Multifocal Osseous Epithelioid Hemangioendothelioma Involving Extremities and Spine with Visceral Metastasis
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2018; 39(01): 103-105
DOI: DOI: 10.4103/ijmpo.ijmpo_31_16
Abstract
Epithelioid hemangioendothelioma (EH) is a rare locally aggressive intermediate grade malignant vasoformative tumor. Bone is a rarer primary site accounting for less than 1% of all malignant bone tumors. Multicentricity and/or multifocality are a relatively frequent occurrence, most commonly clustered in the bones of lower extremities. The axial skeleton is less commonly affected, and concomitant visceral involvement is rarer. We report a unique case of a 20-year-old male who presented with multiple lytic lesions in the skull vault, vertebral bones, bilateral proximal femur, and both radii and humerii with metastasis to the lungs and liver. A final diagnosis of EH was established on biopsy from the right iliac bone. He initially received multiagent chemotherapy and is currently on antiangiogenic therapy. On follow-up positron emission tomography?computerized tomography done 6 months later, marked reduction in fluoro-D-glucose avidity of the hepatic and most skeletal lesions was noted.
Keywords
Bone - epithelioid hemangioendothelioma - lower extremities - metastasis - spinePublication History
23 June 2021
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Epithelioid hemangioendothelioma (EH) is a rare locally aggressive intermediate grade malignant vasoformative tumor. Bone is a rarer primary site accounting for less than 1% of all malignant bone tumors. Multicentricity and/or multifocality are a relatively frequent occurrence, most commonly clustered in the bones of lower extremities. The axial skeleton is less commonly affected, and concomitant visceral involvement is rarer. We report a unique case of a 20-year-old male who presented with multiple lytic lesions in the skull vault, vertebral bones, bilateral proximal femur, and both radii and humerii with metastasis to the lungs and liver. A final diagnosis of EH was established on biopsy from the right iliac bone. He initially received multiagent chemotherapy and is currently on antiangiogenic therapy. On follow-up positron emission tomography?computerized tomography done 6 months later, marked reduction in fluoro-D-glucose avidity of the hepatic and most skeletal lesions was noted.
Keywords
Bone - epithelioid hemangioendothelioma - lower extremities - metastasis - spine
Introduction
Epithelioid hemangioendothelioma (EH) is a rare vasoformative tumor with a malignant potential intermediate between hemangioma and angiosarcoma. Bone as a primary site is exceedingly rare accounting for less than 1% of malignant bone tumors.[1] Less than 10% of the lesions occur in the spinal location.[2] Approximately one-third to one-half of osseous EH are multicentric within a bone or multifocal within multiple bones throughout the skeleton or clustered in an anatomical region, most commonly the lower extremity.[1],[3] We report a unique case of a 20-year-old male with multifocal EH presenting as multiple lytic lesions in the skull vault, vertebral bones, bilateral proximal femur, and both radii and humerii with metastasis to the lungs and liver.
Case Report
A 20-year-old male patient developed pain in the neck with mild restriction of neck movement initially felt during exercise in August 2014.
He underwent imaging of the skull, spine, chest, and pelvis which revealed multiple large mildly expansile sharply marginated osteolytic lesions with variable peripheral sclerosis involving the calvarial bones, C1, C7, L5 vertebrae, posterior part of 12th rib, atlanto-occipital, atlanto-axial, ilio-sarcral joints, right iliac bone, iliopubic rami, ischiopubic rami, bilateral proximal femur, and both radii and humerii [Figure 1]. Rest of the spine showed altered signal intensity in D4, D5, D10, D11, D1, and L4 vertebrae. In addition, numerous interstitial nodules were visualized in both lung fields. Radiologists offered Langerhans cell histiocytosis (LCH) as the most probable underlying disease. However, multiple myeloma, though less likely, was also considered in the clinical differentials. Subsequently, 2-deoxy-2-(18 F) fluoro-D-glucose positron emission tomography (FDG-PET) scan also highlighted multiple FDG avid pulmonary and hepatic metastatic lesions.
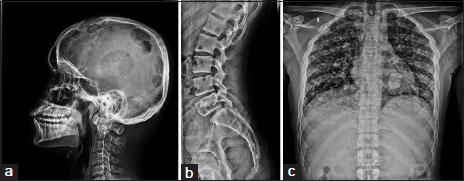
|?Figure.1X-ray shows (a) multiple lytic lesions in skull, (b) lumbar vertebrae and (c) bilateral lung nodules
His complete blood counts, urine routine examination, kidney function tests, serum uric acid, serum calcium, and tumor markers were all within normal limits. Urine for Bence Jones protein was negative. The serum free light chain level and ratio were also within normal limits.
