Molecular Profiling of High-Grade B-Cell Non-Hodgkin Lymphomas and Its Clinicopathologic Correlation in an Indian Tertiary Cancer Care Center
CC BY 4.0 · Indian J Med Paediatr Oncol 2024; 45(06): 515-522
DOI: DOI: 10.1055/s-0044-1785220
Abstract
Introduction Double-expressor and double-hit lymphomas (DHL) are known to be more aggressive and have poor outcomes with standard chemotherapy regimens.
Objectives To assess the incidence of DHL and triple-hit lymphomas (THL) and correlate them with clinicopathologic parameters.
Materials and Methods Patients who were diagnosed with high-grade lymphomas from April 2021 to September 2022 were prospectively followed up, and details comprising clinical and pathological parameters, including the immunohistochemistry expression status and gene rearrangements of MYC, BCL2, and BCL6, were recorded.
Results The incidence of DHL and THL in our study was 16.43%. The separate incidence of the DHL-BCL2, DHL-BCL6, and THL groups was 16.43, 13.69, and 2.73%, respectively. The germinal center B cell subtype of histology was predominantly seen in DHLs. MYC, BCL2, and BCL6 expressions do not correlate well with translocations of these genes.
Conclusion Double protein expression cannot be used for screening to decide which patients should undergo fluorescence in situ hybridization, as this would result in missing 4.5%-of DHLs.
Keywords
double-hit lymphoma - triple-hit lymphoma - double-expressor lymphoma - triple-expressor lymphoma - double protein expressionPatient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given their consent for her images and other clinical information to be reported in the journal. The patient understands that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Ethical Considerations
The study was submitted and cleared by the Institutional Ethical Committee-Biomedical Research, Apollo Hospitals, Chennai, EC Reg No. EC/NEW/INST/2020/527 NABH Certification No. EC-CT-2018-0045 on April 29, 2021, as per approval number ASH-DNB-042/04-21. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All patients included in the study were provided with a patient information leaflet and consented to be part of the study on the informed consent form.
Publication History
Article published online:
10 April 2024
© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Malignant lymphoma in Eastern India: A retrospective analysis of 455 cases according to World Health Organization classificationSantosh Kumar Mondal, Indian Journal of Medical and Paediatric Oncology, 2013
- Profile of non-Hodgkin lymphoma: An Indian perspectiveAjay Gogia, South Asian Journal of Cancer, 2018
- Histopathological pattern of lymphomas and clinical presentation and outcomes of diffuse large B cell lymphoma: A multicenter registry based study from IndiaRamesh B.V. Nimmagadda, Indian Journal of Medical and Paediatric Oncology, 2013
- Molecular Classification of Diffuse Large B-Cell LymphomaAnnie Kanchan Baa, Indian J Radiol Imaging, 2021
- Pattern of Non-Hodgkin Lymphoma in a Tertiary Care Center in Northeast India Using Morphology and ImmunohistochemistryJagannath Dev Sharma, Indian Journal of Medical and Paediatric Oncology, 2019
- Differences in the Clinicopathological Feature, Prognostic Features and Treatment Outcomes between Molecular Subtypes Among Indian Cohort with Diffuse Large B-C...Vaid, Blood, 2019
- Clinical Significance of CD21 Co-Expressed with LFA-1 in Non-Hodgkin’s B-Cell Lymphoma.Kazushi Tanimoto, Blood
- Transcriptome Classification of B-Cell Non-Hodgkins Lymphoma.Aggarwal, Blood
- Non-Hodgkin's Lymphoma: Molecular Features of B Cell LymphomaElizabeth Macintyre, Hematology ASH Education Program, 2000
- LymphGen Classification of Diffuse Large B-Cell Lymphoma in a Cohort of Adolescent and Young Adult (AYA) PatientsAngelo Cabal, Blood, 2022
Abstract
Introduction Double-expressor and double-hit lymphomas (DHL) are known to be more aggressive and have poor outcomes with standard chemotherapy regimens.
Objectives To assess the incidence of DHL and triple-hit lymphomas (THL) and correlate them with clinicopathologic parameters.
Materials and Methods Patients who were diagnosed with high-grade lymphomas from April 2021 to September 2022 were prospectively followed up, and details comprising clinical and pathological parameters, including the immunohistochemistry expression status and gene rearrangements of MYC, BCL2, and BCL6, were recorded.
Results The incidence of DHL and THL in our study was 16.43%. The separate incidence of the DHL-BCL2, DHL-BCL6, and THL groups was 16.43, 13.69, and 2.73%, respectively. The germinal center B cell subtype of histology was predominantly seen in DHLs. MYC, BCL2, and BCL6 expressions do not correlate well with translocations of these genes.
