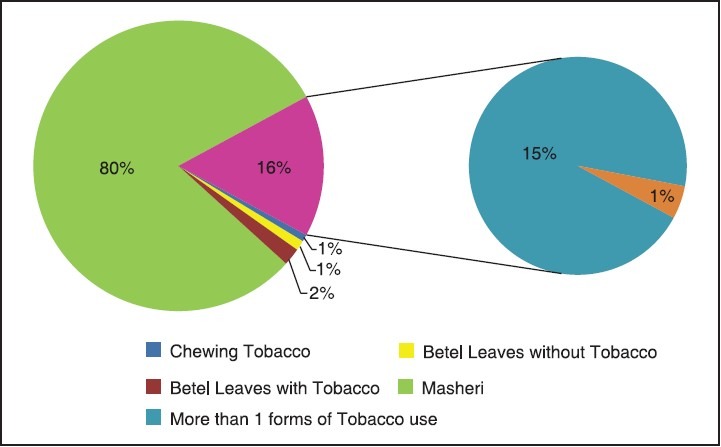
All participants in this program (279) used smokeless forms of tobacco. Only two participant women smoked beedis in addition to using smokeless tobacco. The distribution of use of different forms of tobacco is as shown in Figure 3. Among smokeless tobacco users, majority (94.23%) used masheri – burnt tobacco powder used to clean teeth (80.38% of the women used only masheri, while the rest used it in combination with other forms of tobacco). The frequency of masheri use was 1 to 3 times/day for majority (76.3%) of the participants. The median age of starting masheri was 15 years (range: 4-70) and the median duration of using the same was 35 years (range: 1-72). Most women (88.84%) used tobacco within half an hour of getting up in the morning. When asked regarding willingness to quit tobacco habits, majority (78.46%) women expressed their desire to do so. Majority of the women (61.92%) felt it was not difficult to quit tobacco.
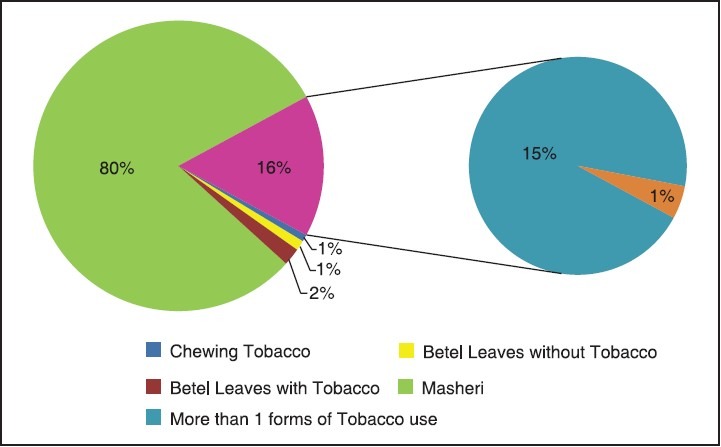
| Fig. 3 Patterns of tobacco use
DISCUSSION
This study focuses on the KAP related to tobacco use and the impact of the interventions on KAP among women in urban low socioeconomic strata in Mumbai, India. During the pre-intervention phase, majority women in our study (66.53%), reported cancer as a health hazard of tobacco. Another study from rural Kerala has reported similar findings. [4] At pre-intervention, 49.6%, 35.8%, and 47.3% of the participant women could correctly identify cancers of the breast, cervix, and oral cavity as common cancers among women in India. 73.8%, 27.0%, and 1.1% participant women from Delhi study identified breast, cervix, and oral cavity as common cancers among women. [5] Very few women identified poor oral hygiene as a risk factor for oral cancer. This is in contrast to another study from Kerala, wherein 42% of the participants mentioned bad oral hygiene as a risk factor for oral cancer. Majority of the women participating in this program (64.61%) were aware about tobacco being the main cause of oral cancer. In the Kerala study, more than 70% of the women attributed smoking as the cause of oral cancer. [6] Few women in the present study, that is, only 9.23% of the respondents, were aware about the possibility of early detection of oral cancers and had knowledge of oral precancers. This is in contrast to the study conducted in the villages in Kerala, where 90% of the respondents felt early detection of oral cancers was feasible. [7] Another study conducted in the general population in Gorakhpur revealed better knowledge about certain oral precancerous conditions. [8] Majority of the women (75.38%) had knowledge of tobacco being injurious to health. The Kerala study, where literacy rate is highest in the country, 96.6% of the participants had this knowledge. [4] We see herein, that though over 70% women participants were aware of tobacco being dangerous, they were still using it. This strengthens the fact that cessation support, in addition to awareness, is important for quitting tobacco. Tobacco users require help in quitting because of the addictive nature of the nicotine present in the tobacco. As per the Global Adult Tobacco Survey (GATS), majority of the women in India are aware about tobacco causing severe health hazards. [9] Majority (73.46%) women in this program could correctly identify at least one health hazard of tobacco. A study conducted in Delhi had similar findings, wherein, majority participants consisting of mixed population (64.2%), could identify health hazards of smoking. [10] In the present study, only a small proportion of women could identify at least one ill effect of second hand smoking (18.07%). This indicates more awareness needs to be created regarding the harms of passive smoking, as women are likely to be exposed to the same in their homes. This is in contrast to a study among rural women in India, wherein the majority of women (75.8%) were aware about some health hazards of smokeless tobacco use on children. [11]
