Primary cutaneous large B-cell lymphoma, leg type: Report of two cases and review of literature
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2012; 33(01): 54-57
DOI: DOI: 10.4103/0971-5851.96973
Abstract
Primary cutaneous large B-cell lymphoma, leg type (PCLBCL-LT), is very rare neoplasm presenting on and confined to leg(s). PCLBCL-LT is distinguished from other type of primary cutaneous B-cell lymphoma (PCBCL) by its frequent relapses and poorer prognosis. We report, two cases of PCLBCL-LT, occurring in two younger patients compared to published cases in literature. Both the patients were treated with chemotherapy and local radiotherapy. During the 1-year follow-up period one patient presented with extracutaneous dissemination and succumbed. The other patient is symptom free and follow-up period was uneventful.
Publication History
Article published online:
13 April 2022
© 2012. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Primary cutaneous large B-cell lymphoma, leg type (PCLBCL-LT), is very rare neoplasm presenting on and confined to leg(s). PCLBCL-LT is distinguished from other type of primary cutaneous B-cell lymphoma (PCBCL) by its frequent relapses and poorer prognosis. We report, two cases of PCLBCL-LT, occurring in two younger patients compared to published cases in literature. Both the patients were treated with chemotherapy and local radiotherapy. During the 1-year follow-up period one patient presented with extracutaneous dissemination and succumbed. The other patient is symptom free and follow-up period was uneventful.
INTRODUCTION
Primary cutaneous B-cell lymphomas (PCBCLs) are less frequent than cutaneous T-cell lymphomas, with incidence rates varying considerably between European (ranges from 20 to 25% of all PCBCL) and north American studies (ranges from 3.2 to 7.7%).[1] Nowadays the new World Health Organization-European Organization for Research and Treatment of Cancer (WHO-EORTC) classification for cutaneous lymphomas identifies four main types of PCBCLs: 1) primary cutaneous marginal zone B-cell lymphoma; 2) primary cutaneous follicle center lymphoma; 3) primary cutaneous large B-cell lymphoma, leg type (PCLBCL-LT); 4) primary cutaneous large B-cell lymphoma, other.[2]
