Pancreatic Adenocarcinoma with Primary Tumor Calcification and Calcified Liver Metastasis: Report of a Rare Case and Review of Literature
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(05): 738-740
DOI: DOI: 10.4103/ijmpo.ijmpo_102_19
Abstract
Calcification is a feature of benign pancreatic diseases such as chronic calcific pancreatitis (CCP) or benign pancreatic tumors such as solid and papillary epithelial neoplasm of the pancreas and serous cystadenoma. The presence of calcification in a primary malignant pancreatic tumor is uncommon except for neuroendocrine tumors of the pancreas. Calcification in adenocarcinoma of the pancreas involving the primary tumor as well as the metastasis resulting thereof is extremely rare in the absence of CCP. To our knowledge, this is the first report of a case of primary adenocarcinoma of the pancreas that presented with calcification of the primary tumor as well as the metastatic liver nodules, accompanied by hypercalcemia.
Keywords
Calcified metastasis - hypercalcemia - pancreatic adenocarcinomaPublication History
Received: 21 April 2020
Accepted: 29 September 2020
Article published online:
17 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Calcification is a feature of benign pancreatic diseases such as chronic calcific pancreatitis (CCP) or benign pancreatic tumors such as solid and papillary epithelial neoplasm of the pancreas and serous cystadenoma. The presence of calcification in a primary malignant pancreatic tumor is uncommon except for neuroendocrine tumors of the pancreas. Calcification in adenocarcinoma of the pancreas involving the primary tumor as well as the metastasis resulting thereof is extremely rare in the absence of CCP. To our knowledge, this is the first report of a case of primary adenocarcinoma of the pancreas that presented with calcification of the primary tumor as well as the metastatic liver nodules, accompanied by hypercalcemia.
Keywords
Calcified metastasis - hypercalcemia - pancreatic adenocarcinomaIntroduction
It is common to find pancreatic calcification in chronic pancreatitis and benign pancreatic tumours. In adenocarcinoma, it is a rare phenomenon. Here we present a case, who had features of calcification of the primary as well as the metastatic sites, and associated with baseline hypercalcemia. This patient was subsequently treated with gemcitabine and nab-paclitaxel, to which he responded well. Tumour response was associated with increase in the calcification density. This case underlines the fact that presence of calcification can be a feature of high grade cancer also, and may be associated with hypercalcemia at presentation.
Case Report
A 63-year-old Indian male presented with upper abdominal discomfort for 2 months accompanied by weight loss and occasional vomiting for the same duration. There was no history of fever, altered bowel habit, hematemesis, or melena. His medical history was significant for diabetes mellitus for the last 20 years and hypothyroidism for the last 5 years, and he was on regular medications for both. He did not have any documented history of hyperparathyroidism. An ultrasound scan done elsewhere showed multiple space-occupying lesions in the liver. He was referred to us for further management.
On clinical examination, his vital signs were all normal and his Eastern Cooperative Oncology Group (ECOG) performance status was 2. Mild pallor was present. No nodes were palpable. Abdominal examination revealed mildly enlarged (two fingers below costal margin), hard liver with no tenderness. Skin examination revealed multiple tender erythematous nodules on the anterolateral aspect of both lower legs. The rest of the systemic examination was normal. At our hospital, the results of baseline investigations were as follows: hemoglobin 10.3 g/dl, total white blood cell count 10,700/mm3, and platelets 3.82 lakhs/mm3. Liver function tests revealed the following: bilirubin total 1.2 mg/dl, serum alanine aminotransferase 95 (21–72) U/L, serum aspartate aminotransferase 172 (17–59) U/L, gamma-glutamyl transferase 425 U/L (15–73 U/L), serum alkaline phosphatase 81 (38–126 U/L), albumin 2.7 g/dl, creatinine 0.72 mg/dl, urea 31 mg/dl, and calcium 9.2 g/dl (corrected 11 g/dl). Contrast-enhanced computed tomography (CECT) of the thorax and whole abdomen was done on December 11, 2018, which revealed multiple poorly defined hypoattenuating nodules in the liver with amorphous areas of calcifications [Figure 1a]. An ill-defined mass with nodular and amorphous calcification was noted in the uncinate process of the pancreas [Figure 1b]. The rest of the pancreatic parenchyma showed no calcification. There was no ductal dilatation or pancreatic parenchymal atrophy. Multiple nodes in the retroperitoneum were seen, with few showing calcifications, largest measuring 2.1 cm.
