Persistent or recurrent Castleman?s disease - Look out for a lurking lymphoma!
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2011; 32(03): 162-164
DOI: DOI: 10.4103/0971-5851.92820
Abstract
Castleman′s disease, a rare condition of uncertain etiology clinically presents in isolated form or as a multicentric disease. The multicentric form can develop malignancies such as Kaposi′s sarcoma or lymphomas. We present a case of Castleman′s disease with coexisting interfollicular Hodgkin′s lymphoma that was confirmed by immunohistochemistry. This case report highlights the fact that an occult lymphoma has to be ruled out in persistent or recurrent Castleman′s disease.
Publication History
Article published online:
06 August 2021
© 2011. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Castleman's disease, a rare condition of uncertain etiology clinically presents in isolated form or as a multicentric disease. The multicentric form can develop malignancies such as Kaposi's sarcoma or lymphomas. We present a case of Castleman's disease with coexisting interfollicular Hodgkin's lymphoma that was confirmed by immunohistochemistry. This case report highlights the fact that an occult lymphoma has to be ruled out in persistent or recurrent Castleman's disease.
INTRODUCTION
Castleman's disease is a rare, non-neoplastic lympho-proliferative disorder of uncertain aetiology, wherein the age of onset, clinical presentation and the histological subtype vary markedly. Clinically, Castleman's disease can be classified into unicentric/unifocal or systemic/multifocal forms. Patients with Castleman's disease are at a high risk for the development of malignant lymphomas and Kaposi sarcoma. Hence, a regular medical surveillance is necessary in these cases. A review of literature shows that non-Hodgkin's lymphoma is seen more commonly in association with Castleman's disease; however, rarely Hodgkin's lymphoma can also occur.[1] We document here, a patient diagnosed as Castleman's disease, who later developed an interfollicularHodgkin's lymphoma on lymph node biopsy. The Hodgkin's lymphoma component was subtle and focal, which could have been missed if a high degree of suspicion had not allowed us to confirm the diagnosis by immunomarkers.
CASE REPORT
A 68-year-old hypertensive and diabetic lady presented with multiple bilateral cervical and axillary lymphadenopathy. Six months before this visit, she presented with a solitary left cervical lymphadenopathy which on excision biopsy showed features of hyaline-vascular type of Castleman's disease. Physical examination on the second visit revealed multiple bilateral cervical and left-sided axillary lymph nodes that were non-tender, discrete, firm in consistency and ranged in size from 0.5 to 8 cm. No organomegaly or constitutional symptoms were noted. Routine investigations such as complete blood count and biochemical profile (including hepatic function tests) were found to be within normal range except for mildly raised globulins (3.9 g/dl). Bone marrow aspiration done showed normal reactive marrow. Chest X-ray and computerized tomography (CT) scan of abdomen was normal. CT of thorax revealed left axillary adenopathy but mediastinum and lung fields were normal. Patient was seronegative for human immunodeficiency virus (HIV) by Western blot method.
Inspite of a course of antibiotics there was no reduction in lymphadenopathy in the 2nd visit. Hence clinically, a recurrent Castleman's disease was suspected and the largest axillary lymph node was excised and sent for histopathological confirmation. The biopsy showed partial effacement of lymph node architecture with expansion of paracortical and interfollicular regions.
Hyalinized follicles, interfollicular vascular proliferation and paracortical collection of plasma cells were also seen [Figure 1]. The interfollicular region showed polymorphous population of cells composed of eosinophils, neutrophils, plasma cells and binucleate/mononuclear atypical cells with abundant cytoplasm having inclusion like eosinophilic nucleoli with perinucleolar halo that resembled Reed-Sternberg (RS) cells [Figure 1, inset].
