Microcystic Pancreatic Ductal Adenocarcinoma: Myth or Reality
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(05): 731-732
DOI: DOI: 10.4103/ijmpo.ijmpo_312_20
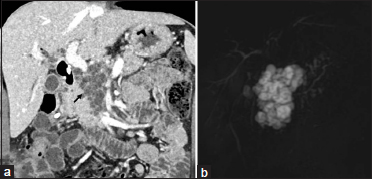
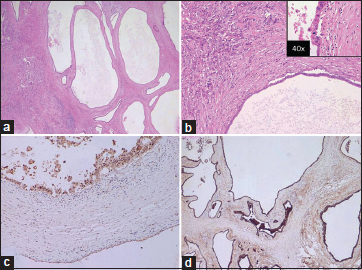
| Figure 1: (a) Contrast-enhanced computed tomography showing microcystic mass (arrow) in the pancreatic head. (b) Magnetic resonance cholangiopancreatography confirming a honeycomb cystic lesion in the head of the pancreas having communication with the main pancreatic duct with mild dilatation of the side-duct branches
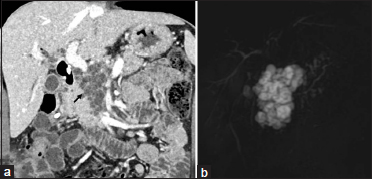
| Figure 2: (a) Low-power microphotograph showing cyst of variable size with epithelial lining, separated by paucicellular desmoplastic stroma (H and E, ×20). (b) Further magnification shows that the cyst is lined by cuboidal epithelial cells. The small irregular angulated glands are also noted (H and E ×100). Inset high-power image (×40) shows moderate nuclear atypia of lining epithelial cells and occasional atypical mitotic figures. (c and d) The lining epithelial cells of cysts show nuclear expression of p53 (×100) and membranous staining for carcinoembryonic antigen (×40)
PDAC typically presents as an irregular solid tumor with a scirrhous character resulting from a prominent desmoplastic reaction. The incidence of PDAC with cystic changes ranges from < 1% to 8%. PDACs with cystic change are uncommon and may occur by means of the four following mechanisms – (i) obstruction of the pancreatic duct by the tumor resulting in the formation of retention cysts localized outside the tumor periphery, (ii) coexisting acute pancreatitis resulting in pseudocyst formation localized outside the tumor, (iii) microcystic appearance caused by marked ectasia of the invasive gland and referred to as the “large-duct type,” and (iv) necrosis within the tumor. The large-duct type ectasia within the tumor was seen in the present case.
Publication History
Received: 28 June 2020
Accepted: 19 August 2020
Article published online:
17 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
We present the case of a 48-year-old male with pain in the upper abdomen and jaundice for 2 months. Minimally deranged liver function tests were seen in the form of mild elevation of total serum bilirubin – 1.16 mg/dL (N: 0.3–1.2 mg/dL) and raised alkaline phosphatase levels – 307 IU/L (N: 20–140 IU/L) with normal serum glutamic pyruvic transaminase/serum glutamic-oxaloacetic transaminase 35/20 IU/L. He was evaluated with contrast-enhanced computed tomography (CECT) and magnetic resonance cholangiopancreatography (MRCP). CECT revealed multicystic mass in the head of the pancreas [Figure 1]a]. In view of the raised bilirubin/cholangitis, endoscopic retrograde cholangiopancreatography with stenting was done. MRCP confirmed the presence of a honeycomb cystic lesion in the head of the pancreas having communication with the main pancreatic duct with mild dilatation of the side-duct branches [Figure 1]b]. A provisional diagnosis of branch-duct intraductal papillary mucinous neoplasm (IPMN) was made considering the morphology of the lesion. After taking due consent and fitness, he underwent open classic pancreatoduodenectomy. Postoperative histopathological examination revealed a highly infiltrative tumor composed of cysts of variable sizes separated by paucicellular desmoplastic stroma. The epithelial cells lining these cysts were cuboidal to low columnar and showed moderate nuclear pleomorphism and atypia. Frequent mitotic figures, including atypical ones, were seen (10–12/10 high-power field). At places, the nuclear stratification of the lining epithelial cells was noted. The lining epithelial cells of cysts showed positive staining for p53 and membranous staining for carcinoembryonic antigen, making the diagnosis of microcystic variant of pancreatic adenocarcinoma [Figure 2]a],[Figure 2]b],[Figure 2]c],[Figure 2]d] over IPMN. Pancreatic ductal adenocarcinoma (PDAC) with large-duct type cysts is one of the morphologic variations of PDACs, which is characterized by more dilated malignant ducts forming a microcystic feature. The size of cysts is small, usually 0.5–0.7 cm in diameter, occasionally exceeding 1 cm and can mimic IPMN or microcystic serous cystadenoma on imaging.
