Posttraumatic Growth and Psychological Distress among Female Breast Cancer Survivors in India: A Cross-Sectional Study
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2022; 43(02): 165-170
DOI: DOI: 10.1055/s-0042-1742441
Abstract
Introduction Breast cancer survivors (BCS) may experience a cascade of negative reactions during the entire treatment process in the form of psychiatric morbidity. However, exposure to a traumatic event also has the fertile ground for the potential to catalyze a host of positive changes, including development in personal, interpersonal, and spiritual levels, commonly referred to as posttraumatic growth (PTG). PTG is defined as “positive psychological change experienced due to a struggle with highly challenging life circumstances.”
Objective This study aims to measure the prevalence and correlates of PTG among BCS.
Materials and Methods It was a cross-sectional study carried in a tertiary care center of North India from January 2021 to April 2021. Total 700 BCS were approached and screened using the purposive sampling technique. Data were analyzed using the Statistical Package for Social Sciences, version 20.
Results The mean age (standard deviation [SD]) of the patients was 43.14 (8.53) years. The mean (SD) PTG score was 37 (13.66). Among the subdomain of PTG, most respondents showed growth in personal strength, relating to others, followed by an appreciation of life, spiritual change, and less growth in new possibilities. PTG was found to be significantly positively correlated with treatment completion time (r = 2.260, p = 0.02) and negatively correlated with depression, anxiety, and stress (r = –0.152, p = 0.04; r = –0.145, p = 0.05; r = –0.162, p = 0.02).
Conclusion Psychological morbidities must be addressed along with medical treatment of breast cancer so that growth post trauma can be further facilitated.
Keywords
breast cancer survivors - posttraumatic growth - psychological distress - depression - anxiety - women - body image disturbancesSource(s) of Support
None.
Presentation at a Meeting
None.
Publication History
Article published online:
08 March 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Introduction Breast cancer survivors (BCS) may experience a cascade of negative reactions during the entire treatment process in the form of psychiatric morbidity. However, exposure to a traumatic event also has the fertile ground for the potential to catalyze a host of positive changes, including development in personal, interpersonal, and spiritual levels, commonly referred to as posttraumatic growth (PTG). PTG is defined as “positive psychological change experienced due to a struggle with highly challenging life circumstances.”
Objective This study aims to measure the prevalence and correlates of PTG among BCS.
Materials and Methods It was a cross-sectional study carried in a tertiary care center of North India from January 2021 to April 2021. Total 700 BCS were approached and screened using the purposive sampling technique. Data were analyzed using the Statistical Package for Social Sciences, version 20.
Results The mean age (standard deviation [SD]) of the patients was 43.14 (8.53) years. The mean (SD) PTG score was 37 (13.66). Among the subdomain of PTG, most respondents showed growth in personal strength, relating to others, followed by an appreciation of life, spiritual change, and less growth in new possibilities. PTG was found to be significantly positively correlated with treatment completion time (r = 2.260, p = 0.02) and negatively correlated with depression, anxiety, and stress (r = –0.152, p = 0.04; r = –0.145, p = 0.05; r = –0.162, p = 0.02).
Conclusion Psychological morbidities must be addressed along with medical treatment of breast cancer so that growth post trauma can be further facilitated.