Conclusion Double protein expression cannot be used for screening to decide which patients should undergo fluorescence in situ hybridization, as this would result in missing 4.5%-of DHLs.
Keywords
double-hit lymphoma - triple-hit lymphoma - double-expressor lymphoma - triple-expressor lymphoma - double protein expressionIntroduction
Non-Hodgkin lymphomas (NHLs) are a heterogeneous group of malignant lymphoproliferative conditions of B, T, and NK cells with differing patterns of behaviors and responses to treatment. According to GLOBOCAN (Global Cancer Observatory) data, the incidence of NHL globally was 5 per 100,000 population (2.8%-of all new cancer cases), with a mortality rate of 2.5 per 100,000.[1] In India, the incidence has been reported to be 2.9 per 100,000 in males and 1.5 per 100,000 in females.[2]
There have been changes in the nomenclature of NHLs in the recent World Health Organization classification of hematolymphoid neoplasm 2017.[3] Based on the revised nomenclature, high-grade NHL includes (1) Burkitt's lymphomas, (2) diffuse large B cell lymphoma (DLBCL), and (3) high-grade B cell lymphoma (HGBL).
The rearrangements of MYC, BCL2, and BCL6 genes are diagnosed by fluorescence in situ hybridization (FISH) and their protein expression by immunohistochemistry (IHC). The incidence of double-expressor lymphomas (DELs) varies from 13 to 46%.[4] [5] The incidence of double-hit lymphomas (DHLs) varies from 1.6%- in Asian studies to 7.9%- in Western literature.[6] [7] [8] [9] [10] [11] [12]
DHL may most commonly have a blastoid morphology (around 50%) or may be seen in DLBCL or Burkitt's lymphoma. The cell of origin (COO) of DLBCL may be determined by the Hans algorithm[13] or by gene expression profiling such as Lymph2Cx.[14] Based on COO, DLBCLs are divided into germinal center B cell (GCB) type or non-GCB (activated B cell or ABC) type. DELs are more commonly seen in the ABC type, whereas DHL is more commonly seen in the GCB type. DHL with MYC and BCL2 is exclusively seen in GCB type and is seen in 1.7%- of ABC type DLBCL. Due to the above-mentioned reasons, the morphology, IHC, or COO cannot be used to screen patients as to who should undergo FISH for detection of DHL. This would result in the unacceptable missed diagnosis of a few DHLs in the screened-out group. One option would be to screen patients by performing FISH for MYC translocation alone, and then to further test FISH for BCL2 and BCL6 only for those who are MYC altered.
DEL and DHL are known to have a poor prognosis and poor responses to standard chemotherapy regimens. There is a lack of data in the Indian scenario regarding the molecular profiling of lymphomas. This study aimed to detail the molecular profiling of high-grade lymphomas and their clinicopathological correlation.
Materials and Methods
Study Design
This is an observational cohort study conducted at Apollo Cancer Centre, Chennai (Tamil Nadu, India) during the period from April 2021 to September 2022.
Sample Size
The previously reported percentage incidence of DHLs was 10%.[8] For 95%- confidence and an error of 5%, the calculated sample size was 73.
Primary and Secondary Outcomes
The primary outcome was to assess the incidence of DHLs by molecular profiling of high-grade B cell NHLs. The secondary outcome was a correlation of the DHL status with clinicopathological and molecular findings.
Inclusion and Exclusion Criteria
Patients diagnosed with aggressive B cell NHLs (Burkitt's lymphoma, DLBCL, and HGBL) with an age older than 18 years were included in the study. Those patients with an age younger than 18 years, and all lymphomas other than aggressive NHLs, such as indolent B NHLs (low-grade follicular lymphoma, low-grade mantle cell and marginal zone lymphomas), and T cell NHLs were excluded.
Methods
The study patients underwent FISH of MYC, BCL2, and BCL6 (aggressive lymphoma panel) on the formalin-fixed paraffin-embedded specimen, preferably obtained from an excision biopsy of the lymph node. Data including demographic details, clinical symptoms, laboratory values, Eastern Cooperative Oncology Group (ECOG) performance status (PS), number of nodal stations involved, extranodal disease, bulky disease, central nervous system (CNS) disease, clinical stage, prognostic scoring, histology (DLBCL/HGBL/Burkitt's lymphoma), and IHC results were recorded. The patients were considered into four groups: (1) DHL-BCL2 (DHL with rearrangement of MYC and BCL2), (2) DHL-BCL6 (DHL with rearrangement of MYC and BCL6), (3) triple-hit lymphoma (THL with rearrangement of MYC, BCL2, and BCL6), and (4) the standard group (“nonhit” lymphomas). The association between each variable and positivity for the aggressive lymphoma panel was analyzed. A correlation between IHC positivity (expressor lymphomas) and FISH positivity (hit lymphomas) was also performed.
