Quality of Life of Parents of Children with Cancer—Single-Center, Prospective Cross-Sectional Study from South India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2022; 43(03): 255-261
DOI: DOI: 10.1055/s-0042-1749402
Abstract
Introduction Holistic care for children with chronic diseases including cancer should include psychological support for children and their families. The impact of pediatric malignancies in regard to quality of life (QOL) of parents is poorly described.
Objectives We aim to study the QOL of parents of children diagnosed with cancer in physical, psychosocial, environmental, and social domains.
Materials and Methods A prospective, cross-sectional study was conducted with 162 parents of children diagnosed with malignancy for 3 months or more. Assessment was done by World Health Organization quality of life (WHOQOL-BREF) questionnaire that includes four domains with a total of 26 questions. Data analysis was done by using Statistical Package for Social Sciences (SPSS) version 20.0; p-value less than 0.05 was considered significant. Results on continuous measurements were presented as “Mean ± SD” and categorical measurements were presented as percentages (%). Differences in the quantitative variables between groups were assessed by unpaired-t-test; comparison between groups by nonparametric Mann–Whitney U test and chi-squared test was used to analyze categorical variables with p-value of < 0.05 using a two-tailed taken as statistically significant.
Results Mean raw scores of QOL in physical health, psychological, social, and environmental domains were 20.10, 15.28, 8.10, and 25.24, respectively, with social relationships being the lowest; inadequate or low QOL was noted in 50% study population and it was maximally affected by increased duration of treatment, multimodality treatment, socioeconomic status, rural population, education and occupation status of the parents, and increased cost of care. Type of family or place of residence, family history of psychiatric illness, or malignancy did not influence the QOL of parents of children with cancer.
Conclusion Psychological support from the beginning of the treatment along with financial, social support should be offered through a comprehensive care program to improve the QOL.
Keywords
quality of life - WHOQOL-BREF scores - socioeconomic status - psychosocial support - childhood cancerAuthors' Contributions
SGJ wrote the initial draft and it was revised for intellectual content by DJ, JXS, and GM. All the other authors were involved in the management of the child. All authors read and approved the final manuscript.
Publication History
Article published online:
02 July 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Introduction Holistic care for children with chronic diseases including cancer should include psychological support for children and their families. The impact of pediatric malignancies in regard to quality of life (QOL) of parents is poorly described.
Objectives We aim to study the QOL of parents of children diagnosed with cancer in physical, psychosocial, environmental, and social domains.
Materials and Methods A prospective, cross-sectional study was conducted with 162 parents of children diagnosed with malignancy for 3 months or more. Assessment was done by World Health Organization quality of life (WHOQOL-BREF) questionnaire that includes four domains with a total of 26 questions. Data analysis was done by using Statistical Package for Social Sciences (SPSS) version 20.0; p-value less than 0.05 was considered significant. Results on continuous measurements were presented as “Mean ± SD” and categorical measurements were presented as percentages (%). Differences in the quantitative variables between groups were assessed by unpaired-t-test; comparison between groups by nonparametric Mann–Whitney U test and chi-squared test was used to analyze categorical variables with p-value of < 0.05 using a two-tailed taken as statistically significant.
Results Mean raw scores of QOL in physical health, psychological, social, and environmental domains were 20.10, 15.28, 8.10, and 25.24, respectively, with social relationships being the lowest; inadequate or low QOL was noted in 50% study population and it was maximally affected by increased duration of treatment, multimodality treatment, socioeconomic status, rural population, education and occupation status of the parents, and increased cost of care. Type of family or place of residence, family history of psychiatric illness, or malignancy did not influence the QOL of parents of children with cancer.
Conclusion Psychological support from the beginning of the treatment along with financial, social support should be offered through a comprehensive care program to improve the QOL.