Keywords
breast cancer survivors - posttraumatic growth - psychological distress - depression - anxiety - women - body image disturbancesIntroduction
Breast cancer (BC) is the most common malignancy affecting millions of individuals worldwide.[1] Various therapeutic modalities are used to cure BC over an extended period.[2] Many psychiatric disorders are associated as a result of the diagnosis of BC.[3] [4] This journey of the entire treatment procedure is difficult as it brings financial burden, disruption of family routine, disfigurement in the body, fear of recurrence (FORC), and death.[3] [4] [5]
Despite all the adverse outcomes, positive changes have been observed in survivors after BC's frightening and traumatic journey.[6] Different individuals use different coping mechanisms to deal with additional adversity of life like BC. A growing literature suggests the development of positive changes resulting from traumatic events known as posttraumatic growth (PTG). PTG is defined as “positive change in the individual's previous level of functioning aftermath a traumatic experience.”[7] According to Tedeschi and Calhoun, PTG encompasses five domains of positive growth: more significant appreciation of life and a changed sense of priority; increased sense of personal strength; closer relationships with others; recognition of new possibilities for one's life; and spiritual growth.[7] [8] Evidence from western literature suggests the development of PTG is associated with various demographic and clinical variables.[7] [9] [10] In the current study, we aimed to know the outcome of PTG among breast cancer survivors (BCS) and the relationship between PTG, psychological distress, body image disturbances, and demographic and clinical variables among women who have survived BC in Indian demography.
Methods and Materials
Sample and Procedure
A cross-sectional study was conducted during January to April 2021 in a tertiary care teaching hospital in North India. We have approached (matching the study population) 700 BCS for the study, treated in the institution from January 2016 to June 2020. We reviewed the patients' medical records to confirm the diagnosis, time of diagnosis, treatment method, and stage of cancer. The final study sample was selected based on inclusion and exclusion criteria ([Fig. 1]). Patients were recruited using purposive sampling during their follow-up visits, and some patients were contacted using the telephone. We explained the purpose of the study to participants in their local language. Women between 18 and 60 years of age, diagnosed and treated for BC, and who have completed their active treatment for at least 3 months (surgery, chemotherapy, and radiotherapy) were included in the study. Patients with metastasis, recurrent cancer, and receiving treatment for any psychiatric comorbidities were excluded from the study. To ensure anonymity, we included no names or other identifying information in the questionnaires or database.
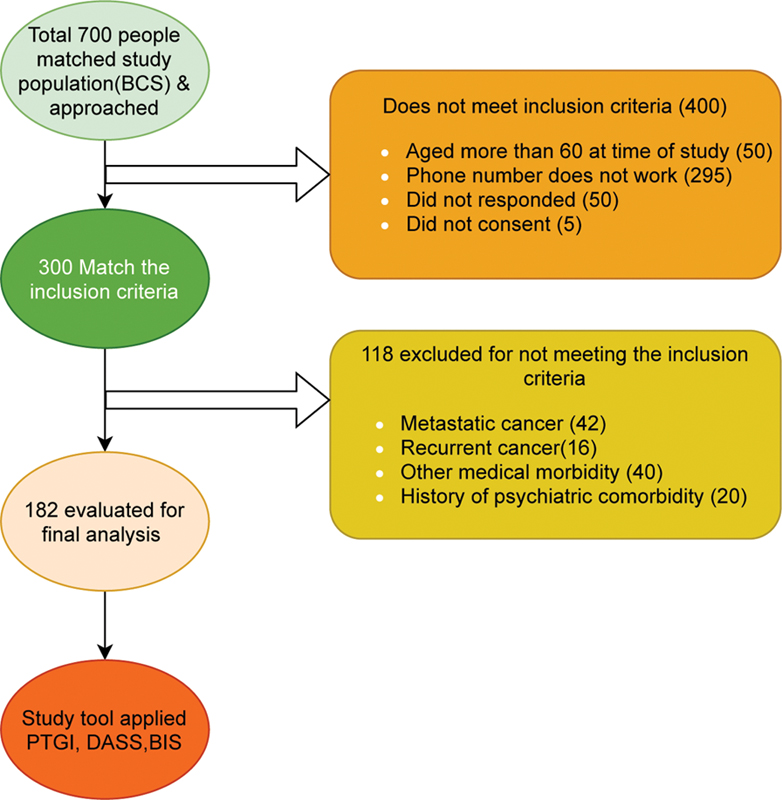
| Fig. 1Recruitment process of the samples. BIS, Body image scale; DASS-21, Depression, Anxiety, and Stress Scale; PTGI, Posttraumatic Growth Inventory Short Form.
