Oral Verrucous Carcinoma: Ten Year Experience from a Tertiary Care Hospital in India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(04): 452-455
DOI: DOI: 10.4103/ijmpo.ijmpo_153_16
Abstract
Background: Verrucous carcinoma of the oral cavity (OVC) is an uncommon variant of oral squamous cell carcinoma (OSCC). The clinical presentation and surgical outcomes of OVC are unique; however, the management protocols for OVC are largely extrapolated from OSCC. Objectives: The aim is to study the clinical, histopathological demographics, and outcome of OVC at a tertiary care referral hospital in South India. To study the need for lymph node dissection and the role of adjuvant therapy for close resection margins. Materials and Methods: A retrospective review of all patients diagnosed to have OVC between January 2005 and April 2015 was undertaken. Data were collected from hospital records and telephonic interview when possible. Results: Thirty patients were diagnosed to have OVC. The mostcommon site of the presentation was the buccal mucosa. Twenty-three patients had wide local excision of the primary tumor and seven patients had neck dissection as well. None of the patients who underwent neck dissection had node-positive disease pathologically. The margins were considered close in nine patients, only one of these patients received adjuvant radiation therapy; despite among the patients with close resection margins, there was no recurrence or disease-related mortality. Among the thirty patients, there was only one patient who had recurred locally and there was no disease associated mortality. Conclusions: OVC is a unique variant of OSCC which has a good prognosis. Routine lymphadenectomy can be avoided.
Publication History
Article published online:
04 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used forcommercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Background:
Verrucous carcinoma of the oral cavity (OVC) is an uncommon variant of oral squamous cell carcinoma (OSCC). The clinical presentation and surgical outcomes of OVC are unique; however, the management protocols for OVC are largely extrapolated from OSCC.
Objectives:
The aim is to study the clinical, histopathological demographics, and outcome of OVC at a tertiary care referral hospital in South India. To study the need for lymph node dissection and the role of adjuvant therapy for close resection margins.
Materials and Methods:
A retrospective review of all patients diagnosed to have OVC between January 2005 and April 2015 was undertaken. Data were collected from hospital records and telephonic interview when possible.
Results:
Thirty patients were diagnosed to have OVC. The most common site of the presentation was the buccal mucosa. Twenty-three patients had wide local excision of the primary tumor and seven patients had neck dissection as well. None of the patients who underwent neck dissection had node-positive disease pathologically. The margins were considered close in nine patients, only one of these patients received adjuvant radiation therapy; despite among the patients with close resection margins, there was no recurrence or disease-related mortality. Among the thirty patients, there was only one patient who had recurred locally and there was no disease associated mortality.
Conclusions:
OVC is a unique variant of OSCC which has a good prognosis. Routine lymphadenectomy can be avoided.
Introduction
Oral verrucous carcinoma (OVC) is an uncommon variant of oral squamous cell carcinoma (OSCC). The incidence of VC of the oral cavity is between 2% and 16% of all oral cancers.[1] The demographics, clinical presentation, and surgical outcomes of VC are believed to be different from OSCC.[2] They are generally considered as slow growing tumors with good prognosis. The management of OVC is rarely radical or multi-modal.[3] Even with local tumor aggression, it is intriguing that regional or distant metastasis is rare.[4] Despite these differences, most guidelines and treatment protocols do not differentiate between OVC and OSCC with respect to the margins of excision, need for adjuvant therapy, or the role and extent of lymph node dissection.
This paper analyses the demographics and outcomes of surgically treated VC of the oral cavity over a 10-year period at a head and neck surgical unit at a tertiary care referral center in South India.
Materials And Methods
A retrospective chart review of patients diagnosed to have OVC between January 2005 and April 2015 was done. The study was conducted in the Department of head and neck surgery of a tertiary care hospital in India. An institutional review board approval was obtained for this study.
Staging and management of the disease were done based on the American joint committee on cancer 7th edition guidelines for oral carcinoma.[5] The clinical and histopathological data, treatment modality/modalities, and outcomes (overall survival and disease-free survival) were collected from the clinical workstation database. Telephonic interview and electronic medical records were used to follow up the patients.
The data collected was analyzed using SPSS® software for windows version 16.0. Chicago, SPSS Inc. Individual variables were checked for statistical significance using Chi-square and Fisher's exact test for categorical variables and continuous variables were analyzed using t-test.
