Non-Hodgkin's lymphoma "masquerading" as Pott's disease in a 13-year old boy
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2011; 32(02): 101-104
DOI: DOI: 10.4103/0971-5851.89793
Abstract
Lymphomas are malignant neoplasms of the lymphoid lineage. They are broadly classified as either Hodgkin disease or as non-Hodgkin lymphoma (NHL). Burkitt′s lymphoma, a variety of NHL, is significantly most common in sub-Saharan Africa, where it accounts for approximately one half of childhood cancers. Lymphoblastic lymphoma is less common. A case of paravertebral high grade non-Hodgkin′s lymphoma (lymphoblastic lymphoma) "masquerading" as Pott′s disease in a 13-year-old child is reported. The present report was informed by the unusual presentation of this case and the intent of increasing the index of diagnostic suspicion. A brief appraisal is provided of the clinical parameters, management strategies and challenges. AT was a 13-year boy that presented on account of a slowly evolving and progressively increasing hunch on the back and inability to walk over 4 and 8 months duration, respectively. There was subsequent inability to control defecation and urination. There was no history of cough. He and his twin brother lived with their paternal grandfather who had chronic cough with associated weight loss. The grandfather died shortly before the child′s admission. The child had no BCG immunization. The essential findings on examination were in keeping with lower motor neurons (LMN) paralysis of the lower limbs. The upper limbs appeared normal. There was loss of cutaneous sensation from the umbilicus (T10) downward. There was a firm, (rather tense), non-tender non-pulsatile, smooth swelling over the mid-third of the back (T6-L1) the mass had no differential warmth. It measures about 20×12 cm. Chest radiograph showed no active focal lung lesion, but the thoraco-lumbar spine showed a vertebral planner at L1 and a wedged collapse of T11-T12 vertebrae. There was sclerosis of the end plates of all the vertebral bodies with associated reduction in the bone density. He had an excision biopsy on the 90th day on admission, following which his clinical state rapidly deteriorated. He died within 48 h post surgery. This report aims at raising the local index of clinical suspicion by highlighting the reality of rarities, even in the presence of inadequate diagnostic facilities!
Publication History
Article published online:
06 August 2021
© 2011. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Lymphomas are malignant neoplasms of the lymphoid lineage. They are broadly classified as either Hodgkin disease or as non-Hodgkin lymphoma (NHL). Burkitt's lymphoma, a variety of NHL, is significantly most common in sub-Saharan Africa, where it accounts for approximately one half of childhood cancers. Lymphoblastic lymphoma is less common. A case of paravertebral high grade non-Hodgkin's lymphoma (lymphoblastic lymphoma) “masquerading” as Pott's disease in a 13-year-old child is reported. The present report was informed by the unusual presentation of this case and the intent of increasing the index of diagnostic suspicion. A brief appraisal is provided of the clinical parameters, management strategies and challenges. AT was a 13-year boy that presented on account of a slowly evolving and progressively increasing hunch on the back and inability to walk over 4 and 8 months duration, respectively. There was subsequent inability to control defecation and urination. There was no history of cough. He and his twin brother lived with their paternal grandfather who had chronic cough with associated weight loss. The grandfather died shortly before the child's admission. The child had no BCG immunization. The essential findings on examination were in keeping with lower motor neurons (LMN) paralysis of the lower limbs. The upper limbs appeared normal. There was loss of cutaneous sensation from the umbilicus (T10) downward. There was a firm, (rather tense), non-tender non-pulsatile, smooth swelling over the mid-third of the back (T6-L1) the mass had no differential warmth. It measures about 20×12 cm. Chest radiograph showed no active focal lung lesion, but the thoraco-lumbar spine showed a vertebral planner at L1 and a wedged collapse of T11-T12 vertebrae. There was sclerosis of the end plates of all the vertebral bodies with associated reduction in the bone density. He had an excision biopsy on the 90th day on admission, following which his clinical state rapidly deteriorated. He died within 48 h post surgery. This report aims at raising the local index of clinical suspicion by highlighting the reality of rarities, even in the presence of inadequate diagnostic facilities!
INTRODUCTION
Lymphomas are malignant neoplasms of lymphoid lineage. They are broadly classified as either Hodgkin disease or as non-Hodgkin lymphoma (NHL).[1] Most childhood non-Hodgkin lymphomas can be classified as one of the following types: (i) lymphoblastic lymphomas (of T-cell), (ii) small noncleaved cell lymphomas (SNCCLs) that are subdivided into Burkitt (common in children) and non-Burkitt (in adults) subtypes and (iii) large cell lymphomas (LCLs).[1,2]
Burkitt's lymphoma, a variety of NHL, is significantly most common in sub-Saharan Africa, where it accounts for approximately one half of childhood cancers.[3] Lymphoblastic lymphoma is less common. A 13-year-old boy with an unusual presentation of lymphoblastic lymphoma is described.