Measure
Patients were assessed using a semi-structured proforma for socio-demographic and clinical details. PTG was measured using posttraumatic growth inventory (PTGI-10 item).[11] Psychological distress was measured using the depression, anxiety, and stress scale (DASS-21) comprising 21 articles.[12] Body image disturbances were measured using a 10-item body image scale.[13] All the tools were administered by the interviewer (mental health professional). Patients found to be positive for any psychiatric morbidity were referred to the department of psychiatry for further consultation.
Depression, Anxiety, and Stress Scale (DASS-21)
The DASS-21 is a self-report questionnaire consisting of three dimensions of negative emotional states: depression, anxiety, and stress/tension (Lovibond and Lovibond, 1995; Page et al., 2007).[41] Seven items measure each dimension, and each item is calculated using a 4-point Likert-type scale, ranging from 0 (“did not apply to me at all”) to 3 (“applied to me very much, or most of the time”). Scores of at least 10 for depression, 8 for anxiety, and 15 for stress indicate clinical levels of distress for each subscale, respectively. The DASS-21 has good reliability and validity, and we found it to be moderately sensitive to change (Page et al., 2007).[41]
Posttraumatic Growth Inventory Short Form (PTGI-SF)
The PTGI (Steffens and Andrykowski, 2014; Tedeschi and Calhoun, 1996[8]) assesses personal growth that can arise from the experience of cancer. While the original PTGI scale has 26 items, the PTGI short form (PTGI-SF[11]) consists of 10 items to measure 5 subscales: new possibilities, relating to others, personal strength, appreciation of life, and spiritual change. Each item is scored on a 6-point Likert scale on the basis of the degree of change that has occurred for the participants concerning that item, ranging from 0, “No change,” to 5, “Change to a very great degree.” The total score ranges from 0 to 50, with a higher score indicating a higher level of PTG. The PTGI-SF has been found to have good internal reliability (α = 0.72–0.89), and the adjusted correlations between the PTGI and PTGI-SF total scores were consistently near or above 0.90.
Body Image
The 10-item body image scale was developed as a unitary measure to measure body image distress, including influence, actions, and cognition, and has been commonly used in oncology contexts. Participants assessed the degree to which they agreed with statements on a 4-point Likert scale, such as “Did you feel self-conscious about your appearance?” (0, not at all, to 3, very much). The total summary scores will range from 0 (no distress) to 30 (high body image distress). This scale demonstrates high reliability (α = 0.93) of the item and strong clinical validity and alteration sensitivity. In the current analysis, the item reliability of this scale was high (α = 0.94).
Statistical Analysis
Statistical analysis was performed using SPSS-20 software. The continuous variables were compared using the t-test, and the ordinal and nominal variables of the two groups were compared using the Chi-square test. We studied the relationship between various domains of PTG and body image and other variables using the Pearson correlation coefficient.
Ethics
The procedures followed were as per the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964, as revised in 2013. The present study was approved by the Institutional Ethics Committee of King George's Medical University, Lucknow, Uttar Pradesh, India, dated January 22, 2021 (Ref code: 104th ECM IIA/P14). Informed consent has been obtained from the patients.
Results
Total 700 BCS were selected for the study. We applied inclusion and exclusion criteria to the subjects. Final analyses were used on 182 BCS. The recruitment process is presented in [Fig. 1].
Socio-Demographic and Clinical Details of the Study Sample
The mean (standard deviation [SD]) age of the patients was 43.14 (8.53) years. The majority of the patients in the study were housewives 175 (96.2%), not literate 56 (30.8%). The majority (180, 98.9%) of the patients were married and belonging to Hindu religion (142, 78%), living in a joint family (127, 69.8%), from an urban and semi-urban background (118, 69.7%), and with monthly family income ranging between 5,000 and 10,000 Indian rupee (127, 69.8%).
