Primary Rectal Lymphoma with Synchronous Liver Involvement: An Extremely Rare Case Report
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2020; 41(01): 93-95
DOI: DOI: 10.4103/ijmpo.ijmpo_103_18
Abstract
Both primary rectal lymphoma (PRL) and primary hepatic lymphoma are rare entities, concomitant NHL in rectum and liver is an extremely rare coincidence. Cases of primary colonic lymphoma however can be found in literature. We report an extremely rare case of PRL with synchronous liver involvement after obtaining written informed consent, with a review of available literature. The case was provisionally diagnosed to be an adenocarcinoma of rectum with liver metastasis, with final confirmation on immunohistochemistry. PRL with synchronous liver involvement is an extremely rare coincidence. It is usually confused with more common adenocarcinoma of rectum with liver metastasis posing diagnostic challenges. The optimal management of PRL has never been validated through randomized trials. The treatment options include chemotherapy, radiation, surgical treatment, or a combination of these. Chemotherapeutic agents of choice are the cyclophosphamide, doxorubicin, vincristine, and prednisone regimen, with or without monoclonal antibody rituximab.
Publication History
Received: 03 May 2018
Accepted: 21 June 2018
Article published online:
23 May 2021
? 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Both primary rectal lymphoma (PRL) and primary hepatic lymphoma are rare entities, concomitant NHL in rectum and liver is an extremely rare coincidence. Cases of primary colonic lymphoma however can be found in literature. We report an extremely rare case of PRL with synchronous liver involvement after obtaining written informed consent, with a review of available literature. The case was provisionally diagnosed to be an adenocarcinoma of rectum with liver metastasis, with final confirmation on immunohistochemistry. PRL with synchronous liver involvement is an extremely rare coincidence. It is usually confused with more common adenocarcinoma of rectum with liver metastasis posing diagnostic challenges. The optimal management of PRL has never been validated through randomized trials. The treatment options include chemotherapy, radiation, surgical treatment, or a combination of these. Chemotherapeutic agents of choice are the cyclophosphamide, doxorubicin, vincristine, and prednisone regimen, with or without monoclonal antibody rituximab.
Keywords
Non-Hodgkin?s lymphoma - primary hepatic lymphoma - primary rectal lymphomaIntroduction
Non-Hodgkin?s lymphomas (NHL) may be nodal and extranodal; gastrointestinal tract (GIT) is the most common site of extranodal lymphoma.[1] Primary rectal lymphoma (PRL) is the rarest disorder of all primary gastrointestinal lymphomas, accounting for 0.1%?0.6% of all colonic malignancies and 0.05% of all primary rectal malignancies.[2] Primary GIT lymphoma occurs in the absence of evidence of systemic disease, mimicking other more common benign and malignant bowel tumors, resulting in misguided provisional diagnosis and late accurate diagnosis. Immunodeficiency and inflammatory bowel diseases have been cited as possible risk factors, although the exact etiology remains unknown.[2] The treatment is a multimodality approach with combinations of surgery, chemotherapy, and radiotherapy.
Case Report
We herein report a case of 66-year-old female who presented to us with right upper abdominal pain for the last 3?4 months. She also complained of weight loss and per-rectal bleeding. A palpable mass was identified in the dentate line fixed to the rectal wall. The superior border of the tumor could not be reached. Physical examination revealed hepatomegaly, palpable 3 cm below the right costal margin. Her hemogram revealed hemoglobin 7.6 g/dl; and liver function tests were slightly deranged with serum bilirubin 1.3 mg/dl, serum glutamic-oxaloacetic transaminase 41 U/L and serum glutamic-pyruvic transaminase 53 U/L. Kidney function tests were within normal limits. Her serum carcinoembryonic antigen and carbohydrate antigen (CA) 19-9 was normal. Other biochemical tests were within normal limits. Contrast-enhanced computed tomography (CECT) of the abdomen and pelvis revealed multiple hypodense to isodense lesions of variable sizes in both lobes of liver with minimal ascites [Figure 1]. Ultrasonography-guided fine-needle aspiration cytology from liver showed malignant round-cell tumor, possibility of NHL was suggested. Further workup included CECT of neck and thorax and bone marrow aspiration and biopsy. CECT thorax revealed minimal right pleural effusion. CECT neck revealed enlarged retromandibular, upper cervical and jugular lymph nodes (largest measuring 14 mm). Punch biopsy of the rectal mass was taken. Histopathology showed diffuse and extensive infiltration of lamina propria and underlying tissue with sheats of round cells with vesicular nuclei and ill-defined scanty cytoplasm suggestive of a round-cell neoplasm. Immunohistochemical staining showed that the tumor cells were positive for CD20, MUM-1, BCL-6 and BCL-2 while negative for CD3, CD10, and cytokeratin (CK) [Figure 2]. The MIB score was 70%. The diagnosis of diffuse large B-cell lymphoma (DLBCL) was established.