CASE REPORT
A.T. was a 13-year old, first of a set of male twins. He presented at the Emergency Paediatric Unit (EPU) of the University of Ilorin Teaching Hospital (UITH) on account of swelling on the back and inability to walk, both of progressive curse over 4 and 8 months, respectively. He was apparently well until 8 months prior to presentation when he started complaining of non-radiating dull upper back pain. The pain did not disturb him from routine daily activities initially, but later became severe especially while walking. There was no preceding physical trauma. Slow evolving and progressively increasing hunch on the back was noted about 4 months later. Weakness of the lower limbs and falling when walking, with subsequent inability to walk followed later. The loss of ability to control defecation and urination occurred by the fourth month of the illness. There was associated low grade, but intermittent, fever with spikes mostly in the evenings. There was poor appetite and progressive weight loss since the onset of the illness. There is no history of cough. He and his twin brother lived with their paternal grandfather who had chronic cough with associated weight loss. The grandfather died shortly before the child's admission. The child had no BCG immunization, his genotype was not known, his blood group was O; Rhesus positive. His father was a bricklayer, while his mother was a food vendor.
Examination revealed an ill-looking emaciated boy. He had no fever; temperature for most part of the 3 months of admission ranged between 36.4°C and 37.1°C. He was not pale, there was no peripheral lymphadenopathy and no finger clubbing. The essential findings were in the musculoskeletal system, namely the lower limbs appeared wasted and the power was grade 0; other features of lower motor neurons (LMN) paralysis were positive. The upper limbs appeared normal. There was a firm, (rather tense), non-tender non-pulsatile, smooth swelling over the mid-third of the back (T6-L1) the mass had no differential warmth. It measured about 20 cm by 12 cm. There was loss of anal sphincteric tone and reflex and loss of cutaneous sensation from the umbilicus (T10) downward.
Investigations
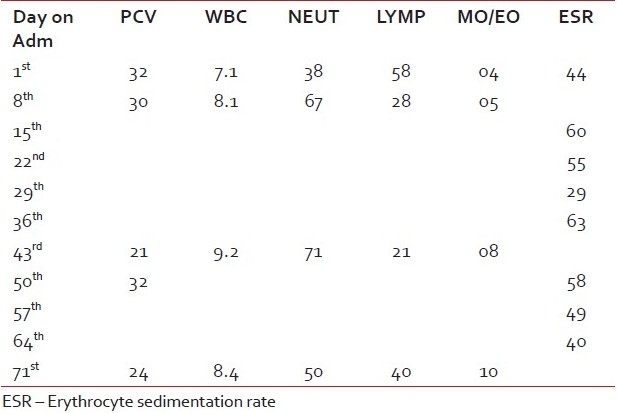
Chest radiograph showed no active focal lung lesion, but the thoraco-lumbar spine showed a vertebral planner at L1 and a wedged collapse of T11-T12 vertebrae. There was sclerosis of the end plates of all the vertebral bodies with associated reduction in the bone density [Figures [Figures11 and and2].2]. The initial diagnosis was hemiplegia complicating thoraco-lumbar spine tuberculosis (Pott's disease) secondary to spinal cord compression. He had 3 months of anti-tuberculous therapy consisting of daily rifampicin, isoniazid and pyrazinamide, with streptomycin included in the first 6 weeks. Adjunct therapy includes thoraco-lumbar jacket and limbs physiotherapy. But there was no significant improvement clinically or on repeat radiographs. He had a persistently elevated erythrocyte sedimentation rate (ESR) throughout the admission period [Table 1]. Abdominal ultrasound at the sixth week on admission showed huge and extensive para-aortic lymph nodes, matted together. He had an excision biopsy on the 90th day on admission, following which his clinical state rapidly deteriorated. He died within 48 h post surgery.
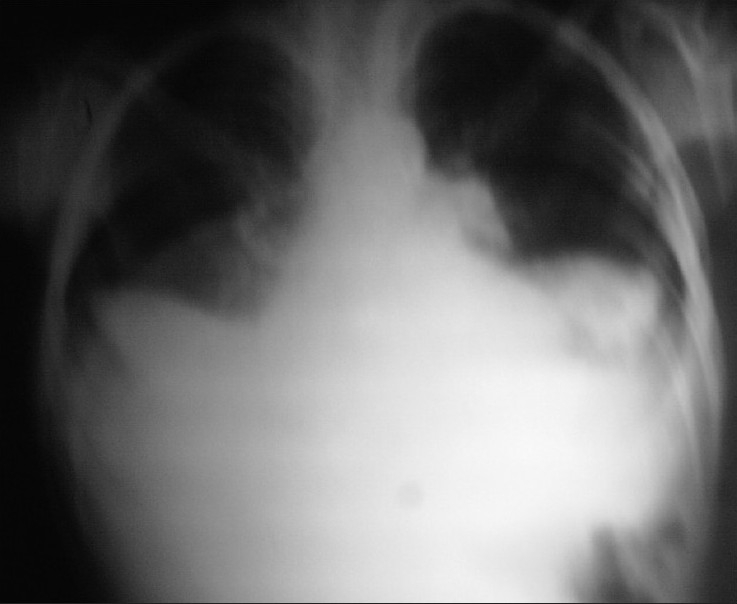
| Fig. 1 Chest radiograph showed no active focal lung lesion
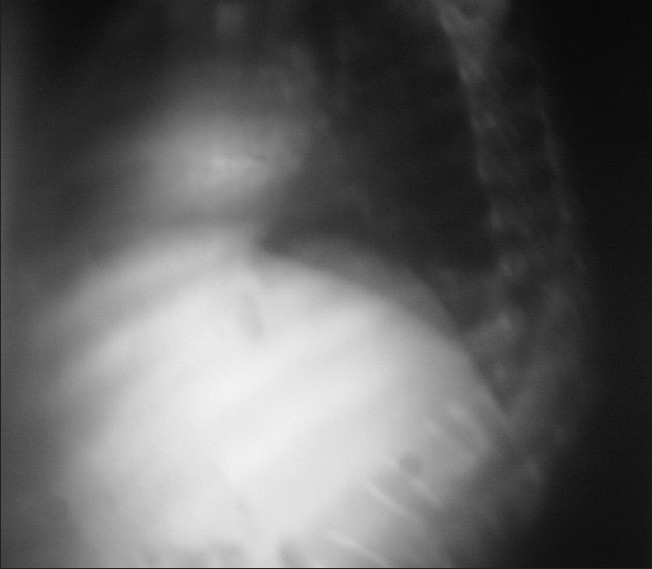
| Fig. 2 The thoraco-lumber spine showed a vertebral planner at L1 and a wedged collapse of T11-T12 vertebrae
Table 1
Some hematologic results during the 92 days on admission
A post-mortem histology report showed sheets of medium-sized malignant lymphoid cells interspersed by macrophages to give a “starry sky appearance.” The cells contained round to oval hyperchromatic vascular nuclei, prominent nucleoli and scanty cytoplasm. Numerous mitoses and thin-walled vascular channels werealso present.