Statistical Analysis
All categorical variables were expressed as percentages. Continuous variables, such as age, were expressed as their mean ± standard deviation if they were normally distributed. Nonnormally distributed continuous variables were represented by their median interquartile range. Comparison of categorical variables was done by either the chi-square test or Fisher's exact test. Data entry was done in Epidata Entry version 3.1. Data analysis was performed using SPSS version 26. All p-values < 0.05 were considered statistically significant.
Results
Results of the Total Cohort
Demographics
There were a total of 73 patients in this study. The mean age of the patients was 52.67 ± 15.62 years, ranging from 20 to 85 years.
Clinical Parameters
Fifty-five patients (75%) of them had an ECOG PS of 1. Only two of them were asymptomatic with an ECOG PS of 0. Fourteen (19.2%) of them had an ECOG PS of 2, and one each had an ECOG PS of 3 and 4. Eighteen (24.7%) of the patients had any one of the B symptoms. Ten (13.7%) of them had fever as one of the presenting complaints. Thirteen (17.8%) of them had a weight loss of more than 10%- of their body weight over the past 6 months. None of them had night sweats.
Clinical Parameters
Fifty-five patients (75%) of them had an ECOG PS of 1. Only two of them were asymptomatic with an ECOG PS of 0. Fourteen (19.2%) of them had an ECOG PS of 2, and one each had an ECOG PS of 3 and 4. Eighteen (24.7%) of the patients had any one of the B symptoms. Ten (13.7%) of them had fever as one of the presenting complaints. Thirteen (17.8%) of them had a weight loss of more than 10%- of their body weight over the past 6 months. None of them had night sweats.
Laboratory Parameters
The mean hemoglobin was 11.73 ± 2.28 g/dL. Thirty-seven of them had hemoglobin less than 12 g/dL. The mean total count was 10,596.58 ± 23,807 cells/mm3, ranging from 1,600 to 208,900 cells/mm3. The platelet count varied from 80,000 729,000 /mm3, with a mean of 273,300/mm3. The mean neutrophil percentage was 69.30 ± 15.11%, and the mean lymphocyte count was 18.42 ± 10.15%. The mean absolute neutrophil count was 5,702.26 ± 3,251.86. Only two patients had neutropenia at diagnosis, one with mild and another with moderate neutropenia.
The mean lactate dehydrogenase (LDH) value was 777.24 ± 2,608.24 units/L, ranging from 130 to 22,020 units/L. LDH was more than the upper limit of normal in 50 (72.2%) patients.
The mean ki67 value was 81.52 ± 15.87%. The ki67 was 80%- or higher in 50 patients. Only four patients had a ki67 of less than 50%.
There was no nodal involvement in four patients. The nodal involvement was limited to one to three nodal groups in 33 patients (45.1%). Seven or more nodal stations were involved in 15 patients.
Extranodal involvement was present in 59 (80%) patients; 26 of them had only involvement in a single extranodal site. Two, three, and ≥ four extranodal sites were involved in 16 (21.9%), 11 (15.1%), and 6 (8.3%) of them, respectively. Bone marrow involvement was seen in six (8.2%) patients. Bulky disease was present in four (5.5%) patients. CNS involvement was seen in five (6.8%) patients. Most of the patients had advanced disease, with 42 (57.5%) of them in stage IV and 11 (15.1%) of them in stage III. Fourteen (19.2%) and 6 (8.2%) of them were in stages II and I, respectively. The international prognostic index (IPI) was ≥ 3 in 39 (53.4%) patients and ≥ 4 in 18 (24.6%) patients. The CNS IPI score was ≥ 4 in 26 (35.6%) patients. The most common histology was the DLBCL–GCB type seen in 37 (50.7%) patients, followed by the DLBCL–non-GCB type in 23 (31.5%) patients. HGBL was seen in eight patients and in three Burkitt's lymphomas.
MYC, BCL2, and BCL6 Expression in the Total Cohort
MYC expression was seen in 30 out of 66 evaluable patients (45.5%). BCL2 was expressed in 39 of the 66 patients (59.1%). BCL6 protein expression was found in 46 of all 64 patients (79.1%) ([Fig. 1]).