Very few participant women in the current program had noticed health warnings on tobacco products at pre-intervention. Totally, 10.76% women had seen pictorial warnings and only 3.84% women could recollect having seen both pictorial and written warnings. Whereas, another study from Mumbai revealed that most participants had seen pictorial as well as written health warnings on tobacco products. The message delivered through these health warnings, was, however, not clearly understood by the participants. [12] Only a few women (8.46%) in the present study, at pre-intervention, were aware about the availability of assistance for quitting tobacco. The availability of formal tobacco cessation services in India is still at a very preliminary stage. [13] These services are inadequate to meet the needs of the vast tobacco using population in India. As a result, awareness regarding the availability of quitting assistance is likely to be less among the Indian population. Participant women in the program were aware about tobacco being injurious to health, mainly through information received from the general public. A study from an industry in rural Maharashtra reported that employees had received knowledge about harms of tobacco through hoardings, printed media, television, and doctors. [14]
In the present study, women with formal education had better knowledge about tobacco being harmful for health. Other studies have also indicated knowledge to be positively co-related with education. [4,15] Though the age was not a significant factor in our study, a Karachi study among urban squatter settlement, showed higher knowledge of health hazards of tobacco with increasing age and educational level. [16] In the present study, income was not related to the knowledge of tobacco hazards. However, a study from Morocco reported lesser knowledge about health hazards of tobacco use among lower income group. [17]
A large majority of participant women in this program used masheri. This is similar to another study among women in rural Maharashtra, wherein masheri and betel quid were the most common forms of tobacco use. [18] Another study from Mumbai also revealed that masheri was the most popular form of tobacco use among women, and that majority women used masheri < 3 times a day. [19] This was consistent with findings from the present study. The average age of initiation for masheri use in the current study was similar to the age of initiation for tobacco use among women in India as per the GATS. [9] Male tobacco users in a rural industry in Maharashtra, India, revealed a little higher age at initiation of tobacco. [14] The average age of smoking initiation among women in five European countries was 18 years. [20] The participants in the current program used tobacco within 30 min of waking, which is consistent with the findings of GATS in India. [9]
Majority of the participant women in this program desired to quit tobacco habits. This in contrast to another study from India, wherein only 12% of tobacco users intended to quit within a month's duration. [21] As per GATS in India, and a survey in Kuwait, a little < 50% of the current tobacco users wanted to quit the habit. [1,9] The participant women in this program (61.92%) did not perceive quitting tobacco use as being difficult. This is in contrast to another study conducted in France and India, wherein most participants felt quitting tobacco was a challenge. [22]
Thus, the present study among urban low socioeconomic women in Mumbai, India shows high prevalence of smokeless tobacco. The use of masheri is especially popular among these women. Though the pre-intervention knowledge on various aspects of tobacco was poor amongst these women, it significantly improved in the post-intervention period. This highlights the importance of health awareness programs and tobacco cessation services focused toward changing the KAP. The outcome of different tobacco cessation and education interventions would be greater if it is implemented hand in hand with other strategies such as reducing the easy availability and raising prices of tobacco products thus making it very expensive.
ACKNOWLEDGMENT
We gratefully acknowledge the funding support for the present service program through the Department of Atomic Energy (DAE) under the Eleventh Five Year Plan period. The sponsor (DAE) had no role in planning, designing or conducting the program. The authors wish to acknowledge the contributions of the following persons who have been directly or indirectly associated with the program, viz. Dr. Pranoti Satpute, Ms. Sarika Chavan, Ms. Trupti Shinde, Ms. Anuradha Patil, Mr. Sachin Khedekar and Mr. Tushar Jadhav.
Footnotes
Source of Support: The study was supported by the Department of Atomic Energy (DAE), Government of India under the Eleventh Five Year Plan.
Conflict of Interest: None declared.
REFERENCES
.jpg)
| Fig. 1 Personal interviews being conducted at the house of participant woman to collect the pre-intervention data
| Fig. 2 Comparison of pre and post-intervention knowledge and attitudes about tobacco among women
| Fig. 3 Patterns of tobacco use


 PDF
PDF  Views
Views  Share
Share

