Renal Lymphoma: Primary or First Manifestation of Aggressive Pediatric B cell Lymphoma
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(04): 538-541
DOI: DOI: 10.4103/ijmpo.ijmpo_48_16
Abstract
Renal lymphoma is an uncommon renal tumor in children. Unlike renal lymphomas presenting as bilateral disease and renal failure, we report a boy who presented with unilateral renal involvement. After initial nephrectomy, he achieved remission with multiagent chemotherapy but relapsed systemically within 3 months. He was initiated on salvage chemotherapy with autologous bone marrow transplant. Even though the initial manifestation was localized lymphoma eventually, it turned out to be a systemic disease. He succumbed to disease at 14 months from diagnosis.
Publication History
Article published online:
04 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used forcommercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Renal lymphoma is an uncommon renal tumor in children. Unlike renal lymphomas presenting as bilateral disease and renal failure, we report a boy who presented with unilateral renal involvement. After initial nephrectomy, he achieved remission with multiagent chemotherapy but relapsed systemically within 3 months. He was initiated on salvage chemotherapy with autologous bone marrow transplant. Even though the initial manifestation was localized lymphoma eventually, it turned out to be a systemic disease. He succumbed to disease at 14 months from diagnosis.
Introduction
Primary renal lymphoma (PRL) is an uncommon renal tumor and constitutes 0.7% of extranodal lymphomas.[1] PRL is a rare diagnosis in pediatric age group.[2,3] Secondary involvement of kidneys in lymphoma is very common entity but primary involvement is rare.[4] PRL in pediatric age groups manifest as bilateral renal involvement, renal failure, and anemia.[2,3] There is no standard treatment approach in case of PRL in children.[2,5] We report a very interesting case in a 10-year-old boy presenting as unilateral renal involvement, without any symptoms. With a suspicion of Wilms tumor, he underwent nephrectomy. In spite of aggressive treatment, he relapsed systemically and succumbed to disease.
Case Report
A 10-year-old boy presented to outside facility with complaints of a diffuse lump in the left flank, incidentally noticed by his mother. There is no history of fever, chills, pain, nausea, vomiting, diarrhea, constipation, urinary complaints, chronic infections, or any other palpable masses. Preliminary physical examination showed no fever, dysmorphic features, hypertension, or lymphadenopathy. There was a ballotable left flank mass that was firm to hard in consistency with ill-defined border. An abdominal sonogram revealed a large, solid, reniform mass with heterogeneous echo pattern in the left renal fossa. Hemogram, metabolic, and liver functions were within normal limits, and blood urea was 22 mg/dl and creatinine was 0.7 mg/dl. He was negative for HIV, HbsAg, and HCV. A contrast-enhanced computed tomography study of the chest and abdomen showed an enlarged left kidney, measuring 17.9 cm × 11.5 cm × 10.5 cm, with loss of internal morphological architecture, uniform hypoattenuation, and few areas of heterogeneous enhancement. There were no calcific foci. The renal artery was encased by the mass while the renal vein was patent. There were a few subcentimeter left paraaortic nodes. Lungs and mediastinum were normal. A provisional diagnosis of Wilms tumor was made. The boy was transferred to the care of a surgical oncologist. He underwent a left radical nephrectomy. Postoperative histopathological examination of the specimen was reported as malignant small round cell tumor, without capsular infiltration or vascular emboli, not involving the ureter, possibly Wilms tumor with the diffuse blastemal pattern. The resected lymph nodes were free of metastases. Postoperatively, he received locoregional radiation therapy (RT) to the tumor bed with three-drug regimen as per National Wilms Tumor Study Group IV.