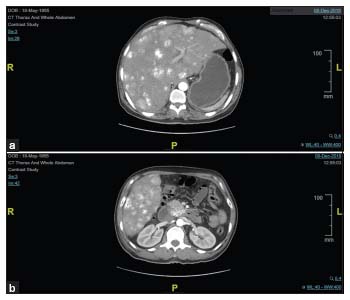
| Figure 1: (a) Calcified liver metastases along with multiple enhancing nodules distributed in the liver. (b) Calcified irregular enhancing mass in the head of the pancreas
Postcontrast image showed minimal enhancement in the liver nodules and pancreatic mass [Figure 1b]. The rest of the abdomen and thorax was unremarkable. A pancreatic primary neoplasm was considered. Serum CA 19-9 was 849 U/ml (normal limit < 27 U/ml). Ultrasound-guided biopsy from one of the liver nodules showed metastatic poorly differentiated carcinoma with areas of calcification, favoring adenocarcinoma. Immunohistochemistry showed diffuse positivity for cytokeratin (AE1/AE3) and CA 19-9, whereas it was negative for CK7, CK20, and p40. Fine-needle aspiration cytology was done from the skin nodules, which showed fat necrosis, inflammatory infiltrate composed of predominantly neutrophils, and foamy macrophages suggestive of erythema nodosum. A diagnosis of pancreatic adenocarcinoma with liver metastases was made.
He was managed for hypercalcemia with hydration and diuretics and was started on systemic chemotherapy with gemcitabine 1000 mg/m2 and nab-paclitaxel 125 mg/m2 given on days 1, 8 and 15, cycles repeated every 28 days. He was ECOG performance status 2 at presentation; therefore, mFOLFIRINOX was not offered. At the time of reporting of this case, he has completed three cycles of gemcitabine and nanoparticle albumin-bound paclitaxel and repeat CECT scan done on March 11, 2019, showed overall partial response. Interestingly, there was an increase in the density of calcification in the primary neoplasm as well as the metastatic lesions [Figure 2a and b]. His serum CA-19.9 level had decreased to 734 U/ml. His serum calcium level had decreased to 8.1 mg/dL and serum albumin level had increased to 3.3 gm/dl. At present, he is asymptomatic and doing well on chemotherapy.
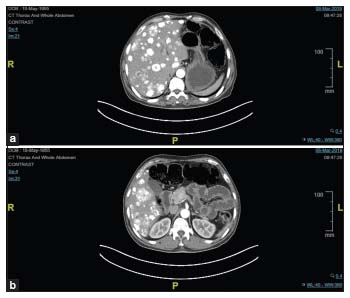
| Figure 2: (a) Increased calcification in the liver lesions. (b) Pancreatic mass showing regression in size
Review of literature
Calcification of pancreatic adenocarcinoma is reported when it occurs in the background of chronic calcific pancreatitis (CCP).[1] In the absence of CCP, calcification in pancreatic adenocarcinoma is very uncommon. Calcification is more commonly seen in benign pancreatic masses such as solid pseudopapillary epithelial neoplasm, serous cystadenoma, and mucinous cystic neoplasm. Malignant tumors of the pancreas that commonly show calcification are neuroendocrine tumors (NETs) and intraductal papillary mucinous neoplasm (IPMN).[2] The presence of calcification is correlated with poor prognosis and outcome.[3] NETs usually show strong enhancement on postcontrast images and malignant IPMN is associated with dilatation of main pancreatic duct; both of these findings were absent in this case. Rare primary tumors associated with calcification include acinar cell carcinoma,[4] liposarcoma, and chondrosarcoma.[5] Some case reports have described psammomatous calcification within the primary adenocarcinoma of the pancreas.[2] Another case report showed the presence of calcification in ductal adenocarcinoma after resection. In the same report, multiple kinds of bone morphogenetic protein (Types 5, 6, and 7) were also identified in the cytoplasm of carcinoma cells. Due to the rare occurrence, the clinicopathologic significance of this finding remains uncertain. Many such cases are a result of chronic pancreatitis, which is the primary cause of calcification.[6]
Calcification of liver metastases can occur either because of the histology of the primary tumor or due to the development of dystrophic calcification secondary to systemic chemotherapy or radiation. Mucinous adenocarcinoma of the gastrointestinal tract is the most common malignancy associated with calcified liver metastases. In this case, the metastatic lesions showed calcification before treatment. However, the amount of calcification increased following treatment, probably due to regression of tumor, causing calcifications to crowd together more closely, which suggests that the calcification was as a result of primary histology as well as dystrophic calcification.