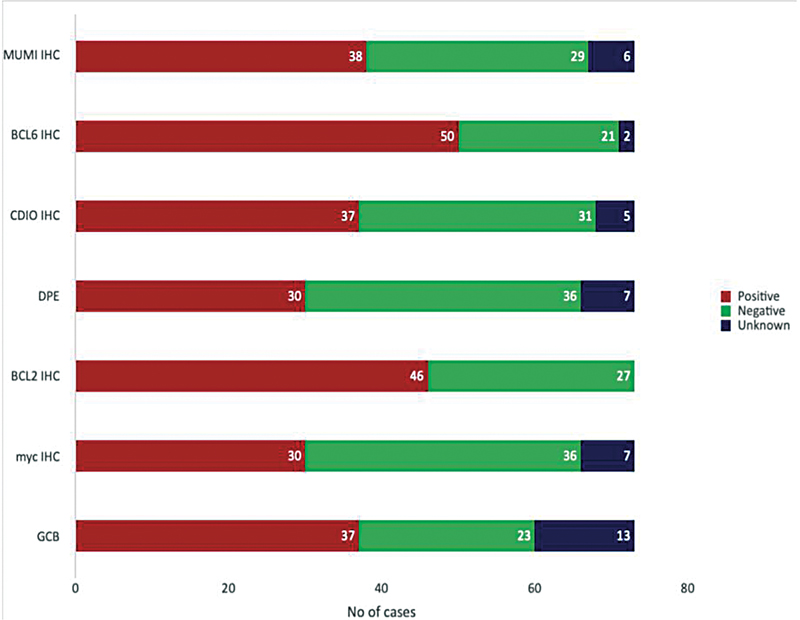
| Fig 1 Percentage positivity of selected immunohistochemistry (IHC) markers, double protein [removed]DPE), and germinal center B cell (GCB) histology in the total cohort including all the patients.|
MYC, BCL2, and BCL6 Gene Rearrangements in the Total Cohort
MYC translocation was seen in 18 out of 73 patients (24.7%). BCL2 translocation was found in 15 out of 58 patients (20.5%). BCL6 translocations were seen in 25 out of 73 patients (34.2%).
Out of the 18 MYC translocations, the partner was Immunoglobulin heavy locus (IgH) in 10 of the cases. Out of the 15 BCL2 translocations detected, the partner was IgH in 10 of the cases. In the remaining cases, the partner was unknown.
Results of Patients with Double-Expressor Lymphoma
Of the 73 patients, IHC for MYC data was available for 66 patients. They were divided into the triple-expressor lymphoma (TEL) group, the DEL-BCL2 group, the DEL-BCL6 group, and the nonexpressor lymphoma group.
MYC, BCL2, and BCL6 Expression in Expressor Lymphomas
MYC expression was positive in all DEL/TEL patients, as was expected, and none in the nonexpressor groups. BCL2 expression was seen in 17 out of 36 (47.2%) standard group patients and 22 of the 30 (73.3%) expressor lymphoma patients. Similarly, BCL6 expression was seen in 19 out of 35 standard group patients and in 27 of the 29 patients in the expressor lymphoma groups ([Table 1]).
Parameter | Total cohort for IHC [removed]n = 66) | Nonexpressor (n = 36) | DEL-BCL2 (n = 8) | DEL-BCL6 (n = 3) | TEL (n = 19) | Total cohort for gene rearrangements (n = 73) | Nonhit lymphomas (n = 61) | DHL-BCL2 (n = 8) | DHL-BCL6 (n = 2) | THL (n = 2) |
|---|---|---|---|---|---|---|---|---|---|---|
MYC IHC | 30 (45.5) | 0 (0) | 8 (100) | 3 (100) | 19 (100) | 30 (41.0) | 21 (34.4) | 6 (57) | 1 (50) | 2 (100) |
BCL2 IHC | 39 (59.1) | 17 (47.2) | 0 (0) | 3 (100) | 19 (100) | 46 (63) | 34 (55.7) | 8 (100) | 2 (100) | 2 (100) |
BCL6 IHC | 46 (71.9) | 19 (54.3) | 8 (100) | 0 (0) | 19 (100) | 50 (68.5) | 40 (65.6) | 6 (75) | 2 (100) | 2 (100) |
MYC gene rearrangement | 17 (25.5) | 3 (8.3) | 2 (25) | 2 (66.7) | 10 (52.6) | 18 (24.7) | 6 (9.8) | 8 (100) | 2 (100) | 2 (100) |
BCL2 gene rearrangement | 15 (22.7) | 7 (19.4) | 0 (0) | 1 (33.3) | 7 (36.8) | 15 (20.5) | 5 (8.2) | 8 (100) | 0 (0) | 2 (100) |
BCL6 gene rearrangement | 21 (31.8) | 12 (33.3) | 1 (12.5) | 1 (33.3) | 7 (36.8) | 25 (34.2) | 21 (34.4) | 0 (0) | 2 (100) | 2 (100) |
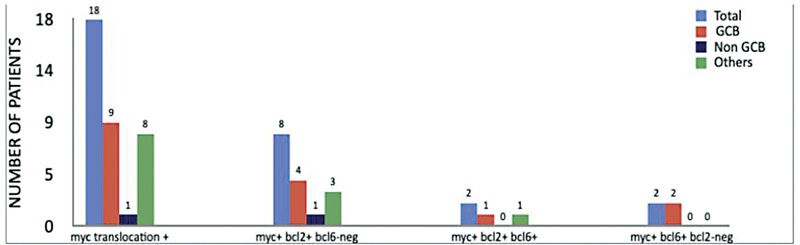
| Fig 2 Distribution of germinal center B cell (GCB) versus non-GCB histologies among patients with MYC translocation, double-hit lymphoma (DHL) with BCL2, DHL with BCL6, and triple-hit lymphoma, expressed in the number of patients.|
MYC, BCL2, and BCL6 Translocations in Hit Lymphomas
Eighteen patients tested positive for MYC by FISH. Six out of 61 patients in the standard hit group had MYC positivity. Of the remaining 12 cases, 2 were in THL, 8 were in DHL-BCL2, and 2 were in DHL-BCL6 groups. Fifteen patients were positive for BCL2 by FISH. Five out of 61 patients in the standard hit group had BCL2 positivity. Of the remaining 10 cases, 2 were in THL and 8 were in DHL-BCL2 groups. Twenty-five patients were positive for BCL6 by FISH. Twenty-one of the 61 patients in the standard hit group were positive, while of the remaining 4 patients, 2 were in the THL group and the other 2 in the DHL-BCL6 group.