The mean (SD) duration of completion of treatment was 13.05 (10.54) months, with a median of 12 ranging from 4 to 64 months. We found family history negative for cancer and other psychiatric morbidities in 175 (96.2%) and 164 (90.01%) of subjects, respectively. The majority of the patients were diagnosed at the third stage of malignancy (99, 54.4%). More than half of the women, 105 (57.7%), were in premenopausal status. The majority, 168 (92.3%), of the patients expressed FORC of BC.
Prevalence of Depression, Anxiety, and Stress and Body Image Disturbances
The prevalence of depression, anxiety, and stress in our study (29.11%, 33.5%, 25.25%, respectively) in majority of the patients was with mild severity ([Table 2]). The mean (SD) body image score was 20.30 (6.48).
|
Variables |
Mean (SD) |
|
|---|---|---|
|
Posttraumatic growth/subdomain |
37.00 (11.38) |
|
|
1. Relating to other |
8.56 (2.45) |
|
|
2. New possibilities |
6.71 (2.68) |
|
|
3. Personal strength |
8.67 (2.36) |
|
|
4. Spiritual change |
8.43 (2.18) |
|
|
5. Appreciation of life |
8.62 (2.30) |
|
|
Psychological distress |
Depression |
10.43 (9.76) |
|
Anxiety |
6.06 (5.43) |
|
|
Stress |
9.97 (6.06) |
|
|
Body image score |
Body image score among MRM + BCS patients |
18.40 (8.52) |
|
Body image score among MRM patients |
20.34 (6.48) |
|
|
Clinical variable/severity (n = 182) |
Depression: n (%) |
Anxiety: n (%) |
Stress: n (%) |
|---|---|---|---|
|
Normal |
129 (70.09) |
121 (66.05) |
136 (74.07) |
|
Mild |
33 (18.01) |
31 (17.0) |
39 (21.04) |
|
Moderate |
8 (4.04) |
23 (12.06) |
6 (3.03) |
|
Severe + very severe |
9 + 3 (6.05) |
6 + 1 (3.08) |
1 (0.5) |
|
Variable |
r, p |
|
|---|---|---|
|
Posttraumatic growth |
Treatment completion time |
r = 2.260, p = 0.02 |
|
Depression |
r = –0.145, p = 0.05 |
|
|
Anxiety |
r = –0.152, p = 0.04 |
|
|
Stress |
r = –0.162, p = 0.02 |
|
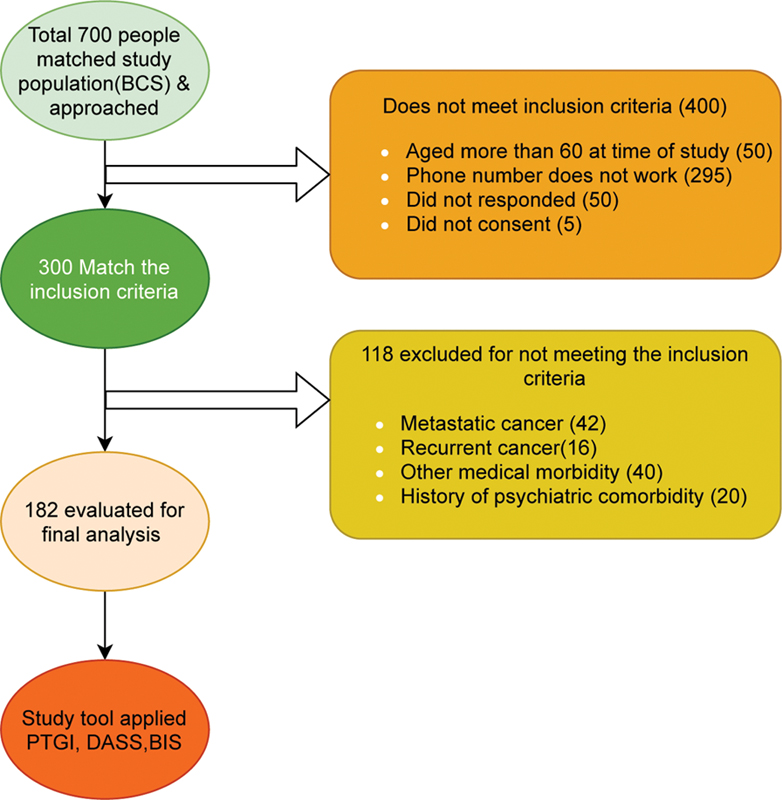
| Fig. 1Recruitment process of the samples. BIS, Body image scale; DASS-21, Depression, Anxiety, and Stress Scale; PTGI, Posttraumatic Growth Inventory Short Form.