Results
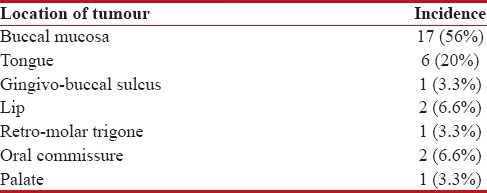
One thousand and forty-nine patients were operated for OSCC over a 10-year period. Thirty patients (2.86%) were diagnosed to have OVC during the study. Twenty-five patients (83%) were male and five (17%) were female with a male: female ratio of 5:1. The mean age at presentation was 49 years (range: 41–76 years, standard deviation 8.75). Ten patients (33.3%) with VC chewed tobacco, eight (26.6%) had chewed and smoked tobacco; three (10%) only smoked tobacco whereas the remaining nine patients did not consume tobacco in any form. The average duration of symptoms before undergoing definitive surgery for OVC was 20 months (range: 4–120 months). Distribution of primary tumors by epicenter at presentation is depicted in Table 1.
Table 1
Location of epicentre of tumour within the oral cavity
|
Six of the thirty patients (20%) required multiple biopsies at different time periods before undergoing wide local excision; most of the patients had a single pre-operative biopsy following which the patient underwent an oncological operation. Thirteen of the thirty patients had biopsy proven malignancy pre-operatively, atypical and dysplastic features were seen in nine patients. The rest had benign pre-operative histopathology but underwent wide local excision based on clinical suspicion [Table 2].
Table 2
Pre-operative histopathology

|
On clinical staging, 6 (20%) had T1, 15 (50%) had T2, and 9 (30%) were T3, but none of the patients in this series presented with T4 tumor. Five patients had significant neck nodes (clinically and radiologically) pre-operatively. Wide local excision was performed in all patients, and neck dissection was done in 7 patients. Five of the seven patients had significant neck nodes (clinical and radiologically) pre-operatively and two of the seven patients had neck dissection based on the characteristics of the primary tumor and after discussion in the multidisciplinary tumor (MDT) board. Following neck dissection, the final histopathology revealed that none of these patients had node positive disease. None of the patients had either lymphovascular invasion or perineural invasion or bone invasion or distant metastasis. Among the thirty patients with OVC, four had hybrid VC (non-verrucous SCC that arises synchronously with the OVC). A total of nine patients (30%) had close margins, and four patients (14%) had positive margins [Table 3]. All these patients were recommended adjuvant therapy as dictated by the tumor characteristics following a discussion in the MDT.
Table 3
Margins of resection
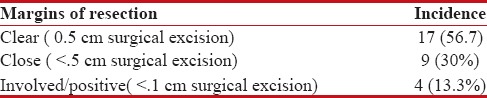
| Among the nine patients with close margins, only one patient received adjuvant radiation therapy, six of these patients were followed up and there was no recurrence or mortality in this cohort of patients.
Among the four patients with positive/involved margins, two were followed up and one recurred locally (this patient also had hybrid VC). They had all received adjuvant radiation therapy; re-excision was not done for any of these patients.
Overall follow up was available for 22 patients. The median follow up was 24 months during which period one patient (4.6%) developed local recurrence. This patient was found to have hybrid VC and positive resection margin. There were no regional recurrences or disease-related mortality.
VC is described as any exophytic growth of well-differentiated squamous cell carcinoma which generally present as white, warty lesions.[6,7] They are slow growing tumors known to have low metastatic potential with good prognosis.[8]
In this retrospective review of 1049 patients that underwent surgical treatment for oral cancer, 30 patients were diagnosed to have OVC. The prevalence of OVC in our institution is toward the low end (2.86%) of the range of 2%–16% reported in the literature.[1] Rekha and Angadi studied 133 cases of VC and concluded that they account for 16.08% of OSCC with a greater predilection for males and buccal mucosa. Walvekar et al. studied 101 cases of OVC and confirmed buccal mucosa as the most common subsite with the association of tobacco chewing.[4] Buccal mucosa was the most common subsite for OVC in our series, and 18 out of 30 patients had a history of tobacco chewing.
Lesions with a “verrucous” surface may belong to a spectrum extending from verrucous hyperplasia (VH), pseudoepithelial hyperplasia, proliferative verrucous leukoplakia (PVL) VC to hybrid OVC.[8,9] Pre-operative histopathological evaluation is not always accurate, or representative and a high degree of clinical suspicion is required to diagnose and treat this disease entity.[9,10]
In the present study, 6 patients (20%) had multiple biopsies before the diagnosis. Interestingly, 8 patients (26%) had benign preoperative incision biopsy/biopsies, and 3 patients (10%) had dysplasia in the preoperative histopathological assessment, and 4 (13%) had hybrid OVC which was not diagnosed preoperatively.