A bone biopsy from right iliac bone was submitted to the Department of pathology which showed a tumor comprising of plump polygonal to spindle-shaped cells arranged predominantly in solid nests [Figure 2]. These cells had a moderate amount of eosinophilic cytoplasm, vesicular nuclei exhibiting mild to moderate pleomorphism and small nucleoli. Mitotic figures were sparse. Few of the cells showed the presence of intracytoplasmic lumina mimicking a signet ring appearance. However, close inspection revealed erythrocytes present within some of the lumina. In addition, a few slit-like ill-defined vasoformative structures were also appreciated. A panel of immunohistochemical stains was performed. CD31 and CD 34 immunopositivity in the tumor cells confirmed the endothelial nature of the cells. They were immunonegative for CD68 (histiocytic marker), S100, CD1a, Langerin (marker for Langerhans cells), and CD138 (plasma cell marker) thereby ruling out LCH and myeloma. A final pathological diagnosis of EH was rendered.
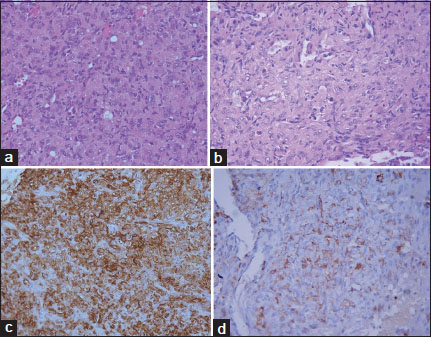
|?Figure.2(a) Polygonal to spindle shaped tumor cells are arranged in solid sheet; (H and E ?200), (b) the tumor cells show moderate nuclear pleomorphism, eosinophilic cytoplasm, small nucleoli and intracytoplasmic lumina with presence of red blood cells in the lumina; (H and E; ?400), the tumor cells are immunopositive for (c) CD34; ?200 and (d) CD31; ?400
He was initially administered a chemotherapeutic cocktail of vinblastine and methotrexate along with parenteral zoledronic acid and oral celecoxib. Subsequently, he has been treated with a maintenance antiangiogenic therapy with thalidomide in addition to zoledronic acid, celecoxib, and calcium supplementation. A follow-up PET-computerized tomography done 6 months later showed a reduction in FDG avidity of the hepatic and most skeletal lesions. The pulmonary lesions remain largely unchanged.
Discussion
Weiss and Enzinger first described EH in soft tissue location and also recognized its endothelial nature as well as intermediate malignant potential in a case series of 46 patients published in 1982.[4],[5] Subsequently, EH has been reported in multiple osseous and virtually all visceral sites, particularly liver and lung.[4]
EH of bone is extremely rare lesion that can affect any age group, but most commonly occurs during the second and third decade of life with a slight male predilection.[1],[6] Patients mostly present with nonspecific symptoms of pain, swelling, and less commonly pathological fracture. Concomitant visceral involvement is rarely observed in few patients.[6]
The distinction between multifocal and metastatic disease, especially with synchronous foci in anatomically distant sites such as femur and spine, has been debated by many authors considering this tumor has definite hematogenous metastatic potential.[1] Our patient presented with an extensive disease afflicting not only both the upper and lower extremities but also the spine and calvarium with simultaneous visceral (liver and lung) involvement.
The imaging features are largely nonspecific. The tumors are mostly purely lytic, poorly marginated with varying degrees of peripheral sclerosis prompting a host of radiological differential diagnosis, namely LCH, myeloma, metastasis, lymphoma, angiosarcoma, and even osteomyelitis.[6]
The diagnosis can be equally challenging on a core biopsy. The vasoformative nature of the malignancy may not be readily apparent on initial inspection. A myxohyaline character of the stroma often prompts the first suspicion. A close scrutiny usually reveals tumor cells with intracytoplasmic lumina often housing red blood cells indicating its endothelial nature which is confirmed by positive immunostaining with antibodies to CD31, CD34, and factor VIII.[1],[2],[3]
Much like its variable presentation, EH also has a widely variable clinical course. The disease may recur locally in approximately 13% of cases, whereas up to 31% of patients may develop metastasis.[1],[2] Surgical resection is most commonly employed for surgically amenable lesion(s) with adjuvant radiation often given to decrease the risk of local recurrence. However in patients with the multifocal/metastatic disease or surgically inaccessible site, the treatment protocol is even more poorly defined. A multimodal approach with radiation therapy is frequently adopted. Although the role of chemotherapy is not yet clear, it may be concurrently offered, especially to patients with extensive multifocal or metastatic disease.[1],[3],[6]
Our patient was administered chemotherapy and has a stable disease on 6-month follow up with in fact reduction in FDG avidity in the hepatic and most skeletal lesions.