Keywords
quality of life - WHOQOL-BREF scores - socioeconomic status - psychosocial support - childhood cancerIntroduction
Each year, ∼400,000 children and adolescents from 0 to 19 years old are diagnosed with cancer across the globe.[1] The diagnosis of cancer in children is often very devastating to the family and has a negative impact on caregivers especially parents in terms of stress (physical, emotional, and financial). It affects their quality of life (QOL) as compared with parents of healthy children and the general healthy population. Impact on QOL may be in terms of physical or personal distress, marital disharmony, economic constraints, or difficulties in adapting to a major change in routine life.[2] [3]
Holistic care for children with cancer should include psychological support and assistance in financial needs to parents apart from medical management of these conditions.[4] In resource-limited settings, lesser accessibility to health care, delayed presentation with advanced stage, and financial restraints are very rampant. Hence, priorities to improve the healthcare and financial aspects should be focused upon to improve accessibility. Structured and proper programs to help parents cope up with their stresses (similar to counseling sessions) by dedicated psycho-oncologists and nurses in developed countries are lacking in developing countries.
There is a lack of substantial research in the subject of QOL of parents of children with cancer, especially from developing countries. This study is intended to measure QOL in parents of children with cancer and to assess relationships of parental QOL with personal, child, disease, and treatment characteristics.
Materials and Methods
This is a cross-sectional study conducted in our tertiary care pediatric hemato-oncology unit in South India between March 2019 and August 2020. One sixty-two participants (either of the parents of children who were diagnosed, admitted in ward for chemotherapy or supportive care, and getting treated for malignancy) were selected as the study group. Parents of children who received chemotherapy or multimodality therapy, on treatment for at least 3 months duration, were included. Those who were diagnosed within 3 months and those who had only surgery/radiation as treatment modality, with relapsed malignancies, or were unwilling to consent were excluded. Children with cancers who were admitted in intensive care units with a complication/morbidity were also excluded.
The World Health Organization quality of life-100 (WHOQOL-100) assessment tool was developed by the WHOQOL group with 15 international field centers simultaneously, in an attempt to develop a QOL assessment tool that does not have differences cross culturally.[5] The WHOQOL-BREF is a scaled down version of the original instrument that may be used more conveniently in large research studies or clinical trials. In World Health Organization Quality of life (WHOQOL-BREF), 26 items were completed by the participant in their language of preference (Tamil or English) themselves or were helped by the principal investigator (the postgraduate doing the study or one of the treating doctors of the team from pediatric hemato-oncology team), when the participant was illiterate. The WHOQOL-BREF questionnaire assesses mainly four domains such as physical (D1), psychological (D2), social (D3), and environmental (D4) with 7, 6, 3, and 8 questions, respectively.
The first two questions assess health and QOL in general. Hence, 26 items related to QOL were answered by the study participants.
Scores in each domain range from 4 to 20 (domain score), where 4 is the worst and 20 is the best score in the domain. They were converted to a score range of 0 to 100 (transformed score), a part of the questionnaire. The transformed scores were used to define the QOL as follows: score > 60 as high, 45 to 60 as moderate, <45>
Socioeconomic status was calculated using modified Kuppuswamy socioeconomic scale (updated for the year 2019).[6] It comprises of occupation of the head of the family, educational qualification of the head of the family, and total monthly income of the family. The scores range from 3 to 29. It is divided into five classes based on scores into lower <5>
Demographic details of the children like name, age, sex, address, diagnosis, and treatment plan were noted down. Details of the parents like education status, income, job details, type of family, and recreational activities were also noted. We wanted to analyze the QOL scores in each domain as primary outcome measures and the factors associated with low QOL as secondary outcome measures.
Based on extensive literature search on QOL studies, with mean score of 47.36 and standard deviation 22.53, sample size was calculated as 127 with relative precision of 10% and desired confidence level of 95%.
Statistical Analysis
Data analysis was done using SPSS (statistical package for social sciences) version 20.0 (IBM SPSS Statistics for Windows, Version 20.0., IBM Corp, Armonk, New York, United States). Difference in quantitative variables between groups was assessed by means of unpaired t-test. Nonparametric data was analyzed using Mann–Whitney U test. Categorical variables were analyzed using chi-squared test. Regression analysis was done to analyze dependent variables that were significantly associated with different levels of QOL. p-Value of < 0.05 was considered significant.