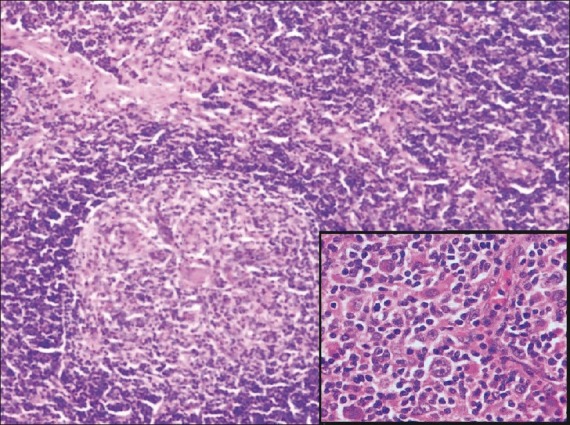
| Figure 1: Lymph node with interfollicular expansion and a large lymphoid follicle showing prominent hyalinised blood vessel within germinal centre (Hematoxylin and eosin stain ×40); Inset shows Reed-Sternberg cells (Hematoxylin and eosin stain ×400)
A panel of immunohistochemical (IHC) markers on tissue sections showed positivity for CD15 and CD30 with negative staining for CD 45 in RS-like cells and few background lymphocytes showed CD 20 positivity [Figure 2]. At this point, the previous lymph node biopsy sections were reviewed and no evidence of Hodgkin's disease was found. Correlating the clinical, histomorphology and immunohistochemistry, the final diagnosis of Castleman's disease (hyaline vascular type) with a coexistent interfollicular Hodgkin's lymphoma (Stage IIA) was arrived at.
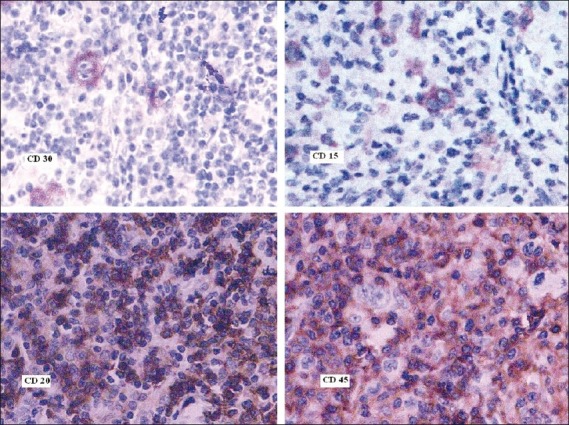
| Figure 2: Reed-Sternberg cells highlighted by positive staining with CD 15 and 30 and negative staining with CD45 while background lymphocytes are positive for CD20 (Immunostains: CD 30, CD15, CD20 and CD45 ×400)
The patient was given three cycles of chemotherapy with COPP (Cyclophosphamide, Oncovin, Procarbazine and Prednisolone). She developed hyperglycemia, hence the chemotherapeutic drugs were changed to ABVD (Adriamycin, Bleomycin, Vinblastine, Dicarbazine) regimen for the next three cycles. Patient is now in complete remission after 2 years of diagnosis and treatment.
DISCUSSION
Castleman's disease also termed as angiofollicular hyperplasia/giant lymph node hyperplasia is categorised into plasma cell, hyaline-vascular and mixed type on histopathology. Castleman's disease can mimic lymphoma clinically as it varies from the latter histologically and therapeutically, it is necessary to distinguish these two conditions. Castleman's disease may occur in lymph nodes involved by Hodgkin's lymphoma, resulting in a diagnostic dilemma. Castleman's-like histological features may also be seen as a part of a non-specific immune response to a variety of immunological stimuli including, Hodgkin's disease. Hence, a possibility of Hodgkin's disease needs to be considered and excluded before a conclusive diagnosis of Castleman's disease is made.[2]
The predominant pattern seen in this case was a hyaline vascular type of Castleman's disease which masked an underlying interfollicular Hodgkin's lymphoma. The suspicious RS-like cells in the lymph node showed positivity for CD15 and CD 30 but was negative for CD 45 thereby confirming a Hodgkin's lymphoma along with Castleman's disease.
Utilization of IHC stains proved to be a valuable tool in identifying the RS cells in our case. Zarate-Osorno documented similar cases exhibiting diagnostic problems in which IHC was useful in detecting the evidence of Hodgkin's lymphoma in Castleman's disease.[2] Likewise Maheswaran et al. reviewed cases previously diagnosed as Castleman's disease presenting later as Hodgkin's disease and IHC studies on these cases showed positivity for CD 15 and CD 30 indicating that a coexisting Hodgkin's was overlooked on initial biopsy.[3] In our case, previous lymph node biopsy showed only hyaline-vascular pattern of Castleman's disease with no evidence of Hodgkin's lymphoma.