Correlation of MYC, BCL2, and BCL6 Expression and Gene Abnormalities
MYC-IHC Positivity in Hit Lymphomas
All two of the patients with THL (100%) were positive for MYC expression. Six out of 8 (75%) in the DHL-BCL2 group, 1 of the 2 (50%) patients with DHL-BCL6, and 21 of the 61 (3.2%) patients in the nonhit lymphoma groups were found to have MYC IHC positive.
BCL2 IHC Positivity in Hit Lymphomas
All patients in THL (two patients), DHL-BCL2 (eight patients), and DHL-BCL6 (two patients) had BCL2-IHC positive, while this was 34 out of 61 (55%) in the standard group.
BCL6 IHC Positivity in Hit Lymphomas
Two out of 2 (100%) patients were each in the THL and DHL-BCL6 groups, while 6 of the 8 patients in the DHL-BCL2 group had BCL6-IHC positivity; 40 out of 61 patients (65%) have BCL6-IHC positivity ([Table 1]).
MYC Gene Rearrangements in Expressor Lymphomas
MYC gene rearrangements were seen in 2 of the 8 (25%) DEL with BCL2, 2 of the 3 (66.7%) DEL with BCL6, and 10 of the 19 (52.63%) TELs. Only 7 of the 36 (19.4%) nonhit lymphoma patients had MYC gene rearrangements.
BCL2 Gene Rearrangements in Expressor Lymphomas
One out of 3 (33%) and 7 out of 19 (36%) patients had BCL2 gene rearrangements in the TEL and DEL-BCL6 groups, respectively, while the DEL-BCL2 groups had 0 out of 8 patients (0%). Seven of the 36 (19.4%) patients in the nonexpressor group had BCL2 gene rearrangements.
BCL6 Gene Rearrangements in Expressor Lymphomas
one out of the 8 (12.5%), 1 out of 3 (33.3%), and 7 out of 19 (36.8%) patients in the DEL-BCL2, DEL-BCL6, and TEL groups had BCL6 gene rearrangements, whereas this was 12 out of 36 (33.33%) in the nonexpressor group ([Table 2]).
Gene abnormality | Total | |||
|---|---|---|---|---|
Hit lymphoma | Nonhit lymphoma | |||
IHC expression status | Expressor lymphomas | 9 | 21 | 30 |
Nonexpressor lymphomas | 3 | 33 | 36 | |
Total | 12 | 54 | 66 | |
Parameter | Value |
|---|---|
Sensitivity | 75.0 |
Specificity | 61.1 |
PPV | 30.0 |
NPV | 91.7 |
Accuracy | 63.6 |
References
- Sung H, Ferlay J, Siegel RL. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- Nair R, Arora N, Mallath MK. Epidemiology of non-Hodgkin's lymphoma in India. Oncology 2016; 91 (Suppl. 01) 18-25
- Swerdlow SH, Campo E, Harris NL. et al., eds. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised 4th ed. Vol. 1.. Lyon Cedex, France: International Agency for Research on Cancer (IARC); 2017
- Hu S, Xu-Monette ZY, Tzankov A. et al. MYC/BCL2 protein coexpression contributes to the inferior survival of activated B-cell subtype of diffuse large B-cell lymphoma and demonstrates high-risk gene expression signatures: a report from The International DLBCL Rituximab-CHOP Consortium Program. Blood 2013; 121 (20) 4021-4031 , quiz 4250
- Johnson NA, Slack GW, Savage KJ. et al. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol 2012; 30 (28) 3452-3459
- Scott DW, Wright GW, Williams PM. et al. Determining cell-of-origin subtypes of diffuse large B-cell lymphoma using gene expression in formalin-fixed paraffin-embedded tissue. Blood 2014; 123 (08) 1214-1217
- Landsburg DJ, Petrich AM, Abramson JS. et al. Impact of oncogene rearrangement patterns on outcomes in double-hit non-Hodgkin lymphoma. Cancer 2016; 122 (04) 559-564