A month later, the boy developed enlargement of the right tonsil and swelling in the right groin. Physical examination showed mild pallor, a right tonsillar mass that was 5 cm × 5 cm and displacing the uvula to other side and right inguinal lymphadenopathy of 3 cm × 3 cm. A fine needle aspiration of the right inguinal lymph node showed metastatic deposits of a malignant round cell tumor. At this point of time, he was referred to our center for further management. The histopathology of the nephrectomy specimen was reviewed. Morphology and immunohistochemistry showed small, round, relatively undifferentiated cells in sheets positive for CD20 and negative for WT-2 and pancytokeratin. A diagnosis of B-non-Hodgkin lymphoma (B-NHL) of the kidney was made. Staging investigations with the whole body 18F fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) showed hypermetabolic large residual disease in the right renal bed and multiple hypermetabolic right tonsil, mediastinal, abdominal and inguinal lymphadenopathy. Bone marrow biopsy was normal. He was diagnosed as B-NHL Stage III A. He was started on chemotherapy with NHL-BFM 95 protocol. He tolerated chemotherapy well and responded well. At the end of six cycles of chemotherapy, he was in complete remission. After 3 months, he again presented with bilateral cervical lymphadenopathy, and biopsy confirmed relapse of B-NHL. Staging workup showed disease on both sides of diaphragm and bone marrow biopsy was negative. He was given salvage treatment with 4 cycles of ifosfamide, etoposide, and carboplatin. He had a very good partial response. In view of limited options and guarded prognosis in a case of early relapsed extranodal NHL in a child, parents consented for autologous bone marrow transplant. After evaluating for the organ reserve, a standard myeloablative regimen of BCNU, etoposide, cytarabine, and melphalan was used. He tolerated the procedure well with mucositis and myelosuppression as main toxicity. At end of 1 month, he was clinical in remission. Two months after autologous BMT, he once again had florid relapse and succumbed to disease, 14 months after diagnosis.
Discussion
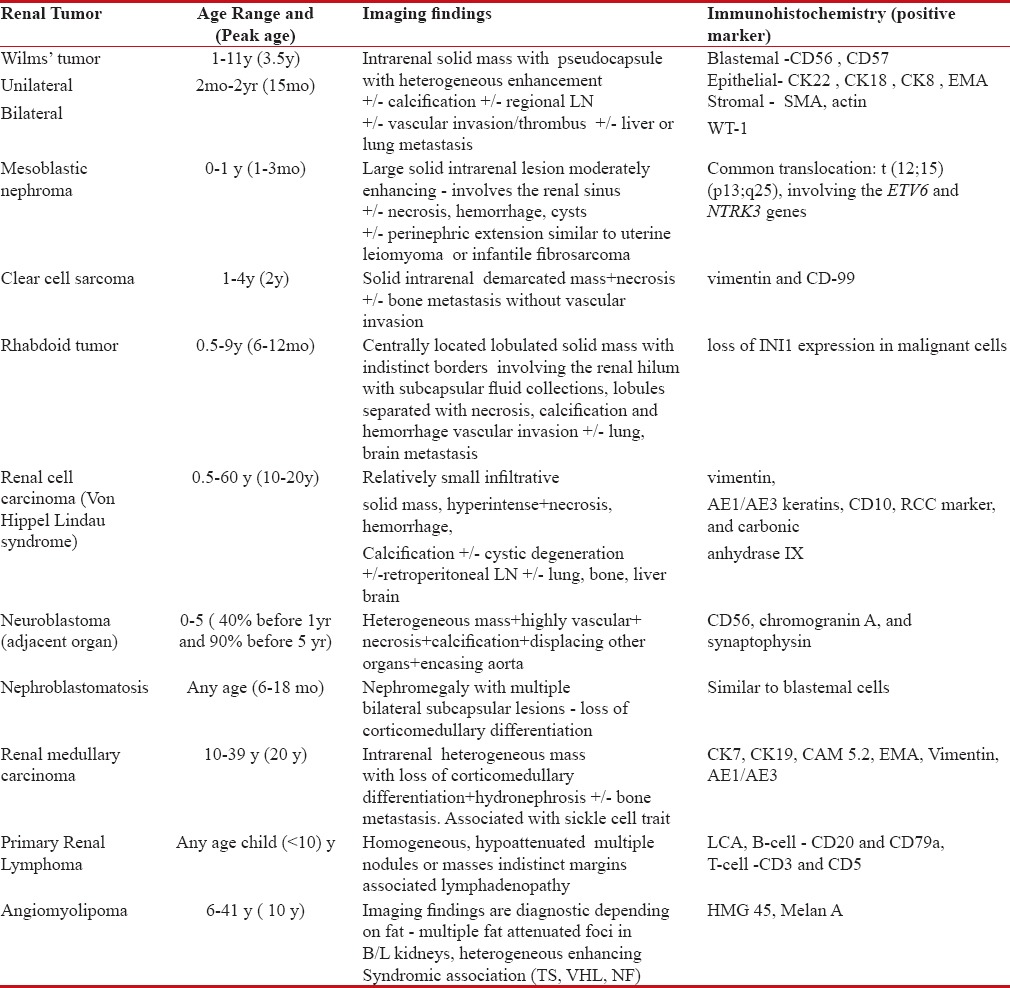
Most common causes of benign enlargement of kidneys are hydronephrosis, polycystic kidney disease, mesoblastic nephroma, multilocular cystic nephroma, multicystic dysplastic kidneys, renal abscess, mesoblastic nephroma, and medullary cystic disease complex. Common malignant kidney tumor is Wilms tumor, neuroblastoma [Table 1].[6]
Table 1
Common Pediatric Renal Tumors
|
Involvement of kidneys in NHL is common and presents as hypodense nodular lesions on imaging or autopsies.[4] Primary involvement of kidney is rare and its existence has been doubted.[7] Based on a report of nine cases in adults, one group suggested the following criteria (1) renal failure as the initial presentation, (2) bilateral enlargement of the kidneys without obstruction and other organ or nodal involvement, (3) diagnosis only made by renal biopsy, (4) absence of other causes of renal failure, and (5) rapid improvement of renal function after radiotherapy or systemic chemotherapy.[8] In this present case, the diagnosis was established in nephrectomy specimen and response to chemotherapy with first-line drugs.