There are many unanswered questions concerning the homing of B-cells to the skin and their predilection to stay localized in the cutis. In the skin, there are no known equivalents to Peyer's patches of the intestinal tract or Waldeyer's ring of the pharynx. It has been postulated that skin and draining lymph nodes form an integrated system whereby a lympho-proliferative response to an antigenic stimuli may be elicited in the skin.[3] Therefore, primary cutaneous B-cell lymphoma (PCBCL) may be due to neoplastic amplification of this process and may be considered skin-associated lymphoid tissue-related B-cell lymphomas.[3]
CASE REPORTS
Case 1
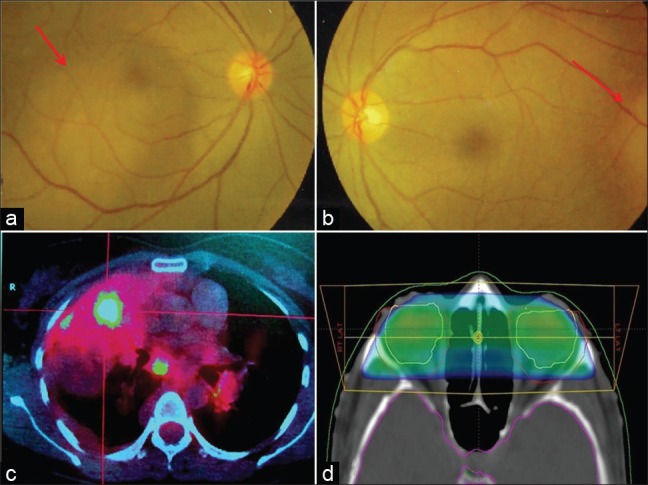
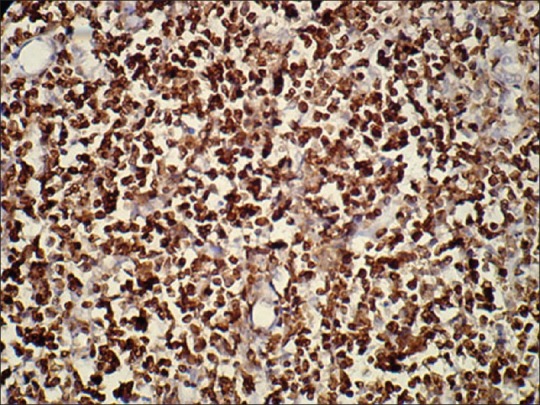
A 26-year-old male presented with light red plaque on medial aspect of left leg of 5 months duration. Recently, the lesion was rapidly increasing in size and subsequently ulcerated [Figure 1]. The lesion was very firm with a hard texture to touch. He also complained of local pain. Incisional biopsy was taken from the non ulcerated area and material was sent for histopathological examination. Microscopical examinations revealed diffuse non epidermotropic infiltrares predominantly made up of large non cleaved cells with variable proportions of centroblasts and immunoblast-like cells. The cells have large nuclei with conspicuous nucleoli. The tumor cells were located in the papillary and reticular dermis and reaching the interface between dermis and subcutis [Figure 2]. No epidermotropism was evident and epithelial cells of epidermis were unremarkable. Immunohistochemistry (IHC) revealed expression of CD20, CD19, Bcl-2, Bcl- 6 and MUM-1 by tumor cells, while they were negative for CD10, CD30, EMA, CD3, and CD5 [Figures [Figures33 and and4].4]. Proliferative index (Mib 1) was 30%. Based on the clinical, histopathologic, and the IHC examination, a diagnosis of PCLBCL-LT was established. Radiologic examination, peripheral blood smear examination, and bone marrow did not reveal any abnormality and/or involvement by lymphoma. Patient was treated with Rituximab, cyclophosphomide, doxorubicin, oncovin, and prednisone (R-CHOP). Local radiotherapy / involved field radiotherapy (IFRT) was also given. However, after 3 months the patient came back with central nervous system/brain involvement and paraparesis. Despite the treatment, the patient died within 1 month.
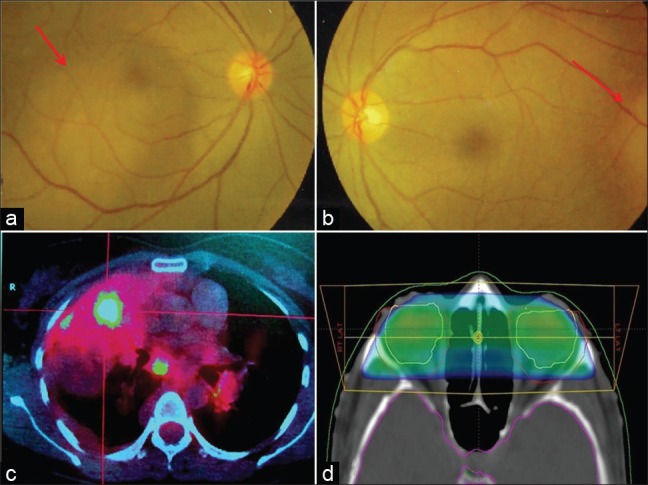
| Fig. 1 Clinical photograph (after biopsy) of case 1 showing residual ulcerated light red plaque on medial aspect of left leg
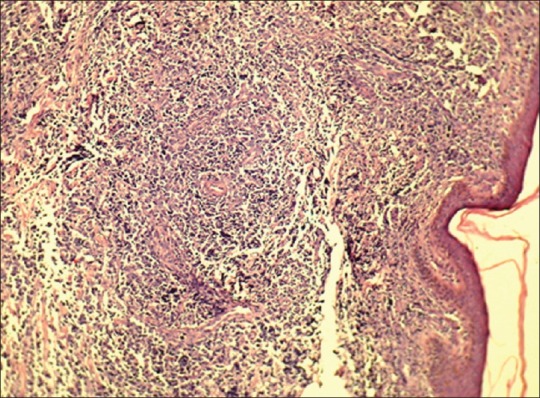