Ethics
Institutional Ethics Committee approval was obtained from our institutional research ethics committee board from Sri Ramachandra Institution of Higher Education and Research (SRIHER - Ref:CSP-MED/19/Mar/51/28) conducted on 02.07.2019. Informed consent was appropriately taken prior to enrolment. Privacy, integrity, and confidentiality of personal information of research subjects were confidentially maintained as per Helsinki declaration.
Results
Among total of 186 children, 20 had relapsed malignancies and 4 parents did not consent for the study. In our study population (n = 162), 61.1% (99) children were boys and 38.9% (63) were girls and 40.1% (65) were less than 5 years of age. Of the 162 children, 62.3% (101) were suffering from hematological malignancies like acute lymphoblastic leukemia (ALL), acute myeloid leukemia, and lymphomas. The rest children (37.7%, 61) had solid tumors including neuroblastoma, renal tumors, germ cell tumors, hepatoblastoma, Ewing's sarcoma, brain tumors, soft tissue sarcomas, and rare tumor types including pancreatoblastoma, adenoid cystic carcinoma, and nasopharyngeal carcinoma.
Among the 162 participants, 79% (128) were mothers while information was provided by fathers in 21% (34). Most of the productive life of parents has been lost in the ordeal against cancer in their children. The mean age of the father was 38.56 years while that of the mother was 34.36 years in our study population. Among 162 parents, most of the parents were educated with 50% up to high school; 55% (89) fathers were unskilled laborers by occupation and 72% (117) mothers were unemployed.
In our study, 63.6%-families had a joint family pattern, 9% parents were single, 11.7% had family history of psychiatric illness, and 57% were from urban background. Majority of them belonged to middle or lower middle class (87%), as detailed in [Table 1].
|
Parameter |
Frequency (n) |
Percentage (%) |
|---|---|---|
|
Type of family |
|
|
|
Nuclear |
103 |
63.6 |
|
Joint |
59 |
36.4 |
|
Living status of parents |
|
|
|
Together |
147 |
90.7 |
|
Single/separated |
15 |
9.3 |
|
Positive family history of cancer |
11 |
6.8 |
|
History of psychiatric illness in family |
19 |
11.7 |
|
Socioeconomic status[*] |
|
|
|
Upper class |
0 |
0 |
|
Upper middle class |
8 |
4.9 |
|
Middle |
66 |
40.7 |
|
Lower middle class |
76 |
46.9 |
|
Lower class |
12 |
7.4 |
|
Residence |
|
|
|
Rural |
69 |
42.6 |
|
Urban |
93 |
57.4 |
|
Frequency (n) |
Percentage (%) |
|
|---|---|---|
|
Ward of admission |
|
|
|
Private |
69 |
42.6 |
|
General |
93 |
57.4 |
|
Insurance to support treatment present |
58 |
35.8 |
|
Funded |
92 |
56.8 |
|
Risk stratification of cancer—high risk |
86 |
53.1 |
|
Duration of treatment |
|
|
|
< 1> |
42 |
25.9 |
|
1–3 years |
39 |
24.1 |
|
> 3 years |
81 |
50 |
|
Type of treatment |
|
|
|
Chemotherapy |
101 |
62.3 |
|
Chemotherapy with surgery |
23 |
14.2 |
|
Chemotherapy with surgery and radiotherapy |
38 |
23.5 |
|
Cost of treatment |
|
|
|
1–5 lakhs |
24 |
14.8 |
|
5–10 lakhs |
99 |
61.1 |
|
> 10 lakhs |
39 |
24.1 |
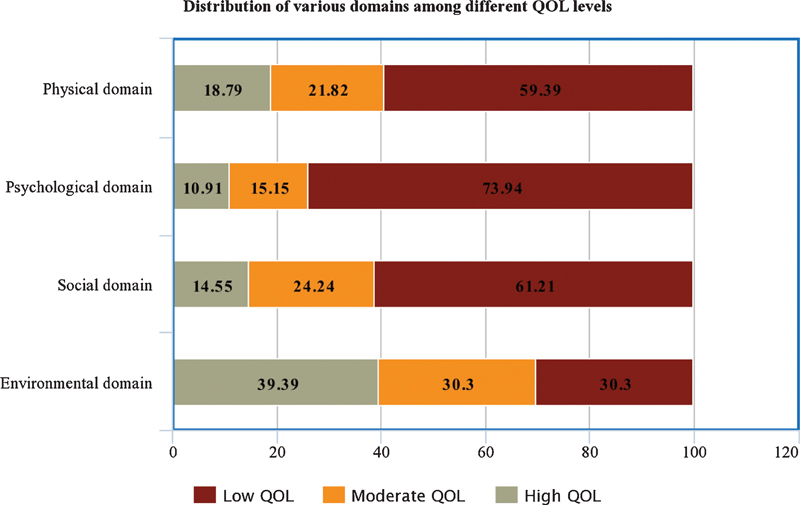
| Figure 1:Distribution of quality of life (QOL) in various domains in the study.