- Sermer D, Bobillo S, Seshan V, Dogan A, Younes A. Clinical significance and outcomes in patients with diffuse large B-cell lymphoma (dlbcl) harboring extra copies [ec] and/or translocations [tl] of Myc, Bcl2, and Bcl6. Hematol Oncol 2019; 37 (S2): 349-350
- Ting CY, Chang KM, Kuan JW. et al. Clinical significance of BCL2, C-MYC, and BCL6 genetic abnormalities, Epstein-Barr virus infection, CD5 protein expression, germinal center B cell/non-germinal center B-cell subtypes, co-expression of MYC/BCL2 proteins and co-expression of MYC/BCL2/BCL6 proteins in diffuse large B-cell lymphoma: a clinical and pathological correlation study of 120 patients. Int J Med Sci 2019; 16 (04) 556-566
- Huang S, Nong L, Wang W. et al. Prognostic impact of diffuse large B-cell lymphoma with extra copies of MYC, BCL2 and/or BCL6: comparison with double/triple hit lymphoma and double expressor lymphoma. Diagn Pathol 2019; 14 (01) 81
- Zhang Y, Wang H, Ren C. et al. Correlation between C-MYC, BCL-2, and BCL-6 protein expression and gene translocation as biomarkers in diagnosis and prognosis of diffuse large B-cell lymphoma. Front Pharmacol 2019; 9: 1497
- Salam DSDA, Thit EE, Teoh SH, Tan SY, Peh SC, Cheah SC. C-MYC, BCL2 and BCL6 translocation in B-cell non-Hodgkin lymphoma cases. J Cancer 2020; 11 (01) 190-198
- Hans CP, Weisenburger DD, Greiner TC. et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 2004; 103 (01) 275-282
- Jais JP, Molina TJ, Ruminy P. et al. Reliable subtype classification of diffuse large B-cell lymphoma samples from GELA LNH2003 trials using the Lymph2Cx gene expression assay. Haematologica 2017; 102 (10) e404-e406
- Mehta A, Verma A, Gupta G, Tripathi R, Sharma A. Double hit and double expresser diffuse large B cell lymphoma subtypes: discrete subtypes and major predictors of overall survival. Indian J Hematol Blood Transfus 2020; 36 (04) 627-634
- Landsburg DJ, Nasta SD, Svoboda J, Morrissette JJD, Schuster SJ. ‘Double-Hit’ cytogenetic status may not be predicted by baseline clinicopathological characteristics and is highly associated with overall survival in B cell lymphoma patients. Br J Haematol 2014; 166 (03) 369-374
- Barraclough A, Alzahrani M, Schmidt Ettrup M. et al. Impact of immunohistochemistry-defined cell of origin and MYC rearrangements on outcomes in patients with PET-defined stage I/II diffuse large B-cell lymphoma treated with R-CHOP ± radiotherapy: an International Multi-Center Retrospective Study. Blood 2017; 130 (Suppl. 01) 415
- Kluk MJ, Ho C, Yu H. et al. MYC immunohistochemistry to identify MYC-driven B-cell lymphomas in clinical practice. Am J Clin Pathol 2016; 145 (02) 166-179
- Sakr H, Cook JR. Identification of “double hit” lymphomas using updated WHO criteria: insights from routine MYC immunohistochemistry in 272 consecutive cases of aggressive B-cell lymphomas. Appl Immunohistochem Mol Morphol 2019; 27 (06) 410-415
- Horn H, Ziepert M, Becher C. et al; German High-Grade Non-Hodgkin Lymphoma Study Group. MYC status in concert with BCL2 and BCL6 expression predicts outcome in diffuse large B-cell lymphoma. Blood 2013; 121 (12) 2253-2263
Address for correspondence
Nikhil Sebastian, MD Radiation OncologyDepartment of Medical Oncology, Apollo Cancer Centre320, Padma Complex, Anna Salai, Chennai 600035, Tamil NaduIndiaEmail: drnikseban@gmail.comEmail: drnikhiloncology@yahoo.comPublication History
Article published online:
10 April 2024© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, IndiaWe recommend- Malignant lymphoma in Eastern India: A retrospective analysis of 455 cases according to World Health Organization classificationSantosh Kumar Mondal, Indian Journal of Medical and Paediatric Oncology, 2013
- Profile of non-Hodgkin lymphoma: An Indian perspectiveAjay Gogia, South Asian Journal of Cancer, 2018
- Histopathological pattern of lymphomas and clinical presentation and outcomes of diffuse large B cell lymphoma: A multicenter registry based study from IndiaRamesh B.V. Nimmagadda, Indian Journal of Medical and Paediatric Oncology, 2013
- Molecular Classification of Diffuse Large B-Cell LymphomaAnnie Kanchan Baa, Indian J Radiol Imaging, 2021
- Pattern of Non-Hodgkin Lymphoma in a Tertiary Care Center in Northeast India Using Morphology and ImmunohistochemistryJagannath Dev Sharma, Indian Journal of Medical and Paediatric Oncology, 2019
- Simplified algorithm for genetic subtyping in diffuse large B-cell lymphomaRong Shen, Signal Transduction and Targeted Therapy, 2023
- Non-Hodgkin lymphoma in childhood and adolescence: frequency and distribution of immunomorphological types from a tertiary care center in South IndiaMarie Therese Manipadam, World Journal of Pediatrics
- Outcome of aggressive B-cell lymphoma with TP53 alterations administered with CAR T-cell cocktail alone or in combination with ASCTJia Wei, Signal Transduction and Targeted Therapy, 2022
- Single-cell landscape of primary central nervous system diffuse large B-cell lymphomaNianping Liu, Cell Discovery, 2023
- Radiomics-based quantitative contrast-enhanced CT analysis of abdominal lymphadenopathy to differentiate tuberculosis from lymphomaMeng-Ting Shen, Precision Clinical Medicine, 2024
- Malignant lymphoma in Eastern India: A retrospective analysis of 455 cases according to World Health Organization classification
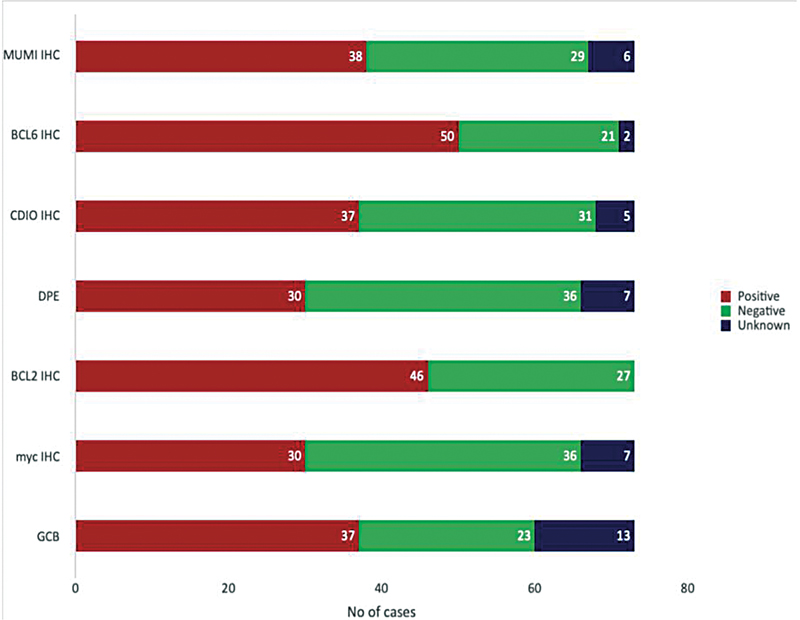
| Fig 1 Percentage positivity of selected immunohistochemistry (IHC) markers, double protein [removed]DPE), and germinal center B cell (GCB) histology in the total cohort including all the patients.|
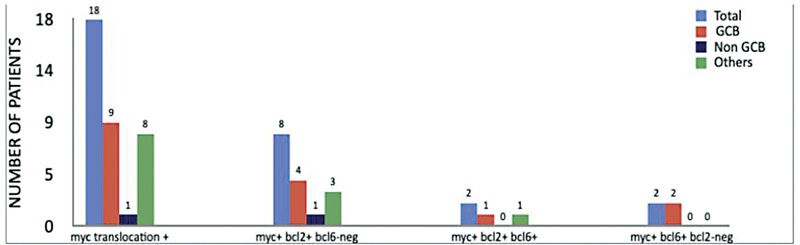
| Fig 2 Distribution of germinal center B cell (GCB) versus non-GCB histologies among patients with MYC translocation, double-hit lymphoma (DHL) with BCL2, DHL with BCL6, and triple-hit lymphoma, expressed in the number of patients.|
References
- Sung H, Ferlay J, Siegel RL. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- Nair R, Arora N, Mallath MK. Epidemiology of non-Hodgkin's lymphoma in India. Oncology 2016; 91 (Suppl. 01) 18-25
- Swerdlow SH, Campo E, Harris NL. et al., eds. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised 4th ed. Vol. 1.. Lyon Cedex, France: International Agency for Research on Cancer (IARC); 2017
- Hu S, Xu-Monette ZY, Tzankov A. et al. MYC/BCL2 protein coexpression contributes to the inferior survival of activated B-cell subtype of diffuse large B-cell lymphoma and demonstrates high-risk gene expression signatures: a report from The International DLBCL Rituximab-CHOP Consortium Program. Blood 2013; 121 (20) 4021-4031 , quiz 4250
- Johnson NA, Slack GW, Savage KJ. et al. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol 2012; 30 (28) 3452-3459
- Scott DW, Wright GW, Williams PM. et al. Determining cell-of-origin subtypes of diffuse large B-cell lymphoma using gene expression in formalin-fixed paraffin-embedded tissue. Blood 2014; 123 (08) 1214-1217