To our knowledge, only five cases of intratumoral calcification have been reported, but no reports of metastatic calcification have been reported in literature for poorly differentiated adenocarcinoma.[2],[5],[7],[8],[9],[10],[11],[12],[13],[14] This is, as per our search results, the first case to be reported with such a clinicoradiological picture. Historically, baseline hypercalcemia is associated with poor prognosis in other solid tumors like the lung.
In summary, this is the first reported case of metastatic poorly differentiated adenocarcinoma of the pancreas with extensive calcification of both primary and the metastatic sites, with baseline hypercalcemia. Clinicians and radiologists should not discard the possibility of a primary pancreatic adenocarcinoma in the presence of a mildly enhancing calcified primary tumor and calcified metastatic liver nodules.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
References
- Mohamed Jr. A, Ayav A, Belle A, Orry X, Chevaux JB, Laurent V. Pancreatic cancer in patients with chronic calcifying pancreatitis: Computed tomography findings-A retrospective analysis of 48 patients. Eur J Radiol 2017; 86: 206-12
- Ohike N, Sato M, Kawahara M, Ohyama S, Morohoshi T. Ductal adenocarcinoma of the pancreas with psammomatous calcification. Report of a case. JOP 2008; 9: 335-8
- Poultsides GA, Huang LC, Chen Y, Visser BC, Pai RK, Jeffrey RB. et al. Pancreatic neuroendocrine tumors: Radiographic calcifications correlate with grade and metastasis. Ann Surg Oncol 2012; 19: 2295-303
- Xing-Mao Z, Hong-Juan Z, Qing L, Qiang H. Pancreatic acinar cell carcinoma-case report and literature review. BMC Cancer 2018; 18: 1083
- Manning MA, Paal EE, Srivastava A, Mortele KJ. Nonepithelial neoplasms of the pancreas, part 2: Malignant tumors and tumors of uncertain malignant potential from the radiologic pathology archives. Radiographics 2018; 38: 1047-72
- Campisi A, Brancatelli G, Vullierme MP, Levy P, Ruszniewski P, Vilgrain V. Are pancreatic calcifications specific for the diagnosis of chronic pancreatitis? A multidetector-row CT analysis. Clin Radiol 2009; 64: 903-11
- Schneider NI, Bauernhofer T, Schöllnast H, Ott A, Langner C. Pancreatic adenocarcinoma with multiple eosinophilic extracellular deposits consistent with noncalcified psammoma bodies. Virchows Arch 2011; 459: 623-5
- Kuroda N, Iwamura S, Fujishima N, Ohara M, Hirouchi T, Mizuno K. et al. Anaplastic carcinoma of the pancreas with rhabdoid features and hyaline globule-like structures. Med Mol Morphol 2007; 40: 168-71
- Takahashi T, Hatakeyama S, Machida T. Ductal adenocarcinoma of the pancreas with psammomatous calcification: Report of a case with immunohistochemical study for bone morphogenetic protein. Pathol Int 2011; 61: 603-7
- Gui T, Shen K. The epidermal growth factor receptor as a therapeutic target in epithelial ovarian cancer. Cancer Epidemiol 2012; 36: 490-6
- Kim T, Murakami T, Takahashi S, Hori M, Sakon M, Nakamori S. et al. Ductal adenocarcinoma of the pancreas with intratumoral calcification. Abdom Imaging 1999; 24: 610-3
- Kendig TA, Johnson RM, Shackford BC. Calcification pancreatic carcinoma. Ann Intern Med 1966; 65: 122-4
- Furukawa H, Takayasu K, Mukai K, Inoue K, Mizuguchi Y, Ushio K. et al. Ductal adenocarcinoma of the pancreas associated with intratumoral calcification. Int J Pancreatol 1995; 17: 291-6