|
Parameter |
F-Value |
Odds ratio |
95% CI |
p-Value |
|---|---|---|---|---|
|
Lower socioeconomic class |
20.44 |
3.522 |
11.17–39.93 |
< 0.001 |
|
Chemotherapy with radiotherapy and surgery |
5.168 |
8.0 |
2.45–19.71 |
0.007 |
|
Treatment cost: 5–10 lakhs |
5.182 |
2.174 |
0.00–0.64 |
0.044 |
|
Treatment duration: 1–3 years |
12.27 |
10.82 |
0.33–0.96 |
< 0.001 |
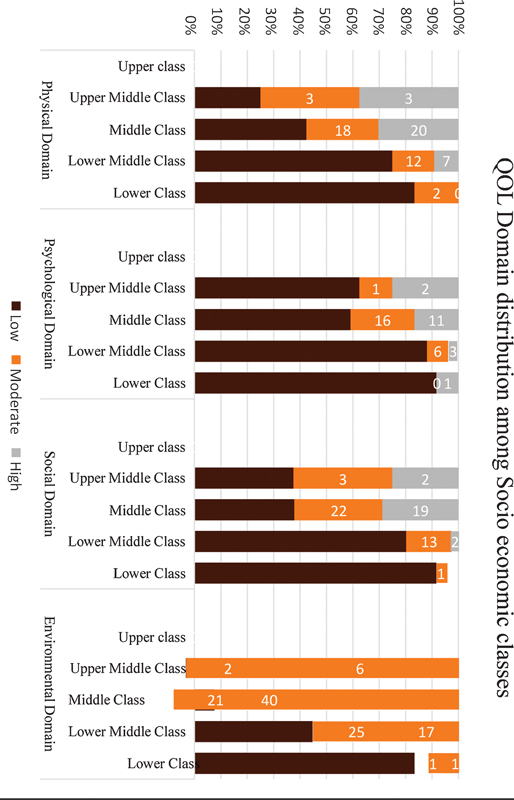
| Figure.2:Quality of life (QOL) scores in various domains among various socioeconomic classes.
Among the other factors, it was found in our study that QOL scores were high in urban population (p = 0 0.039); however, they were not different between nuclear or joint family type (p = 0.871), positive or negative history of psychiatric illness in the family (p = 0.808), positive or negative family history of cancer (p = 0.214), or risk stratification of any cancer type (p = 0.148).