| Fig. 2 Photomicrograph (low power) showing diffuse nonepidermotropic infiltrates of tumor cells in the papillary and reticular dermis (Hematoxylin and Eosin, ×100)
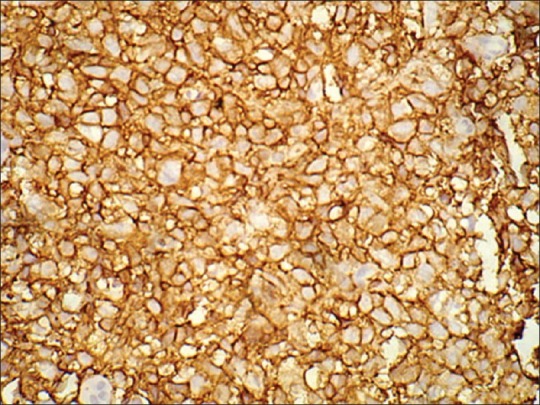
| Fig. 3 Photomicrograph showing CD20 positivity (cytoplasmic membrane) by tumor cells (×400)
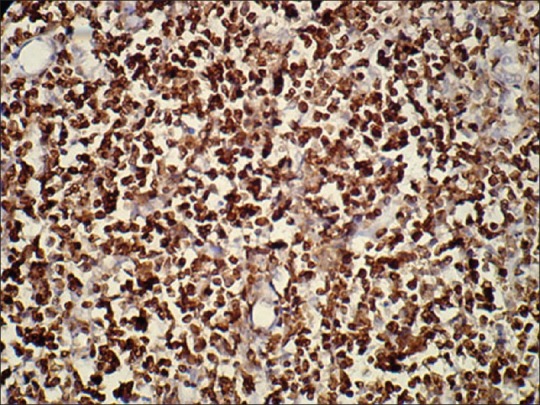
| Fig. 4 Photomicrograph showing Bcl-6 positivity (nuclear) by tumor cells (×100)
Case 2
A 38-year-old lady presented with non ulcerated plaque over right thigh for 6 months. The lesion was slowly increasing in size. Incisonal biopsy was taken and histopathological examination revealed similar findings as in case 1 [Figure 5]. IHC analysis was also same. Proliferative index (Mib 1) was 40%. Therefore, a diagnosis of PCLBCL-LT was given after excluding the possibility of lymphoma at any other site. The patient was treated with the same treatment protocol R-CHOP and IFRT. A 2-year follow up was uneventful and the patient is symptom free.
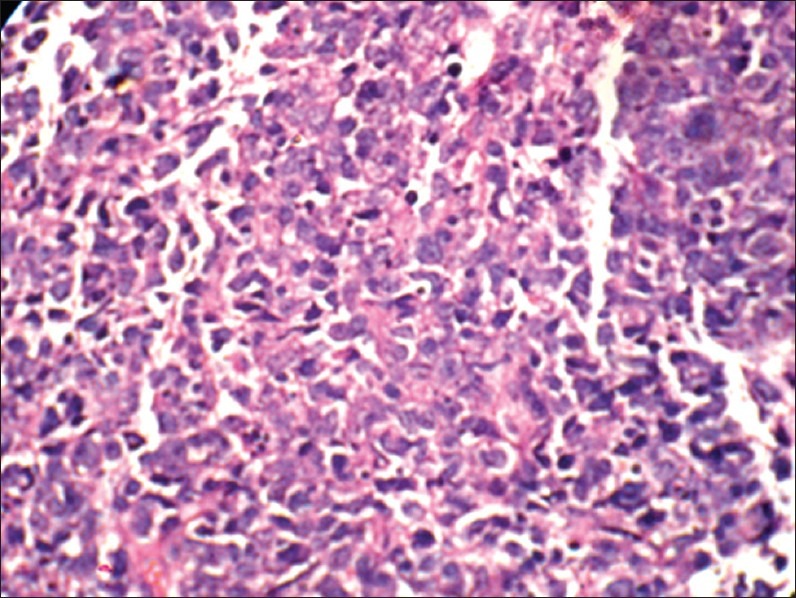
| Fig. 5 Photomicrograph (high power) showing monomorphic large cells arranged in diffuse sheets. The cells have the high nuclearcytoplasmic ratio and prominent single to multiple nucleoli (Hematoxylin and Eosin, ×400)
DISCUSSION
Approximately 27% of non-Hodgkin lymphomas occur in extranodal sites, and the skin is the second most common site of extranodal involvement after the gastrointestinal tract.[4] PCLBCL-LT is diagnosed by the presence of medium sized to large B lymphoid cells in diffuse sheets with round nuclei and conspicuous nucleoli that express BCl-2. In this update of the classification, the localization on the leg is incidental to the immunohistological aspects, which represent the diagnostic criteria, irrespective of the site of the onset. This explains the new term “leg type” instead of the previous “of the leg” in EORTIC, 1997 classification. In the WHO, 2001 classification this entry was known as diffuse large B-cell lymphoma (DLBCL), which later on grouped as PCLBCL-LT in the latest WHO, 2008 classification. Location other than legs have been reported to be sporadic even in the large series of patients, in particular trunk localization is found in 7.5-13.3% of all PCLBCL-LT.[5] Prognosis of PCLBCL-LT depends on pathologic features such as age of the patient, presence of multiple skin lesions (but not spread of single lesion) and disease duration.[5–7]