| Figure 1: (a) Contrast-enhanced computed tomography showing microcystic mass (arrow) in the pancreatic head. (b) Magnetic resonance cholangiopancreatography confirming a honeycomb cystic lesion in the head of the pancreas having communication with the main pancreatic duct with mild dilatation of the side-duct branches
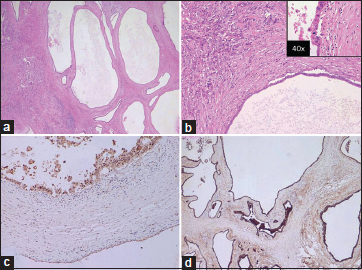
| Figure 2: (a) Low-power microphotograph showing cyst of variable size with epithelial lining, separated by paucicellular desmoplastic stroma (H and E, ×20). (b) Further magnification shows that the cyst is lined by cuboidal epithelial cells. The small irregular angulated glands are also noted (H and E ×100). Inset high-power image (×40) shows moderate nuclear atypia of lining epithelial cells and occasional atypical mitotic figures. (c and d) The lining epithelial cells of cysts show nuclear expression of p53 (×100) and membranous staining for carcinoembryonic antigen (×40)
PDAC typically presents as an irregular solid tumor with a scirrhous character resulting from a prominent desmoplastic reaction. The incidence of PDAC with cystic changes ranges from < 1% to 8%. PDACs with cystic change are uncommon and may occur by means of the four following mechanisms – (i) obstruction of the pancreatic duct by the tumor resulting in the formation of retention cysts localized outside the tumor periphery, (ii) coexisting acute pancreatitis resulting in pseudocyst formation localized outside the tumor, (iii) microcystic appearance caused by marked ectasia of the invasive gland and referred to as the “large-duct type,” and (iv) necrosis within the tumor. The large-duct type ectasia within the tumor was seen in the present case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
Address for correspondence
Publication History
Received: 28 June 2020
Accepted: 19 August 2020
Article published online:
17 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
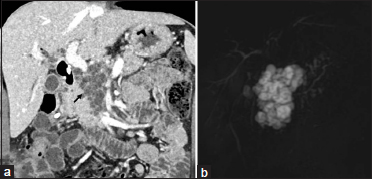
| Figure 1: (a) Contrast-enhanced computed tomography showing microcystic mass (arrow) in the pancreatic head. (b) Magnetic resonance cholangiopancreatography confirming a honeycomb cystic lesion in the head of the pancreas having communication with the main pancreatic duct with mild dilatation of the side-duct branches
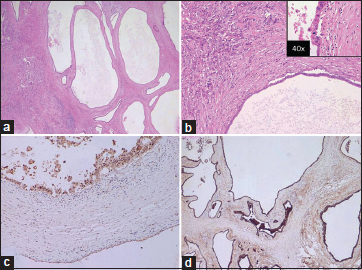
| Figure 2: (a) Low-power microphotograph showing cyst of variable size with epithelial lining, separated by paucicellular desmoplastic stroma (H and E, ×20). (b) Further magnification shows that the cyst is lined by cuboidal epithelial cells. The small irregular angulated glands are also noted (H and E ×100). Inset high-power image (×40) shows moderate nuclear atypia of lining epithelial cells and occasional atypical mitotic figures. (c and d) The lining epithelial cells of cysts show nuclear expression of p53 (×100) and membranous staining for carcinoembryonic antigen (×40)


 PDF
PDF  Views
Views  Share
Share