Discussion
Parents of cancer children from developing countries still face fundamental problems like financial stress, social stigma, disrupted family structure, and lack of access to treatment in remote areas, leading to decline in their QOL, as seen in 50% of study population in our study.[7] Research shows that there is long-term physical and psychological impact by cancer on children and families especially during and after treatment when the child appears to be cured or to be a “survivor.”[7]
There were no significant differences among QOL scores in various domains across the age groups in our study. The male to female distribution was 1.5:1. Acute lymphoblastic leukemia (ALL) was the most common childhood cancer constituting 43.8%-cases followed by retinoblastoma and Hodgkin lymphoma. Similar distribution of cancers was noted by epidemiological studies by Swaminathan et al with leukemias, lymphomas, retinoblastomas, and renal tumors being the most common cancer types.[8]
Study by McCubbin et al[9] shows that support from extended family especially from grandparents and in-laws provided assistance in several forms including parental respite, care of the sibling, transportation to the place of treatment, monetary and emotional support. In our study, there was no significant difference noted between QOL scores based on the type of family, probably due to the lack of transparency within families and prevailing stigma. In our study, the parents' WHOQOL-BREF scores were low especially in physical, psychological, and social domains with lowest being the psychological domain. Various other scales including PAT2.0 have been used by Mccarthy et al for the measurement of QOL in caregivers of children with cancer.[10] These findings were comparable to a study by Sajjadi et al[11] wherein the QOL of the caregivers in physical, psychological, and environmental domain was significantly lower than the QOL of the general population that shows the effect on caring for a child with a life-threatening disease. Similar findings have also been seen in studies on the QOL of caregivers of brain tumor patients by Chien et al.[12] Studies by Lin et al and Yuen Shan Leung on caregivers of children with disabilities also reflect similar findings and have attributed these decreases in QOL to a combination of stress and socioeconomic pressures.[13] [14] [15]
Parents from rural setting had lower QOL in our study that may be due to major disruption in family dynamics because of relocation for treatment needs. Educated parents had better QOL than uneducated, as they were able to be involved in decision making for the child and understand the process of treatment better. The parents who are professionals had better QOL in all domains as they were able to manage the financial burden in a better way, whereas unemployed mothers, on the other hand, had low QOL in all domains, probably due to better social and financial situation of the family.[16] Study by Kim and Spillers in 2010[17] have noted that caregivers with more than a high-school education had a positive influence on the QOL measured at a minimum period of 2 years after the child was diagnosed with cancer.
QOL was lowest in all the domains when the time of duration of treatment was more than a year that is proportionate to the financial burden and disruption of family routine for longer duration. Studies by Litzelman et al also support similar findings especially among caregivers of children affected with brain tumors. After 3 years, parents learn to accept and cope up with the disease. Also, most probably, the treatment would come to an end at this point in most of the cases.[2]
The QOL was low in parents of children whose treatment cost was high. QOL of parents was low in all domains for children who need all three modalities of treatment with radiotherapy, surgery, and chemotherapy compared with those who received chemotherapy alone. This is due to the increased financial burden, side effects, and deformities associated with treatment.[18]
This study adds significant information to a growing body of research on parents of children living with cancer beyond the initial phase of the illness trajectory. The need for professional support with the help of psychologist is emphasized through this study. A further study to assess the QOL of parents at different time points might give more strength to the study to arrive at better meaningful conclusions. A multi-institutional study to avoid bias arising due to cultural and social differences might be more appropriate. A larger study with more sample size and a control group is definitely warranted to generalize the conclusions.
Several standards and guidelines that highlight these parameters on the different domains of life are available from developed countries, as summarized by Lorie Weiner et al, where the scenario of social security schemes is different from that of a developing country like India.[19] While several coping measures are available in developed countries, such extensive programs that focus on the QOL among parents are lacking in developing countries.[20] [21] Our study has been conducted as a cross-sectional study drawing results from one-time assessment. Study in a larger population and repeat assessments of the QOL scores in same cohort at periodic intervals might give more insight to make meaningful conclusions. This study would serve as a launch pad for similar research focusing on different domains of QOL among parents of children diagnosed with cancer.
Conclusion
Nearly 50%-of the study population experienced low QOL in our study; it was significantly associated with illiterate parents, lower socioeconomic status, prolonged treatment duration, and increasing cost of treatment. Psychological support from the beginning of the treatment of a child with cancer, apart from the appropriate treatment and financial support through various resources, should be a part of the comprehensive care program to be led by the pediatric oncologists. Evaluation and intervention in a professional manner with routine and timely care would certainly help in reducing the psychological burden of the caregivers and would indirectly improve the quality of care the child and family.