PCLBCL-LT usually affects the elderly patients with a female preponderance.[5,6] This subset comprise of approximately 1-3% of all cutaneous lymphomas and 5-105 of PCBCL.[8] It has intermediate clinical behavior and 5-year survival rate is 41%.[2] It presents as unique red or violaceous rapidly growing nodule or plaque, frequently ulcerated and located in the lower limb. Our cases are unusual for presentation in younger patients (age ranging between 26 and 38 years) compared to mean age of presentation (70 years) published in the literature.[2,5] Moreover, one of the two lesions was non ulcerated that is an uncommon finding in PCLBCL-LT.
The tumor cells of PCLBCL-LT express monotypic SIg and Cig, C19, C20, CD22, and CD79A. These lymphomas generally strongly express the BCL-2 protein, but are not associated with the interchromosomal t (14; 18) translocation. BCI-6 is expressed by most of the cases but CD10 is negative. In our cases, IHC analysis showed expression of CD20, CD19, MUM-1, Bcl-6 and BCl-2 by tumor cells whereas they were negative for CD10, CD30, EMA, CD5, and CD3. Both BCl-6 and BCl-2 expression were seen in our two cases. Later on one patient died with extracutaneous dissemination (brain involvement). The adverse prognostic impact of the BCl-2 expression has recently been substantiated by gene expression profiling studies showing high expression levels of apoptosis-including cytotoxic effector genes, which lead to constitutive inhibition of apoptotic pathways in the neoplastic cells.[9]
Radiotherapy is less effective in PCL BCL-LT and relapse rate was 58%. Extracutaneous progression was found in 30% of the cases.[10] Recent reviews suggest that PCL BCL-LT should be treated as systemic DLBCL with multiagent chemotherapy with or without rituximab.[2] Some suggest that these patients should be treated with various combinations of age-adapted, anthracycline containing chemotherapies and rituximab have a better outcome than patients receiving other treatments. Nowadays, R-CHOP with or without IFRT is considered as first line of treatment in PCL BCL-LT but the efficiency of this approach is still poorly documented.[10] Because follow up of the group treated with this protocol was insufficient (mean follow up period less than 2 years) to determine a statistically significant difference. In our case, both the patients received the R-CHOP+IFRT. During 1-year follow up period, one patient died with extracutaneous dissemination while the other patient is asymptomatic.