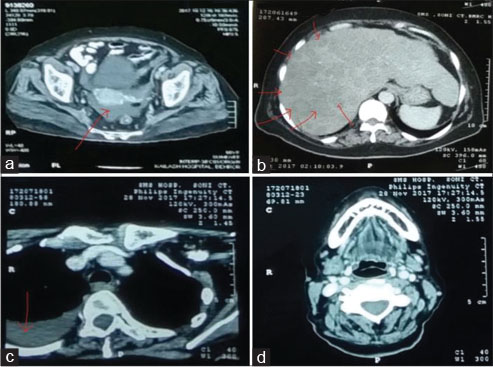
|?Fig. 1: Contrast-enhanced computed tomography of (a) Pelvis showing rectal mass, (b) Abdomen showing multiple hypodense lesions in liver parenchyma, (c) Thorax showing pleural effusion,(d) head and neck showing the normal architecture
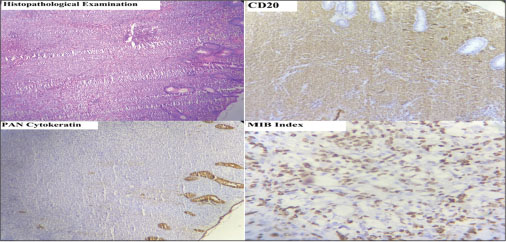
|?Fig. 2: Histopathological and immunohistochemical examination of rectal mass. On immunohistochemistry, it stained positive for CD20 and negative for pan cytokeratin with mib score of 70%, favoring non-Hodgkin?s lymphoma-diffuse large B-cell typ
Discussion
PRL is a rare extranodal lymphoma comprising 0.1%?0.5% of all colorectal malignancies and 1.4% of all cases of NHL.[2] Cecum is the most frequent location for primary colonic lymphoma; in different series, the data on the frequency in the rectum varies from 8.3% to 35%.[3] [4] Primary hepatic lymphoma is even rare, accounting for <0.016% of all NHL.[5]?Concomitant NHL in rectum and liver is an extremely rare coincidence; the present case, to the best of our knowledge, is the first reported case of synchronous rectal and hepatic lymphoma, although a few cases of synchronous colonic and hepatic lymphoma have been cited in the literature. It is very difficult to differentiate PRL based on clinical and radiological findings from adenocarcinoma rectum with hepatic metastasis.[6] [7] PRL occur more often in conditions of immunosuppression (HIV infection), inflammatory bowel disease (ulcerative colitis), and following organ transplantation.[2] Men are affected twice as common as women, with the mean age of 55 years at diagnosis. The usual presentation is with abdominal pain, weight loss, and changing bowel habits.
The diagnosis of primary colonic lymphoma is based on five diagnostic criteria: no enlarged superficial lymph nodes when the patient is first seen; chest radiographs without obvious enlargement of the mediastinal nodes; the white blood cell counts, both total and differential, are within normal range and bone marrow biopsy is also normal; at laparotomy only regional nodes are affected by disease; and the liver and spleen seem free of tumor.[8] Our case, however, had lesion in the liver also.