Even though the most common manifestation is bilateral renal involvement, acute renal failure, anemia, hematuria, fatigue, and musculoskeletal pains there are few case reports of unilateral involvement.[2,3] Both T- and B-cell renal lymphoma has been reported.[2,9] In this present case, it manifested as single kidney involvement with no systemic symptoms or renal failure. The patient was 10-year-old, on initial radiological findings, there was suspicion of Wilms tumor, and he underwent nephrectomy. In a case of WT, the common radiological findings are intrarenal heterogeneous mass with pseudo capsule with calcification and involvement of renal vein or inferior vena cava with or without lymphadenopathy, but in a case of lymphoma, there is some hypodense nodular lesion with homogenous involvement with our distinct borders and ± nodal involvement [Table 1]. There are case reports of PRL who underwent nephrectomy, based on radiological features.[10]
Aggressive lymphomas fall into the differential diagnosis of small blue round cells tumors and may be confused with other round cells tumor like neuroblastoma or blastemal component of WT, where immunohistochemitsry (IHC) is of great help. The differential diagnoses of the renal mass with common IHC markers are presented in Table 1. There is growing evidence that a renal mass in a doubtful situation can be subjected to 18FDG PET especially before contemplating nephrectomy. 18FDG PET may be useful in differentiating lymphomas as they have more avid uptake.[11]
In most cases, pediatric renal lymphomas are treated as in adults with six cycles of chemotherapy ± rituximab with varied outcome.[2,5] Patients with renal lymphoma rarely survive more than 1 year.[12]
The interesting lesson learnt from our patient is that PRL can manifest initially with an asymptomatic renal mass and can relapse later with systemic disease. Better radiological, nuclear imaging and comprehensive pathology could have established an earlier and accurate diagnosis. We have treated with multiagent protocol NHL-BFM-95 and autologous transplant, but still, the patient could not be salvaged. Pediatric renal lymphomas are an aggressive form of lymphoma with guarded prognosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Authors would like to thank Department of Pathology, Nizams Institute of Medical Science.
References
- Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer 1972;29:252-60.
- Dhull VS, Mukherjee A, Karunanithi S, Durgapal P, Bal C, Kumar R, et al. Bilateral primary renal lymphoma in a pediatric patient: Staging and response evaluation with 18 F-FDG PET/CT. Rev Esp Med Nucl Imagen Mol 2015;34:49-52.
- Dash SC, Purohit K, Mohanty SK, Dinda AK. An unusual case of bilateral renal enlargement due to primary renal lymphoma. Indian J Nephrol 2011;21:56-8.
- Tefekli A, Baykal M, Binbay M, Barut M, Muslumanoglu AY. Lymphoma of the kidney: Primary or initial manifestation of rapidly progressive systemic disease? Int Urol Nephrol 2006;38:775-8.