To conclude, PCL BCL-LT is a very rare type of cutaneous lymphoma and clinically it should be regarded as DLBCL. Though current recommendation to treat these cases is R-CHOP+IFRT, more controlled clinical trials are needed before coming to a conclusion.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
| Fig. 1 Clinical photograph (after biopsy) of case 1 showing residual ulcerated light red plaque on medial aspect of left leg
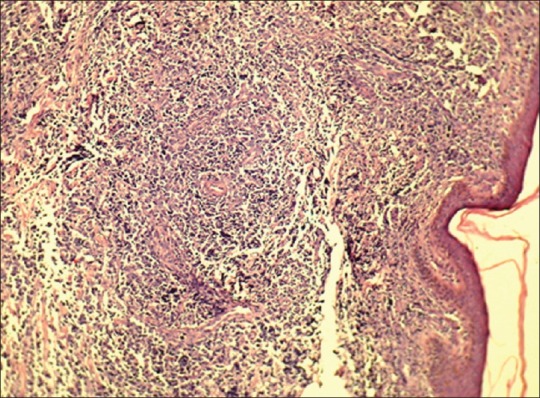
| Fig. 2 Photomicrograph (low power) showing diffuse nonepidermotropic infiltrates of tumor cells in the papillary and reticular dermis (Hematoxylin and Eosin, ×100)
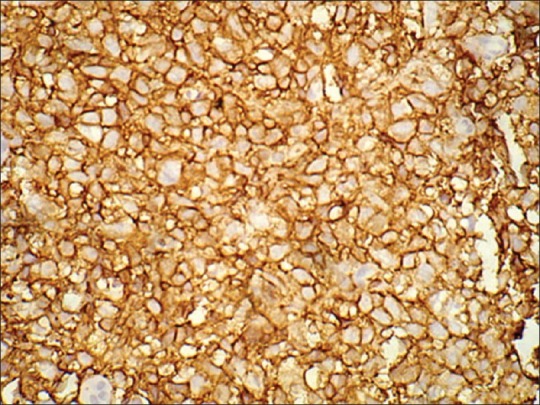
| Fig. 3 Photomicrograph showing CD20 positivity (cytoplasmic membrane) by tumor cells (×400)
| Fig. 4 Photomicrograph showing Bcl-6 positivity (nuclear) by tumor cells (×100)
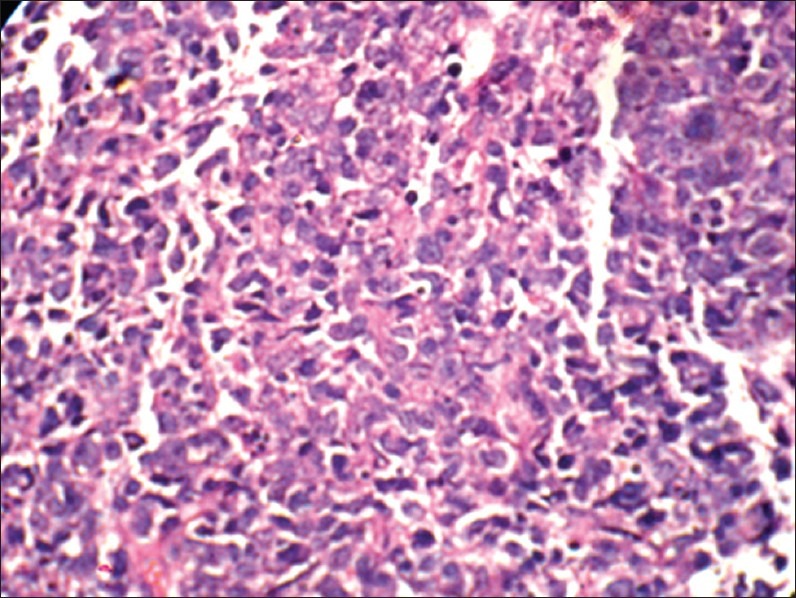
| Fig. 5 Photomicrograph (high power) showing monomorphic large cells arranged in diffuse sheets. The cells have the high nuclearcytoplasmic ratio and prominent single to multiple nucleoli (Hematoxylin and Eosin, ×400)


 PDF
PDF  Views
Views  Share
Share