Conclusion
EH of the bone is a rare tumor with a widely variable presentation, prognosis and poses considerable diagnostic and therapeutic challenge. It lacks any specific imaging findings and histology can often be quite deceptive, especially to the unwary. A high index of suspicion on light microscopy coupled with judicious use of immunohistochemical antibodies remains the gold standard to clinch the diagnosis.
Conflict of Interest
There are no conflicts of interest.
References
- Angelini A, Mavrogenis AF, Gambarotti M, Merlino B, Picci P, Ruggieri P.?Epithelioid hemangioendothelioma of bone. J Surg Oncol 2014; 109: 791-7
- Weiss SW, Goldblum J, Enzinger FM.?Enzinger and Weiss' Soft Tissue Tumors. Philadelphia, PA: Mosby 2001; 4: 891-914
- Liu Q, Miao J, Lian K, Huang L, Ding Z.?Multicentric epithelioid hemangioendothelioma involving the same lower extremity: A case report and review of literature. Int J Med Sci 2011; 8: 558-63
- Gherman CD, Fodor D. Epithelioid hemangioendothelioma of the forearm with radius involvement?Case report. Diagn Pathol 2011; 6: 120
- Weiss SW, Enzinger FM.?Epithelioid hemangioendothelioma: A vascular tumor often mistaken for a carcinoma. Cancer 1982; 50: 970-81
- Larochelle O, P?rigny M, Lagac? R, Dion N, Gigu?re C.?Best cases from the AFIP: Epithelioid hemangioendothelioma of bone. Radiographics 2006; 26: 265-70
Address for correspondence
Publication History
Article published online:
23 June 2021
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
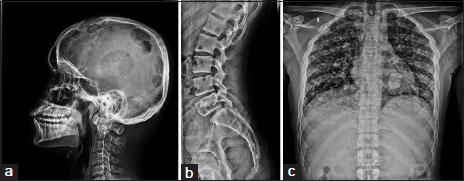
|?Figure.1X-ray shows (a) multiple lytic lesions in skull, (b) lumbar vertebrae and (c) bilateral lung nodules
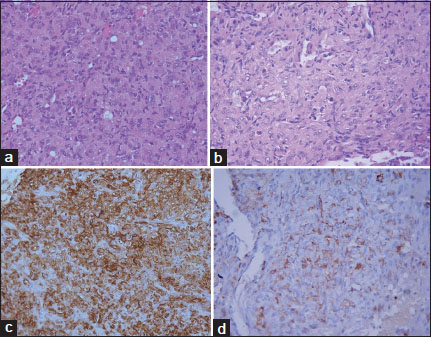
|?Figure.2(a) Polygonal to spindle shaped tumor cells are arranged in solid sheet; (H and E ?200), (b) the tumor cells show moderate nuclear pleomorphism, eosinophilic cytoplasm, small nucleoli and intracytoplasmic lumina with presence of red blood cells in the lumina; (H and E; ?400), the tumor cells are immunopositive for (c) CD34; ?200 and (d) CD31; ?400
References
- Angelini A, Mavrogenis AF, Gambarotti M, Merlino B, Picci P, Ruggieri P.?Epithelioid hemangioendothelioma of bone. J Surg Oncol 2014; 109: 791-7
- Weiss SW, Goldblum J, Enzinger FM.?Enzinger and Weiss' Soft Tissue Tumors. Philadelphia, PA: Mosby 2001; 4: 891-914
- Liu Q, Miao J, Lian K, Huang L, Ding Z.?Multicentric epithelioid hemangioendothelioma involving the same lower extremity: A case report and review of literature. Int J Med Sci 2011; 8: 558-63
- Gherman CD, Fodor D. Epithelioid hemangioendothelioma of the forearm with radius involvement?Case report. Diagn Pathol 2011; 6: 120
- Weiss SW, Enzinger FM.?Epithelioid hemangioendothelioma: A vascular tumor often mistaken for a carcinoma. Cancer 1982; 50: 970-81
- Larochelle O, P?rigny M, Lagac? R, Dion N, Gigu?re C.?Best cases from the AFIP: Epithelioid hemangioendothelioma of bone. Radiographics 2006; 26: 265-70


 PDF
PDF  Views
Views  Share
Share