Conflict of Interest
None declared.
Authors' Contributions
SGJ wrote the initial draft and it was revised for intellectual content by DJ, JXS, and GM. All the other authors were involved in the management of the child. All authors read and approved the final manuscript.
References
- Steliarova-Foucher E, Colombet M, Ries LAG. et al; IICC-3 contributors. International incidence of childhood cancer, 2001-10: a population-based registry study. Lancet Oncol 2017; 18 (06) 719-731
- Litzelman K, Catrine K, Gangnon R, Witt WP. Quality of life among parents of children with cancer or brain tumors: the impact of child characteristics and parental psychosocial factors. Qual Life Res 2011; 20 (08) 1261-1269
- Witt WP, Litzelman K, Wisk LE. et al. Stress-mediated quality of life outcomes in parents of childhood cancer and brain tumor survivors: a case-control study. Qual Life Res 2010; 19 (07) 995-1005
- Acton GJ. Health-promoting self-care in family caregivers. West J Nurs Res 2002; 24 (01) 73-86
- The World Health Organization Quality of Life Assessment (WHOQOL). development and general psychometric properties. Soc Sci Med 1998; 46 (12) 1569-1585
- Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh's scale updated for 2019. J Family Med Prim Care 2019; 8 (06) 1846-1849
- Dietz AC, Mulrooney DA. Life beyond the disease: relationships, parenting, and quality of life among survivors of childhood cancer. Haematologica 2011; 96 (05) 643-645
- Swaminathan R, Rama R, Shanta V. Childhood cancers in Chennai, India, 1990-2001: incidence and survival. Int J Cancer 2008; 122 (11) 2607-2611
- McCubbin M, Balling K, Possin P, Frierdich S, Bryne B. Family resiliency in childhood cancer*. Fam Relat 2002; 51 (02) 103-111
- McCarthy MC, Clarke NE, Vance A, Ashley DM, Heath JA, Anderson VA. Measuring psychosocial risk in families caring for a child with cancer: the Psychosocial Assessment Tool (PAT2.0). Pediatr Blood Cancer 2009; 53 (01) 78-83
- Sajjadi H, Vameghi M, Ghazinour M, Khodaeiardekani M. Caregivers' quality of life and quality of services for children with cancer: a review from Iran. Glob J Health Sci 2013; 5 (03) 173-182