- Haas O, Guillard G, Rat P, Friedman S, Favre JP. Pancreatic carcinoma developing in chronic pancreatitis: A report of four cases. Hepatogastroenterology 1990; 37: 350-1
Address for correspondence
Publication History
Received: 21 April 2020
Accepted: 29 September 2020
Article published online:
17 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
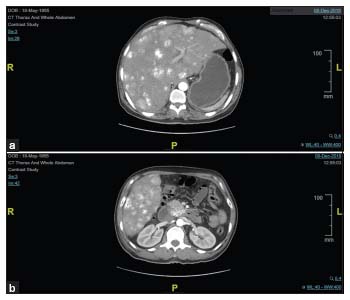
| Figure 1: (a) Calcified liver metastases along with multiple enhancing nodules distributed in the liver. (b) Calcified irregular enhancing mass in the head of the pancreas
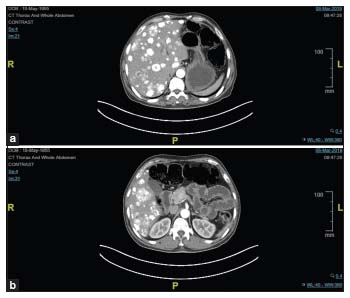
| Figure 2: (a) Increased calcification in the liver lesions. (b) Pancreatic mass showing regression in size
- 1 Mohamed Jr. A, Ayav A, Belle A, Orry X, Chevaux JB, Laurent V. Pancreatic cancer in patients with chronic calcifying pancreatitis: Computed tomography findings-A retrospective analysis of 48 patients. Eur J Radiol 2017; 86: 206-12
- 2 Ohike N, Sato M, Kawahara M, Ohyama S, Morohoshi T. Ductal adenocarcinoma of the pancreas with psammomatous calcification. Report of a case. JOP 2008; 9: 335-8
- 3 Poultsides GA, Huang LC, Chen Y, Visser BC, Pai RK, Jeffrey RB. et al. Pancreatic neuroendocrine tumors: Radiographic calcifications correlate with grade and metastasis. Ann Surg Oncol 2012; 19: 2295-303
- 4 Xing-Mao Z, Hong-Juan Z, Qing L, Qiang H. Pancreatic acinar cell carcinoma-case report and literature review. BMC Cancer 2018; 18: 1083
- 5 Manning MA, Paal EE, Srivastava A, Mortele KJ. Nonepithelial neoplasms of the pancreas, part 2: Malignant tumors and tumors of uncertain malignant potential from the radiologic pathology archives. Radiographics 2018; 38: 1047-72
- 6 Campisi A, Brancatelli G, Vullierme MP, Levy P, Ruszniewski P, Vilgrain V. Are pancreatic calcifications specific for the diagnosis of chronic pancreatitis? A multidetector-row CT analysis. Clin Radiol 2009; 64: 903-11
- 7 Schneider NI, Bauernhofer T, Schöllnast H, Ott A, Langner C. Pancreatic adenocarcinoma with multiple eosinophilic extracellular deposits consistent with noncalcified psammoma bodies. Virchows Arch 2011; 459: 623-5
- 8 Kuroda N, Iwamura S, Fujishima N, Ohara M, Hirouchi T, Mizuno K. et al. Anaplastic carcinoma of the pancreas with rhabdoid features and hyaline globule-like structures. Med Mol Morphol 2007; 40: 168-71
- 9 Takahashi T, Hatakeyama S, Machida T. Ductal adenocarcinoma of the pancreas with psammomatous calcification: Report of a case with immunohistochemical study for bone morphogenetic protein. Pathol Int 2011; 61: 603-7
- 10 Gui T, Shen K. The epidermal growth factor receptor as a therapeutic target in epithelial ovarian cancer. Cancer Epidemiol 2012; 36: 490-6
- 11 Kim T, Murakami T, Takahashi S, Hori M, Sakon M, Nakamori S. et al. Ductal adenocarcinoma of the pancreas with intratumoral calcification. Abdom Imaging 1999; 24: 610-3
- 12 Kendig TA, Johnson RM, Shackford BC. Calcification pancreatic carcinoma. Ann Intern Med 1966; 65: 122-4
- 13 Furukawa H, Takayasu K, Mukai K, Inoue K, Mizuguchi Y, Ushio K. et al. Ductal adenocarcinoma of the pancreas associated with intratumoral calcification. Int J Pancreatol 1995; 17: 291-6
- 14 Haas O, Guillard G, Rat P, Friedman S, Favre JP. Pancreatic carcinoma developing in chronic pancreatitis: A report of four cases. Hepatogastroenterology 1990; 37: 350-1


 PDF
PDF  Views
Views  Share
Share