The majority of patients with rectal lymphoma present with nonspecific symptoms or negative rectal biopsy, which often leads to misleading provisional diagnosis and delayed accurate diagnosis with an advanced stage at presentation. CT scan is helpful not only in suggesting diagnosis but also in describing tumor extension and staging. Points favoring the radiological diagnosis of lymphoma are CT appearance of extensive abdominal lymphadenopathy, location at the cecum, demarcation from the peri-colonic fat with no invasion of surrounding viscera, concentric wall thickening involving the full thickness of the bowel wall, and the absence of desmoplastic reaction.[7] In more than half of the patients, lymphoma is a bulky disease. The role of positron emission tomography in the diagnosis and follow-up of patients with colorectal lymphoma is yet to be established.
Pathological analysis of a biopsy remains the gold standard for diagnosis of this disease. As colorectal lymphoma originates from the submucosa, accurately obtaining a biopsy sample is challenging, resulting in low pathological positive rate. The most common histological subtype of colorectal lymphoma is DLBCL; other may be follicular lymphoma, Burkitt lymphoma, and Mantle cell lymphoma. DLBCL cells generally express pan B cell markers such as CD20, CD19, CD22, CD45 and CD79a; 70% of tumor cells express BCL-6 protein; and 30%?60% express CD10.[9] In our case, the tumor cells were strongly positive for CD20, MUM-1, BCL-6 and BCL-2 while negative for CD3, CD10, and CK, with MIB score of 70%.
As there is only a low incidence of the disease, there have been no prospective studies evaluating the relative benefits of adjuvant chemotherapy, radiotherapy, surgery, or a combination of treatments for PRL.[10] The treatment options for colorectal DLBCL usually involves chemotherapy, radiation, surgical treatment, or a combination of these modalities. Chemotherapeutic agents of choice are the cyclophosphamide, doxorubicin, vincristine, and prednisone regimen, with or without monoclonal antibody rituximab. Surgery may be of use in preventing complications such as hemorrhage, obstruction, and perforation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
References
- Zucca E, Roggero E, Bertoni F, Cavalli F.?Primary extranodal non-Hodgkin?s lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol 1997; 8: 727-37
- Stanojevic GZ, Nestorovic MD, Brankovic BR, Stojanovic MP, Jovanovic MM, Radojkovic MD. et al.?Primary colorectal lymphoma: An overview. World J Gastrointest Oncol 2011; 3: 14-8
- Stanojevic GZ, Stojanovic MP, Stojanovic MM, Krivokapic Z, Jovanovic MM, Katic VV. et al.?Non-Hodgkin?s lymphomas of the large bowel-clinical characteristics, prognostic factors and survival. Acta Chir Iugosl 2008; 55: 109-14
- Cho MJ, Ha CS, Allen PK, Fuller LM, Cabanillas F, Cox JD. et al.?Primary non-Hodgkin lymphoma of the large bowel. Radiology 1997; 205: 535-9
- Warnera B, Birda G, Schofielda J, Rassama S.?Primary hepatic lymphoma: A diagnosis to remember. J Med Cases 2013; 4: 52-5
- Risio D, Percario R, Legnini M, Caldaralo F, Angelucci D, Marinelli C. et al.?Diffuse large B-cell lymphoma of the colon with synchronous liver metastasis: A rare case report mimicking metastatic colorectal adenocarcinoma. BMC Surg 2014; 14: 75