- Chien L-Y, Lo L-H, Chen C-J, Chen Y-C, Chiang C-C, Yu Chao YM. Quality of life among primary caregivers of Taiwanese children with brain tumor. Cancer Nurs 2003; 26 (04) 305-311
- Lin J-D, Hu J, Yen C-F. et al. Quality of life in caregivers of children and adolescents with intellectual disabilities: use of WHOQOL-BREF survey. Res Dev Disabil 2009; 30 (06) 1448-1458
- ;Yuen ShanLeung C, Wai PingLi- Tsang C. Quality of life of parents who have children with disabilities. Hong Kong J Occup Ther 2003; 13 (01) 19-24
- Kim Y, Spillers RL. Quality of life of family caregivers at 2 years after a relative's cancer diagnosis. Psychooncology 2010; 19 (04) 431-440
- Matthews RA, Booth SM, Taylor CF, Martin T. A qualitative examination of the work– family interface: parents of children with autism spectrum disorder. J Vocat Behav 2011; 79 (03) 625-639
- Kim J, Chung H, Amtmann D, Salem R, Park R, Askew RL. Symptoms and quality of life indicators among children with chronic medical conditions. Disabil Health J 2014; 7 (01) 96-104
- Mosher CE, Bakas T, Champion VL. Physical health, mental health, and life changes among family caregivers of patients with lung cancer. Oncol Nurs Forum 2013; 40 (01) 53-61
- Wiener L, Kazak AE, Noll RB, Patenaude AF, Kupst MJ. Standards for the psychosocial care of children with cancer and their families: an introduction to the special issue. Pediatr Blood Cancer 2015; 62 (Suppl. 05) S419-S424
- Kazak AE, Barakat LP. Brief report: parenting stress and quality of life during treatment for childhood leukemia predicts child and parent adjustment after treatment ends. J Pediatr Psychol 1997; 22 (05) 749-758
- Kerr LMJ, Harrison MB, Medves J, Tranmer JE, Fitch MI. Understanding the supportive care needs of parents of children with cancer: an approach to local needs assessment. J Pediatr Oncol Nurs 2007; 24 (05) 279-293
Address for correspondence
Publication History
Article published online:
02 July 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2,
Noida-201301 UP, India
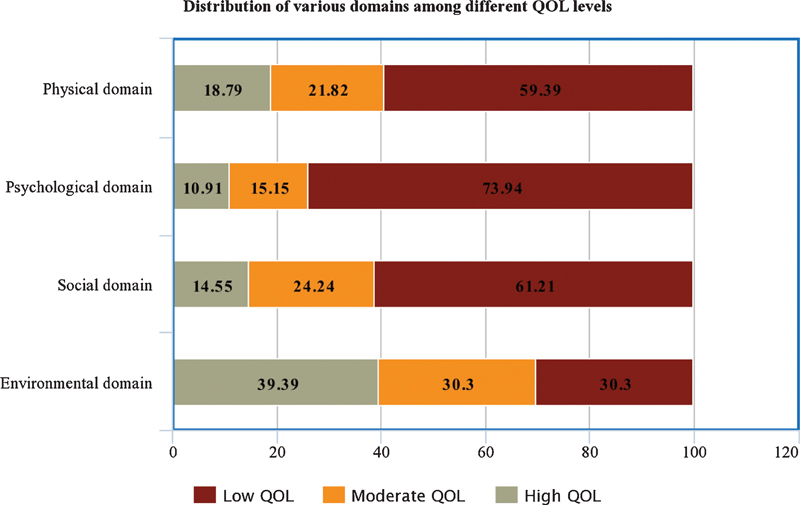
| Figure 1:Distribution of quality of life (QOL) in various domains in the study.
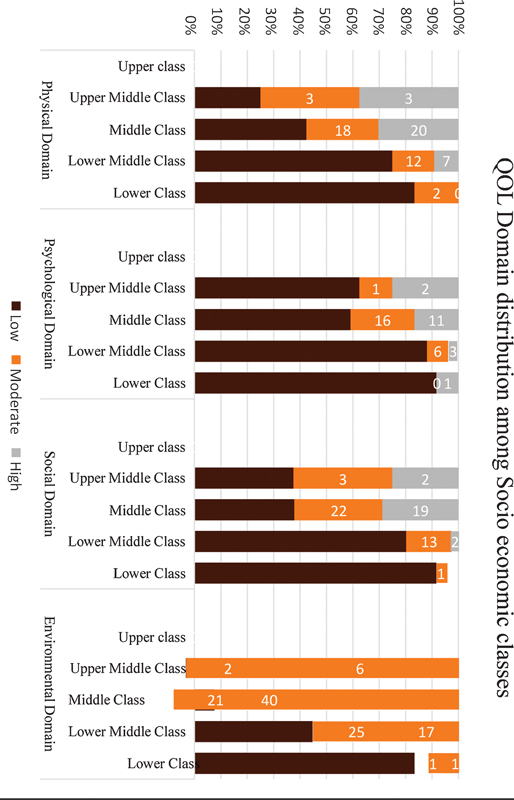
| Figure.2:Quality of life (QOL) scores in various domains among various socioeconomic classes.