VH is pathologically described as an overgrowth of the differentiated keratinized epithelium. Proliferative PVL is similar to VH with the addition of dysplastic or atypical features. VC, on the other hand, has the above-mentioned features and also the pathognomonic destructive pushing border at its interface with connective tissue. However, the basement membrane is intact. Hybrid VC has a VC plus an element of SCC as evidenced by the destruction of the basement.[10,11] Multiple biopsies from multiple sites, is the usual practice due to the numerous disease entities that display verrucous appearance. Most authorities suggest that hyperplasia can be best differentiated from VC in biopsies taken from the margins of the tumor.[8]
As it is clinically difficult to differentiate these lesions preoperatively, it is generally recommended that all verrucous lesions in patients be surgically excised.[11]
The surgical dilemma is two-fold – if the preoperative biopsy is reported as VH/PVL is there an element of VC that has not been sampled? If the biopsy report is VC, is there an element of Hybrid OVC or SCC that has not been sampled. Authors observed that 51% of incision biopsies failed to answer these questions despite advances in molecular and genetic studies, flow cytometry and immune-histochemical analysis. Accurate diagnosis is possible only after definitive surgery.[8]
The extent of the surgery (margins) and need for neck dissection may need to be re-discussed after the primary surgery if there is a histological surprise. Re-doing a surgery may be challenging if a complex reconstruction (especially microvascular) was done during the primary surgery. Due to the rare nature of the disease, consensus guidelines discussing these issues are not available.
Surgical excision with adequate margins has proven to be effective in the management of these tumours and radiotherapy has generally been recommended in the presence of adverse risk factors in the Histopathology report.[12,13]
In our series, only 5 (16%) had clinically palpable nodes and underwent therapeutic neck dissection, two additional patients underwent neck dissection based on strong clinical suspicion and MDT board recommendations. However, all the neck dissection specimens were pathologically negative. Walvekar et al. showed that ¼th of their patients presented with palpable nodes and none had pathologically node-positive disease.[4] They concluded that most enlarged lymph nodes at presentation are often reactive to a secondary infection or inflammation. Reported case series with node-positive disease could be a variant of VC with an invasive component (hybrid variety).[6] It is reasonable to omit neck dissection in confirmed VC cases or consider a selective neck treatment such as a supraomohyoid neck dissection (SOHND) in situations where there is uncertainty regarding the pathological diagnosis in the face of clinically suspicious lymphadenopathy. Alternatively, a staged neck procedure is also a reasonable option if final tumor histology mandates it.
Most surgeons agree that margins are considered “close” if margins excised is <0 href="https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5759063/#ref14" rid="ref14" class=" bibr popnode tag_hotlink tag_tooltip" id="__tag_659253011" role="button" aria-expanded="false" aria-haspopup="true" xss=removed>14] In the present study, close margins were present in nine patients. The patients with close margins were reviewed in the MDT postoperatively and were recommended adjuvant radiation therapy. Only one patient completed the adjuvant radiation therapy. None of them recurred. The role of adjuvant radiation therapy in OVC is reserved for patients similar to squamous cell carcinoma of the oral cavity.[1] Six of these patients were followed up with a mean follow up of 27 months. The long-term survival of these patients was however excellent with no local recurrences or disease-related mortality. This is in contradistinction to OSCC where close margins are considered to be a poor prognostic factor with recurrence rates exceeding 50%.[14,15,16] This raises the obvious question as to what margin is acceptable for OVC and whether we need to give margins of excision similar to OSCC. Whether close margins can be kept on follow-up without radiotherapy is to be discussed. Positive resection margins significantly affect local recurrence. However, the association of close margin and tumour recurrence of OVC has not been discussed in literature available.[4]
Although some studies have reported 28% local recurrence rates for OVC; various other studies did not reveal such a high recurrence rate.[4,10,17] Only one patient in our series recurred locally (this patient had hybrid OVC). This is in contrast to OSCC where more than a third of all patients recur locally.[16,18] The overall prognosis of OVC has generally been considered to be good with overall survival rates exceeding 80%.[1,4,11] This is much higher than what is seen in OSCC.[18,19]
The existing guidelines for OSCC are followed for managing OVC, especially in deciding adequate margins for surgical excision, adjuvant therapy, and the role of lymphadenectomy. However, the pathology and clinical outcomes of OVC are different as evident in the above discussion.