- Peng JX, Wang LZ, Tan ZJ, Zhong XS, Huang YX, Diao JF. et al.?Concomitant non-Hodgkin?s lymphoma in colon and liver: Report of a rare case and review of literature. Int J Clin Exp Pathol 2015; 8: 3257-61
- Dawson IM, Cornes JS, Morson BC.?Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg 1961; 49: 80-9
- Colomo L, L?pez-Guillermo A, Perales M, Rives S, Mart?nez A, Bosch F. et al.?Clinical impact of the differentiation profile assessed by immunophenotyping in patients with diffuse large B-cell lymphoma. Blood 2003; 101: 78-84
- Bilsel Y, Balik E, Yamaner S, Bugra D.?Clinical and therapeutic considerations of rectal lymphoma: A case report and literature review. World J Gastroenterol 2005; 11: 460-1
Address for correspondence
Publication History
Received: 03 May 2018
Accepted: 21 June 2018
Article published online:
23 May 2021
? 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
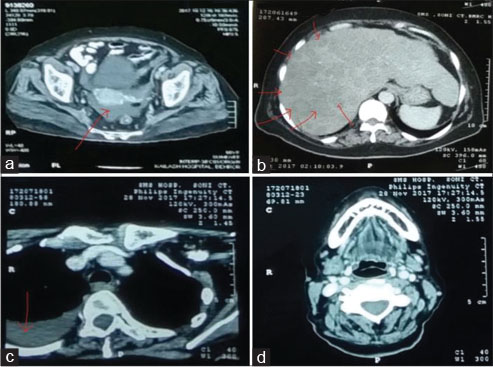
|?Fig. 1: Contrast-enhanced computed tomography of (a) Pelvis showing rectal mass, (b) Abdomen showing multiple hypodense lesions in liver parenchyma, (c) Thorax showing pleural effusion,(d) head and neck showing the normal architecture
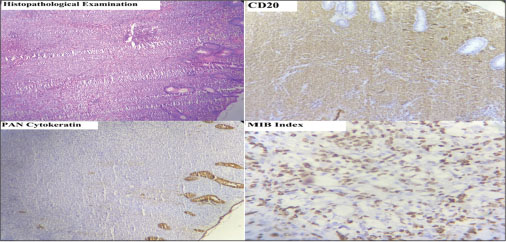
|?Fig. 2: Histopathological and immunohistochemical examination of rectal mass. On immunohistochemistry, it stained positive for CD20 and negative for pan cytokeratin with mib score of 70%, favoring non-Hodgkin?s lymphoma-diffuse large B-cell typ
References
- Zucca E, Roggero E, Bertoni F, Cavalli F.?Primary extranodal non-Hodgkin?s lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol 1997; 8: 727-37
- Stanojevic GZ, Nestorovic MD, Brankovic BR, Stojanovic MP, Jovanovic MM, Radojkovic MD. et al.?Primary colorectal lymphoma: An overview. World J Gastrointest Oncol 2011; 3: 14-8
- Stanojevic GZ, Stojanovic MP, Stojanovic MM, Krivokapic Z, Jovanovic MM, Katic VV. et al.?Non-Hodgkin?s lymphomas of the large bowel-clinical characteristics, prognostic factors and survival. Acta Chir Iugosl 2008; 55: 109-14
- Cho MJ, Ha CS, Allen PK, Fuller LM, Cabanillas F, Cox JD. et al.?Primary non-Hodgkin lymphoma of the large bowel. Radiology 1997; 205: 535-9
- Warnera B, Birda G, Schofielda J, Rassama S.?Primary hepatic lymphoma: A diagnosis to remember. J Med Cases 2013; 4: 52-5
- Risio D, Percario R, Legnini M, Caldaralo F, Angelucci D, Marinelli C. et al.?Diffuse large B-cell lymphoma of the colon with synchronous liver metastasis: A rare case report mimicking metastatic colorectal adenocarcinoma. BMC Surg 2014; 14: 75
- Peng JX, Wang LZ, Tan ZJ, Zhong XS, Huang YX, Diao JF. et al.?Concomitant non-Hodgkin?s lymphoma in colon and liver: Report of a rare case and review of literature. Int J Clin Exp Pathol 2015; 8: 3257-61
- Dawson IM, Cornes JS, Morson BC.?Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg 1961; 49: 80-9
- Colomo L, L?pez-Guillermo A, Perales M, Rives S, Mart?nez A, Bosch F. et al.?Clinical impact of the differentiation profile assessed by immunophenotyping in patients with diffuse large B-cell lymphoma. Blood 2003; 101: 78-84
- Bilsel Y, Balik E, Yamaner S, Bugra D.?Clinical and therapeutic considerations of rectal lymphoma: A case report and literature review. World J Gastroenterol 2005; 11: 460-1


 PDF
PDF  Views
Views  Share
Share