References
- Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J. et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013; 49 (06) 1374-1403
- Ferlay J, Soerjomataram I, Dikshit R. et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015; 136 (05) E359-E386
- Thakur M, Gupta B, Kumar R, Mishra AK, Gupta S, Kar SK. Depression among women diagnosed with breast cancer: a study from North India. Indian J Med Paediatr Oncol 2019; 40 (03) 347
- Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr 2004; (32) 57-71
- Thakur M, Sharma R, Mishra AK, Singh KR. Prevalence and psychobiological correlates of depression among breast cancer patients. Indian J Surg Oncol 2021; 12 (02) 251-257
- Calhoun LG, Tedeschi RG. AUTHOR RESPONSE: The Foundations of Posttraumatic Growth: New Considerations. Psychol Inq 2004; 15 (01) 93-102
- Tedeschi RG, Calhoun LG. Post-traumatic growth: conceptual foundations and empirical evidence. Psychol Inq 2004; 15 (01) 1-8
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 1996; 9 (03) 455-471
- Bellizzi KM, Blank TO. Predicting posttraumatic growth in breast cancer survivors. Health Psychol 2006; 25 (01) 47-56
- Updegraff JA, Taylor SE. From vulnerability to growth: positive and negative effects of stressful life events. In Harvey JH, Miller ED. eds. Loss and Trauma: General and Close Relationship Perspectives. Philadelphia, PA: Brunner-Routledge; 2000: 3-28
- Cann A, Calhoun LG, Tedeschi RG. et al. A short form of the Posttraumatic Growth Inventory. Anxiety Stress Coping 2010; 23 (02) 127-137
- Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol 2005; 44 (Pt 2): 227-239
- Hopwood P, Fletcher I, Lee A, Al Ghazal S. A body image scale for use with cancer patients. Eur J Cancer 2001; 37 (02) 189-197
- Srivastava V, Ansari MA, Kumar A. et al. Study of anxiety and depression among breast cancer patients from North India. Ann Clin Psychiatry 2016; 2 (01) 4
- Shreyamsa M, Singh D, Ramakant P. et al. Barriers to timely diagnosis and management of breast cancer: observations from a tertiary referral center in resource poor setting. Indian J Surg Oncol 2020; 11 (02) 287-293
- Kriplani A, Banerjee K. An overview of age of onset of menopause in northern India. Maturitas 2005; 52 (3-4): 199-204
- ;Kim Y, Carver CS, Spillers RL, Love-Ghaffari M, Kaw CK. Dyadic effects of fear of recurrence on the quality of life of cancer survivors and their caregivers. Qual Life Res 2012; 21 (03) 517-525
- McDowell ME, Occhipinti S, Ferguson M, Dunn J, Chambers SK. Predictors of change in unmet supportive care needs in cancer. Psychooncology 2010; 19 (05) 508-516
- Vickberg SM. The Concerns About Recurrence Scale (CARS): a systematic measure of women's fears about the possibility of breast cancer recurrence. Ann Behav Med 2003; 25 (01) 16-24
- Kuswanto CN, Sharp J, Stafford L, Schofield P. Posttraumatic growth as a buffer and a vulnerability for psychological distress in breast cancer survivors mothers. J Affect Disord 2020; 275: 31-37
- Manne S, Ostroff J, Winkel G, Goldstein L, Fox K, Grana G. Posttraumatic growth after breast cancer: patient, partner, and couple perspectives. Psychosom Med 2004; 66 (03) 442-454
- Sharma A, Zhang J. Predictors of post-traumatic growth among breast cancer patients in Nepal. Asian Pacific J Health Sci. 2017; 4 (02) 9-17