Limitations
This is a retrospective study with a median follow up of 24 months.
VC of the oral cavity is a distinct clinical entity with good prognosis. Surgical excision with wide margins and appropriate reconstruction yields a good outcome. Palpable neck nodes are usually reactive/inflammatory and neck dissection could be avoided or limited to SOHND in selective cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Rekha KP, Angadi PV. Verrucous carcinoma of the oral cavity: A clinico-pathologic appraisal of 133 cases in Indians. Oral Maxillofac Surg 2010;14:211-8.
- Alkan A, Bulut E, Gunhan O, Ozden B. Oral verrucous carcinoma: A study of 12 cases. Eur J Dent 2010;4:202-7.
- Terada T. Verrucous carcinoma of the oral cavity: A histopathologic study of 10 Japanese cases. J Maxillofac Oral Surg 2011;10:148-51.
- Walvekar RR, Chaukar DA, Deshpande MS, Pai PS, Chaturvedi P, Kakade A, et al. Verrucous carcinoma of the oral cavity: A clinical and pathological study of 101 cases. Oral Oncol 2009;45:47-51.
- AJCC Cancer Staging Manual | Springer. Available from: http://www.springer.com/in/book/9780387884400. [Last accessed on 2015 Jun 22].
- Jordan RC. Verrucous carcinoma of the mouth. J Can Dent Assoc 1995;61:797-801.
- Sadasivan A, Thankappan K, Rajapurkar M, Shetty S, Sreehari S, Iyer S, et al. Verrucous lesions of the oral cavity treated with surgery: Analysis of clinico-pathologic features and outcome. Contemp Clin Dent 2012;3:60-3.
- Gokavarapu S, Chandrasekhara Rao LM, Patnaik SC, Parvataneni N, Raju KV, Chander R, et al. Reliability of incision biopsy for diagnosis of oral verrucous carcinoma: A Multivariate clinicopathological study. J Maxillofac Oral Surg 2015;14:599-604.
- Garcia NG, Oliveira DT, Hanemann JA, Pereira AA. Oral verrucous carcinoma mimicking a chronic candidiasis: A case report. Case Rep Oncol Med 2012;2012:190272.
- Mehrotra D, Goel M, Kumar S, Pandey R, Ram H. Oral verrucous lesions: Controversies in diagnosis and management. J Oral Biol Craniofac Res 2012;2:163-9.
- Depprich RA, Handschel JG, Fritzemeier CU, Engers R, Kübler NR. Hybrid verrucous carcinoma of the oral cavity: A challenge for the clinician and the pathologist. Oral Oncol Extra 2006;42:85-90.
- Huang SH, Lockwood G, Irish J, Ringash J, Cummings B, Waldron J, et al. Truths and myths about radiotherapy for verrucous carcinoma of larynx. Int J Radiat Oncol Biol Phys 2009;73:1110-5.
- Devaney KO, Ferlito A, Rinaldo A, El-Naggar AK, Barnes L. Verrucous carcinoma (carcinoma cuniculatum) of the head and neck: What do we know now that we did not know a decade ago? Eur Arch Otorhinolaryngol 2011;268:477-80.
- Nason RW, Binahmed A, Pathak KA, Abdoh AA, Sándor GK. What is the adequate margin of surgical resection in oral cancer? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:625-9.
- ;Eldeeb H, Macmillan C, Elwell C, Hammod A. The effect of the surgical margins on the outcome of patients with head and neck squamous cell carcinoma: Single institution experience. Cancer Biol Med 2012;9:29-33.
- Dillon JK, Brown CB, McDonald TM, Ludwig DC, Clark PJ, Leroux BG, et al. How does the close surgical margin impact recurrence and survival when treating oral squamous cell carcinoma? J Oral Maxillofac Surg 2015;73:1182-8.
- Candau-Alvarez A, Dean-Ferrer A, Alamillos-Granados FJ, Heredero-Jung S, García-García B, Ruiz-Masera JJ, et al. Verrucous carcinoma of the oral mucosa: An epidemiological and follow-up study of patients treated with surgery in 5 last years. Med Oral Patol Oral Cir Bucal 2014;19:e506-11.
- Wang B, Zhang S, Yue K, Wang XD. The recurrence and survival of oral squamous cell carcinoma: A report of 275 cases. Chin J Cancer 2013;32:614-8.