- Lee SM, Son IC, Kim JJ, Lee T, Yoon SM, Kim SG. Primary renal lymphoma in a child. Korean J Urol 2001;42:1220-3.
- Lowe LH, Isuani BH, Heller RM, Stein SM, Johnson JE, Navarro OM, et al. Pediatric renal masses: Wilms tumor and beyond. Radiographics 2000;20:1585-603.
- Kandel LB, McCullough DL, Harrison LH, Woodruff RD, Ahl ET Jr., Munitz HA, et al. Primary renal lymphoma. Does it exist? Cancer 1987;60:386-91.
- Malbrain ML, Lambrecht GL, Daelemans R, Lins RL, Hermans P, Zachée P, et al. Acute renal failure due to bilateral lymphomatous infiltrates. Primary extranodal non-Hodgkin's lymphoma (p-EN-NHL) of the kidneys: Does it really exist? Clin Nephrol 1994;42:163-9.
- Sharma SB, Debnath PR, Tripathi R. Primary renal lymphoma in a child. Indian J Pediatr 2006;73:947.
- Hayakawa A, Shimotake N, Kubokawa I, Mitsuda Y, Mori T, Yanai T, et al. Primary pediatric stage III renal diffuse large B-cell lymphoma. Am J Case Rep 2013;14:34-7.
- Ye XH, Chen LH, Wu HB, Feng J, Zhou WL, Yang RM, et al. 18F-FDG PET/CT evaluation of lymphoma with renal involvement: Comparison with renal carcinoma. South Med J 2010;103:642-9.
- Kose F, Sakalli H, Mertsoylu H, Sezer A, Kocer NE, Tokmak N, et al. Primary renal lymphoma: Report of four cases. Oncol Res Treat 2009;32:200-2.
References
- Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer 1972;29:252-60.
- Dhull VS, Mukherjee A, Karunanithi S, Durgapal P, Bal C, Kumar R, et al. Bilateral primary renal lymphoma in a pediatric patient: Staging and response evaluation with 18 F-FDG PET/CT. Rev Esp Med Nucl Imagen Mol 2015;34:49-52.
- Dash SC, Purohit K, Mohanty SK, Dinda AK. An unusual case of bilateral renal enlargement due to primary renal lymphoma. Indian J Nephrol 2011;21:56-8.
- Tefekli A, Baykal M, Binbay M, Barut M, Muslumanoglu AY. Lymphoma of the kidney: Primary or initial manifestation of rapidly progressive systemic disease? Int Urol Nephrol 2006;38:775-8.
- Lee SM, Son IC, Kim JJ, Lee T, Yoon SM, Kim SG. Primary renal lymphoma in a child. Korean J Urol 2001;42:1220-3.
- Lowe LH, Isuani BH, Heller RM, Stein SM, Johnson JE, Navarro OM, et al. Pediatric renal masses: Wilms tumor and beyond. Radiographics 2000;20:1585-603.
- Kandel LB, McCullough DL, Harrison LH, Woodruff RD, Ahl ET Jr., Munitz HA, et al. Primary renal lymphoma. Does it exist? Cancer 1987;60:386-91.
- Malbrain ML, Lambrecht GL, Daelemans R, Lins RL, Hermans P, Zachée P, et al. Acute renal failure due to bilateral lymphomatous infiltrates. Primary extranodal non-Hodgkin's lymphoma (p-EN-NHL) of the kidneys: Does it really exist? Clin Nephrol 1994;42:163-9.
- Sharma SB, Debnath PR, Tripathi R. Primary renal lymphoma in a child. Indian J Pediatr 2006;73:947.
- Hayakawa A, Shimotake N, Kubokawa I, Mitsuda Y, Mori T, Yanai T, et al. Primary pediatric stage III renal diffuse large B-cell lymphoma. Am J Case Rep 2013;14:34-7.
- Ye XH, Chen LH, Wu HB, Feng J, Zhou WL, Yang RM, et al. 18F-FDG PET/CT evaluation of lymphoma with renal involvement: Comparison with renal carcinoma. South Med J 2010;103:642-9.
- Kose F, Sakalli H, Mertsoylu H, Sezer A, Kocer NE, Tokmak N, et al. Primary renal lymphoma: Report of four cases. Oncol Res Treat 2009;32:200-2.


 PDF
PDF  Views
Views  Share
Share