The pathogenesis of Castleman's disease is complex. Recently Kaposi's sarcoma associated Herpes virus (also called Human Herpes virus – 8) was reported to be an etiological agent of Castleman's disease, especially in patients infected with HIV. The association of interleukin-6 (IL-6) in the evolution of Castleman's disease is suggested due to an increased IL-6 production by the germinal centres. Monoclonal antibody blocking the IL-6 receptor have shown clinical efficacy resulting in symptom resolution.[4] Several treatment protocols have been designed for Castleman's disease. In case of a localized disease, the options include excision of the affected lymph nodes and radiation. Corticosteroid, chemotherapy drugs and radiation therapy are treatment modalities available for multicentric disease. Targeting and deleting CD20-positive B cells, a prominent component of Castleman's disease, is a new immunotherapeutic approach which is responsible for the deregulated productions of human IL-6, vascular endothelial growth factor (VEGF) and other cytokines as well.[5]
Lymphoma occurring within the context of Castleman's disease should be treated with standard lymphoma chemotherapy regimen. Targeted therapy may be used against cytokines IL-2R and IL-6, the increased levels of which are responsible for characteristic B symptoms. Purging of CD20 positive cells using antiCD20 therapy might also be beneficial, since it deprives RS cells of a survival factor.[6] In our case, the patient responded well to COPP and ABVD therapy and after six cycles of chemotherapy, the patient is in complete remission for 2 years.
Rare cases of Hodgkin's lymphoma may present initially with a histological picture indistinguishable from Castleman's disease and the diagnosis may become evident only at a late stage. Therefore, before a final diagnosis of Castleman's disease is made, the lymph node must be scrutinised thoroughly for the subtle evidence of lymphoma using a panel of immunomarkers.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
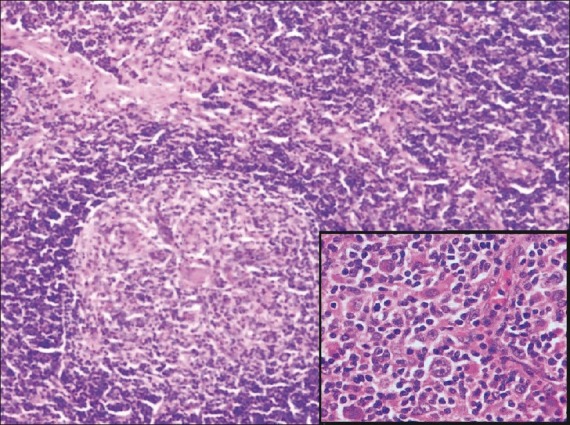
| Figure 1: Lymph node with interfollicular expansion and a large lymphoid follicle showing prominent hyalinised blood vessel within germinal centre (Hematoxylin and eosin stain ×40); Inset shows Reed-Sternberg cells (Hematoxylin and eosin stain ×400)
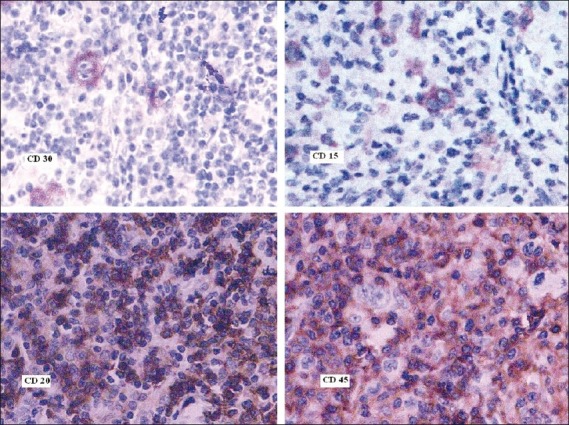
| Figure 2: Reed-Sternberg cells highlighted by positive staining with CD 15 and 30 and negative staining with CD45 while background lymphocytes are positive for CD20 (Immunostains: CD 30, CD15, CD20 and CD45 ×400)


 PDF
PDF  Views
Views  Share
Share