- Landsburg DJ, Petrich AM, Abramson JS. et al. Impact of oncogene rearrangement patterns on outcomes in double-hit non-Hodgkin lymphoma. Cancer 2016; 122 (04) 559-564
- Sermer D, Bobillo S, Seshan V, Dogan A, Younes A. Clinical significance and outcomes in patients with diffuse large B-cell lymphoma (dlbcl) harboring extra copies [ec] and/or translocations [tl] of Myc, Bcl2, and Bcl6. Hematol Oncol 2019; 37 (S2): 349-350
- Ting CY, Chang KM, Kuan JW. et al. Clinical significance of BCL2, C-MYC, and BCL6 genetic abnormalities, Epstein-Barr virus infection, CD5 protein expression, germinal center B cell/non-germinal center B-cell subtypes, co-expression of MYC/BCL2 proteins and co-expression of MYC/BCL2/BCL6 proteins in diffuse large B-cell lymphoma: a clinical and pathological correlation study of 120 patients. Int J Med Sci 2019; 16 (04) 556-566
- Huang S, Nong L, Wang W. et al. Prognostic impact of diffuse large B-cell lymphoma with extra copies of MYC, BCL2 and/or BCL6: comparison with double/triple hit lymphoma and double expressor lymphoma. Diagn Pathol 2019; 14 (01) 81
- Zhang Y, Wang H, Ren C. et al. Correlation between C-MYC, BCL-2, and BCL-6 protein expression and gene translocation as biomarkers in diagnosis and prognosis of diffuse large B-cell lymphoma. Front Pharmacol 2019; 9: 1497
- Salam DSDA, Thit EE, Teoh SH, Tan SY, Peh SC, Cheah SC. C-MYC, BCL2 and BCL6 translocation in B-cell non-Hodgkin lymphoma cases. J Cancer 2020; 11 (01) 190-198
- Hans CP, Weisenburger DD, Greiner TC. et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 2004; 103 (01) 275-282
- Jais JP, Molina TJ, Ruminy P. et al. Reliable subtype classification of diffuse large B-cell lymphoma samples from GELA LNH2003 trials using the Lymph2Cx gene expression assay. Haematologica 2017; 102 (10) e404-e406
- Mehta A, Verma A, Gupta G, Tripathi R, Sharma A. Double hit and double expresser diffuse large B cell lymphoma subtypes: discrete subtypes and major predictors of overall survival. Indian J Hematol Blood Transfus 2020; 36 (04) 627-634
- Landsburg DJ, Nasta SD, Svoboda J, Morrissette JJD, Schuster SJ. ‘Double-Hit’ cytogenetic status may not be predicted by baseline clinicopathological characteristics and is highly associated with overall survival in B cell lymphoma patients. Br J Haematol 2014; 166 (03) 369-374
- Barraclough A, Alzahrani M, Schmidt Ettrup M. et al. Impact of immunohistochemistry-defined cell of origin and MYC rearrangements on outcomes in patients with PET-defined stage I/II diffuse large B-cell lymphoma treated with R-CHOP ± radiotherapy: an International Multi-Center Retrospective Study. Blood 2017; 130 (Suppl. 01) 415
- Kluk MJ, Ho C, Yu H. et al. MYC immunohistochemistry to identify MYC-driven B-cell lymphomas in clinical practice. Am J Clin Pathol 2016; 145 (02) 166-179
- Sakr H, Cook JR. Identification of “double hit” lymphomas using updated WHO criteria: insights from routine MYC immunohistochemistry in 272 consecutive cases of aggressive B-cell lymphomas. Appl Immunohistochem Mol Morphol 2019; 27 (06) 410-415
- Horn H, Ziepert M, Becher C. et al; German High-Grade Non-Hodgkin Lymphoma Study Group. MYC status in concert with BCL2 and BCL6 expression predicts outcome in diffuse large B-cell lymphoma. Blood 2013; 121 (12) 2253-2263


 PDF
PDF  Views
Views  Share
Share