A final histopathologic diagnosis of paravertebral high grade non Hodgkin's lymphoma (lymphoblastic lymphoma) was then made.
DISCUSSION
The present report describes, to our knowledge, the first patient with lymphoblastic lymphoma originating as a paraspinal mass accompanied by complete paraplegia (following a collapse of the vertebrae). The child presented with neither an anterior mediastinal mass nor lymphadenopathy, the two most presenting form of lymphoblastic lymphoma.[4,5] The positive history of contact with a close relative (paternal grandfather) who had chronic cough with associated weight loss and died shortly before the child's admission warranted an initial diagnosis of Pott's disease in this patient.
Although the age of this patient is in favor of non-Hodgkin lymphoma,[3] the relatively long duration of symptoms and the findings on the imaging studies are also part of the “red herrings.” Non-Hodgkin lymphoma is best regarded as a systemic disease because of the unique anatomy of the lymphoid system and because of the physiology of lymphoid cells, which tend to migrate whether they are normal or malignant. Childhood non-Hodgkin lymphoma generally manifests as bulky extramedullary (usually extranodal) disease with or without demonstrable dissemination.
Taken collectively, lymphomas are the most common childhood malignancies followed by acute leukemias. Burkitt lymphoma is significantly most common in sub-Saharan Africa, where it accounts for approximately one half of childhood cancers. Its incidence also appears to be higher in Latin America, in North Africa, and in the Middle East.[3]
Patients with SNCCLs may present with a mass in the jaw (i.e., endemic Burkitt's lymphoma classically seen in equatorial Africa), nasopharynx, or orbit. Abdominal mass (typically in the ileocecal area and arising from Peyer patches) may cause bowel obstruction due to direct compression, torsion, or intussusception.[1,2]
Rapidly growing or bulky tumors can cause severe metabolic derangement, and have potential for tumor lysis syndrome. Other immediate risks depend on the site, the extent of involvement and the histologic subtype of the disease. Individuals with lymphoblastic lymphoma often present with mediastinal involvement, which may be massive and life threatening.
Anaplastic large-cell lymphoma (T-cell neoplasm) often present with mediastinal lymphadenopathy, involvement of the skin and bone. Pulmonary parenchymal lesions occur more often in this type of non-Hodgkin's lymphoma than in other types. Bone marrow infiltration is unusual. Mediastinal tumors may cause symptomatic airway compromise, compression of the great vessel (superior vena cava syndrome), with plethora, swelling of the neck, face, and upper extremities, esophageal compression resulting in dysphagia. Pleural effusion may be large enough to cause symptoms.
With current treatments, non-Hodgkin lymphomas in most children are apparently curable through precise histologic diagnosis, thorough staging of the disease, and multiagent (and sometimes multimodal) treatment. The short-term morbidity of chemotherapy regimens is considerable, but the effects are usually manageable.[6,7]
CONCLUSION
The paucity and inadequacy of diagnostic facilities in our center contributed to the low index of suspicion of lymphoblastic lymphoma in this case. The present report therefore aimed at raising the local index of clinical suspicion by highlighting the reality of rarities, even with inadequate diagnostic facilities!
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
| Fig. 1 Chest radiograph showed no active focal lung lesion
| Fig. 2 The thoraco-lumber spine showed a vertebral planner at L1 and a wedged collapse of T11-T12 vertebrae


 PDF
PDF  Views
Views  Share
Share