- Härtl K, Schennach R, Müller M. et al. Quality of life, anxiety, and oncological factors: a follow-up study of breast cancer patients. Psychosomatics 2010; 51 (02) 112-123
- Danhauer SC, Russell GB, Tedeschi RG. et al. A longitudinal investigation of posttraumatic growth in adult patients undergoing treatment for acute leukemia. J Clin Psychol Med Settings 2013; 20 (01) 13-24
- Cordova MJ, Cunningham LL, Carlson CR, Andrykowski MA. Posttraumatic growth following breast cancer: a controlled comparison study. Health Psychol 2001; 20 (03) 176-185
- Barthakur MS, Sharma MP, Chaturvedi SK, Manjunath SK. Post-traumatic growth in women survivors of breast cancer. Indian J Palliat Care 2016; 22 (02) 157-162
- Mehrabi E, Hajian S, Simbar M, Houshyari M, Zayeri F. Post-traumatic growth: a qualitative analysis of experiences regarding positive psychological changes among Iranian women with breast cancer. Electron Physician 2015; 7 (05) 1239-1246
- Brix SA, Bidstrup PE, Christensen J. et al. Post-traumatic growth among elderly women with breast cancer compared to breast cancer-free women. Acta Oncol 2013; 52 (02) 345-354
- Casellas-Grau A, Vives J, Font A, Ochoa C. Positive psychological functioning in breast cancer: an integrative review. Breast 2016; 27: 136-168
- Cormio C, Muzzatti B, Romito F, Mattioli V, Annunziata MA. Posttraumatic growth and cancer: a study 5 years after treatment end. Support Care Cancer 2017; 25 (04) 1087-1096
- Schroevers MJ, Helgeson VS, Sanderman R, Ranchor AV. Type of social support matters for prediction of posttraumatic growth among cancer survivors. Psychooncology 2010; 19 (01) 46-53
- Thakur M, Gupta B, Kumar R. et al. Coping among women diagnosed with breast cancer with co-morbid depression: a study from North India. Delhi Psychiatry J. 2018; 21: 358-365
- Schreiber JA. Image of God: effect on coping and psychospiritual outcomes in early breast cancer survivors. Oncol Nurs Forum 2011; 38 (03) 293-301
- Lelorain S, Bonnaud-Antignac A, Florin A. Long term posttraumatic growth after breast cancer: prevalence, predictors and relationships with psychological health. J Clin Psychol Med Settings 2010; 17 (01) 14-22
- Dekel S, Ein-Dor T, Solomon Z. Posttraumatic growth and post-traumatic distress: a longitudinal study. Psychol Trauma 2012; 4 (01) 94
- Fromm K, Andrykowski MA, Hunt J. Positive and negative psychosocial sequelae of bone marrow transplantation: implications for quality of life assessment. J Behav Med 1996; 19 (03) 221-240
- Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychol 2003; 22 (05) 487-497
- Weiss T. Correlates of post-traumatic growth in married breast cancer survivors. J Soc Clin Psychol 2004; 23 (05) 733-746
- Jansen L, Hoffmeister M, Chang-Claude J, Brenner H, Arndt V. Benefit finding and post-traumatic growth in long-term colorectal cancer survivors: prevalence, determinants, and associations with quality of life. Br J Cancer 2011; 105 (08) 1158-1165
- Morris BA, Shakespeare-Finch J, Rieck M, Newbery J. Multidimensional nature of posttraumatic growth in an Australian population. J Trauma Stress 2005; 18 (05) 575-585
- Lovibond S.H., Lovibond P.F.. Manual for the Depression Anxiety Stress Scales. Psychology Foundation; Sydney, Australia: 1995


 PDF
PDF  Views
Views  Share
Share