References
- Steliarova-Foucher E, Colombet M, Ries LAG. et al; IICC-3 contributors. International incidence of childhood cancer, 2001-10: a population-based registry study. Lancet Oncol 2017; 18 (06) 719-731
- Litzelman K, Catrine K, Gangnon R, Witt WP. Quality of life among parents of children with cancer or brain tumors: the impact of child characteristics and parental psychosocial factors. Qual Life Res 2011; 20 (08) 1261-1269
- Witt WP, Litzelman K, Wisk LE. et al. Stress-mediated quality of life outcomes in parents of childhood cancer and brain tumor survivors: a case-control study. Qual Life Res 2010; 19 (07) 995-1005
- Acton GJ. Health-promoting self-care in family caregivers. West J Nurs Res 2002; 24 (01) 73-86
- The World Health Organization Quality of Life Assessment (WHOQOL). development and general psychometric properties. Soc Sci Med 1998; 46 (12) 1569-1585
- Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh's scale updated for 2019. J Family Med Prim Care 2019; 8 (06) 1846-1849
- Dietz AC, Mulrooney DA. Life beyond the disease: relationships, parenting, and quality of life among survivors of childhood cancer. Haematologica 2011; 96 (05) 643-645
- Swaminathan R, Rama R, Shanta V. Childhood cancers in Chennai, India, 1990-2001: incidence and survival. Int J Cancer 2008; 122 (11) 2607-2611
- McCubbin M, Balling K, Possin P, Frierdich S, Bryne B. Family resiliency in childhood cancer*. Fam Relat 2002; 51 (02) 103-111
- McCarthy MC, Clarke NE, Vance A, Ashley DM, Heath JA, Anderson VA. Measuring psychosocial risk in families caring for a child with cancer: the Psychosocial Assessment Tool (PAT2.0). Pediatr Blood Cancer 2009; 53 (01) 78-83
- Sajjadi H, Vameghi M, Ghazinour M, Khodaeiardekani M. Caregivers' quality of life and quality of services for children with cancer: a review from Iran. Glob J Health Sci 2013; 5 (03) 173-182
- Chien L-Y, Lo L-H, Chen C-J, Chen Y-C, Chiang C-C, Yu Chao YM. Quality of life among primary caregivers of Taiwanese children with brain tumor. Cancer Nurs 2003; 26 (04) 305-311
- Lin J-D, Hu J, Yen C-F. et al. Quality of life in caregivers of children and adolescents with intellectual disabilities: use of WHOQOL-BREF survey. Res Dev Disabil 2009; 30 (06) 1448-1458
- ;Yuen ShanLeung C, Wai PingLi- Tsang C. Quality of life of parents who have children with disabilities. Hong Kong J Occup Ther 2003; 13 (01) 19-24
- Kim Y, Spillers RL. Quality of life of family caregivers at 2 years after a relative's cancer diagnosis. Psychooncology 2010; 19 (04) 431-440
- Matthews RA, Booth SM, Taylor CF, Martin T. A qualitative examination of the work– family interface: parents of children with autism spectrum disorder. J Vocat Behav 2011; 79 (03) 625-639
- Kim J, Chung H, Amtmann D, Salem R, Park R, Askew RL. Symptoms and quality of life indicators among children with chronic medical conditions. Disabil Health J 2014; 7 (01) 96-104
- Mosher CE, Bakas T, Champion VL. Physical health, mental health, and life changes among family caregivers of patients with lung cancer. Oncol Nurs Forum 2013; 40 (01) 53-61
- Wiener L, Kazak AE, Noll RB, Patenaude AF, Kupst MJ. Standards for the psychosocial care of children with cancer and their families: an introduction to the special issue. Pediatr Blood Cancer 2015; 62 (Suppl. 05) S419-S424
- Kazak AE, Barakat LP. Brief report: parenting stress and quality of life during treatment for childhood leukemia predicts child and parent adjustment after treatment ends. J Pediatr Psychol 1997; 22 (05) 749-758
- Kerr LMJ, Harrison MB, Medves J, Tranmer JE, Fitch MI. Understanding the supportive care needs of parents of children with cancer: an approach to local needs assessment. J Pediatr Oncol Nurs 2007; 24 (05) 279-293


 PDF
PDF  Views
Views  Share
Share