- Oral Cancer 5-Year Survival Rates by Race, Gender, and Stage of Diagnosis. Available from: http://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/OralCancer/OralCancer5 YearSurvivalRates.htm. [Last accessed on 2015 Oct 05].
References
- Rekha KP, Angadi PV. Verrucous carcinoma of the oral cavity: A clinico-pathologic appraisal of 133 cases in Indians. Oral Maxillofac Surg 2010;14:211-8.
- Alkan A, Bulut E, Gunhan O, Ozden B. Oral verrucous carcinoma: A study of 12 cases. Eur J Dent 2010;4:202-7.
- Terada T. Verrucous carcinoma of the oral cavity: A histopathologic study of 10 Japanese cases. J Maxillofac Oral Surg 2011;10:148-51.
- Walvekar RR, Chaukar DA, Deshpande MS, Pai PS, Chaturvedi P, Kakade A, et al. Verrucous carcinoma of the oral cavity: A clinical and pathological study of 101 cases. Oral Oncol 2009;45:47-51.
- AJCC Cancer Staging Manual | Springer. Available from: http://www.springer.com/in/book/9780387884400. [Last accessed on 2015 Jun 22].
- Jordan RC. Verrucous carcinoma of the mouth. J Can Dent Assoc 1995;61:797-801.
- Sadasivan A, Thankappan K, Rajapurkar M, Shetty S, Sreehari S, Iyer S, et al. Verrucous lesions of the oral cavity treated with surgery: Analysis of clinico-pathologic features and outcome. Contemp Clin Dent 2012;3:60-3.
- Gokavarapu S, Chandrasekhara Rao LM, Patnaik SC, Parvataneni N, Raju KV, Chander R, et al. Reliability of incision biopsy for diagnosis of oral verrucous carcinoma: A Multivariate clinicopathological study. J Maxillofac Oral Surg 2015;14:599-604.
- Garcia NG, Oliveira DT, Hanemann JA, Pereira AA. Oral verrucous carcinoma mimicking a chronic candidiasis: A case report. Case Rep Oncol Med 2012;2012:190272.
- Mehrotra D, Goel M, Kumar S, Pandey R, Ram H. Oral verrucous lesions: Controversies in diagnosis and management. J Oral Biol Craniofac Res 2012;2:163-9.
- Depprich RA, Handschel JG, Fritzemeier CU, Engers R, Kübler NR. Hybrid verrucous carcinoma of the oral cavity: A challenge for the clinician and the pathologist. Oral Oncol Extra 2006;42:85-90.
- Huang SH, Lockwood G, Irish J, Ringash J, Cummings B, Waldron J, et al. Truths and myths about radiotherapy for verrucous carcinoma of larynx. Int J Radiat Oncol Biol Phys 2009;73:1110-5.
- Devaney KO, Ferlito A, Rinaldo A, El-Naggar AK, Barnes L. Verrucous carcinoma (carcinoma cuniculatum) of the head and neck: What do we know now that we did not know a decade ago? Eur Arch Otorhinolaryngol 2011;268:477-80.
- Nason RW, Binahmed A, Pathak KA, Abdoh AA, Sándor GK. What is the adequate margin of surgical resection in oral cancer? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:625-9.
- ;Eldeeb H, Macmillan C, Elwell C, Hammod A. The effect of the surgical margins on the outcome of patients with head and neck squamous cell carcinoma: Single institution experience. Cancer Biol Med 2012;9:29-33.
- Dillon JK, Brown CB, McDonald TM, Ludwig DC, Clark PJ, Leroux BG, et al. How does the close surgical margin impact recurrence and survival when treating oral squamous cell carcinoma? J Oral Maxillofac Surg 2015;73:1182-8.
- Candau-Alvarez A, Dean-Ferrer A, Alamillos-Granados FJ, Heredero-Jung S, García-García B, Ruiz-Masera JJ, et al. Verrucous carcinoma of the oral mucosa: An epidemiological and follow-up study of patients treated with surgery in 5 last years. Med Oral Patol Oral Cir Bucal 2014;19:e506-11.
- Wang B, Zhang S, Yue K, Wang XD. The recurrence and survival of oral squamous cell carcinoma: A report of 275 cases. Chin J Cancer 2013;32:614-8.
- Oral Cancer 5-Year Survival Rates by Race, Gender, and Stage of Diagnosis. Available from: http://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/OralCancer/OralCancer5 YearSurvivalRates.htm. [Last accessed on 2015 Oct 05].


 PDF
PDF  Views
Views  Share
Share

