Metastatic Nasopharyngeal Carcinoma: Outcome from Cancer Institute, Chennai
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(02): 198-201
DOI: DOI: 10.4103/ijmpo.ijmpo_160_19
Abstract
Background: Optimal management of metastatic nasopharyngeal carcinoma (NPC) at presentation is debatable. The aim of this study was to investigate the treatment outcome of patients with metastatic NPC treated with concurrent chemoradiation or with radiation alone and to analyze the factors that correlate with the outcome. Methods: This was a retrospective study of patients with metastatic NPC treated in Cancer Institute, Chennai, from 1996 to 2015 with either chemoradiation or only radiation. Factors including age, sex, stage, treatment type, and type of metastasis were correlated with the outcome. Statistical analysis was done using SPSS version 20, and survival was estimated by Kaplan–Meier’s curve. Results: A total of 515 patients with NPC were treated during this period, and among them, 74 patients (14%) had metastasis at the time of presentation. The median follow-up was 14 months; the median progression-free survival and overall survival (OS) were 11 months and 19 months, respectively. About 72% (n = 53) were treated with chemoradiation and the rest 28% (n = 21) were treated with radiation alone. The 3-year OS was better in patients who received chemoradiation (39%) as compared to those who received only radiation (23.8%). Patients with the bone-only site of metastasis had better survival. Among them patients with oligometastatic bone disease (1–3 sites) had a better 3-year OS (51%) as compared to multiple bone metastasis (>3) 15.8%. Conclusion: Chemoradiation can be an option to treat metastatic NPC. Patients with oligometastatic bone disease had better survival.
Publication History
Received: 31 July 2019
Accepted: 19 January 2020
Article published online:
23 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Background: Optimal management of metastatic nasopharyngeal carcinoma (NPC) at presentation is debatable. The aim of this study was to investigate the treatment outcome of patients with metastatic NPC treated with concurrent chemoradiation or with radiation alone and to analyze the factors that correlate with the outcome. Methods: This was a retrospective study of patients with metastatic NPC treated in Cancer Institute, Chennai, from 1996 to 2015 with either chemoradiation or only radiation. Factors including age, sex, stage, treatment type, and type of metastasis were correlated with the outcome. Statistical analysis was done using SPSS version 20, and survival was estimated by Kaplan–Meier’s curve. Results: A total of 515 patients with NPC were treated during this period, and among them, 74 patients (14%) had metastasis at the time of presentation. The median follow-up was 14 months; the median progression-free survival and overall survival (OS) were 11 months and 19 months, respectively. About 72% (n = 53) were treated with chemoradiation and the rest 28% (n = 21) were treated with radiation alone. The 3-year OS was better in patients who received chemoradiation (39%) as compared to those who received only radiation (23.8%). Patients with the bone-only site of metastasis had better survival. Among them patients with oligometastatic bone disease (1–3 sites) had a better 3-year OS (51%) as compared to multiple bone metastasis (>3) 15.8%. Conclusion: Chemoradiation can be an option to treat metastatic NPC. Patients with oligometastatic bone disease had better survival.
Keywords
Chemoradiation - metastatic nasopharyngeal cancer - survivalIntroduction
Nasopharyngeal carcinoma (NPC) is a rare malignancy with the highest incidence in patients from northeast India.[1] The majority of patients in India present with locally advanced stage or with distant metastasis.[2] [3] NPC is a chemotherapy and radiosensitive disease with distinct demographic, clinical, staging, and treatment options as compared to nonnasopharyngeal head-and-neck cancer.[4] In view of the paucity of randomized controlled trials in metastatic NPC, the optimal treatment is unknown. The usual practice is first-line platinum-based therapy and second-line gemcitabine- or taxane-based chemotherapy.[5] There is ongoing research with Epstein–Barr virus (EBV) such as vaccination or administration of cytotoxic T cells targeting EBV[6] and immunotherapy.[7] There is a lack of long-term outcomes of metastatic NPC from India. This study was done to compare the outcomes of patients with NPC treated with chemoradiation or radiation alone and to assess factors that correlated with the outcome.
Methods
This was a retrospective study of patients with metastatic NPC treated in Cancer Institute, Chennai, from 1996 to 2015. The diagnosis was established by biopsy of the nasopharyngeal mass. The staging investigations were contrast-enhanced computerized tomography of head and neck, chest X-ray, ultrasound of abdomen/pelvis, and bone scan. Patients were treated with palliative intent either with chemoradiation or only radiation. The chemotherapy regimen concurrent with radiation was either cisplatin and 5-fluorouracil or only cisplatin. Patients were reassessed after completion of chemoradiation or only radiation. Zoledronic acid 4 mg intravenously every month for 2 years was administered for patients with bone metastasis. After completion of treatment, patients were evaluated monthly for the first 6 months, 2 monthly until 2nd year, 3 monthly in the 3rd year, and 6 monthly thereafter. During the first follow-up, patients underwent clinical examination, nasopharyngoscopy, and biopsy, if any residual disease. Further investigations during the follow-up were nasopharyngoscopy, chest X-ray, ultrasound abdomen/pelvis every year, and bone scan, if symptomatic.
Progression-free survival (PFS) was calculated from the date of diagnosis to date of progression or date of the last follow-up. Overall survival (OS) was calculated from the date of diagnosis to date of death or date of the last follow-up. Survival was estimated by the Kaplan–Meier method. The Cox regression model was used to assess prognostic factors. P < 0>
Results
A total of 74 patients were included in this analysis, with a median follow-up of 14 months. The median age was 42 years (range: 9–77 years). Fifty-five patients (74%) were male and 19 (26%) were female. The most common symptom at presentation was a lump in the neck (78%) followed by a nasal block (18%). The histology was the World Health Organization (WHO) Type 2 in 93% and WHO Type 1 or 3 in 7%. T Stage was T1–T2 (57%) and T3–T4 (43%). N stage was N 0–1 (24%) and N 2–3 (76%). The sites of metastasis were bone only in 95% (n = 70) and 5% (n = 4) had visceral metastasis [Table 1].
Table 1Baseline characteristics
|
Variable |
n (%) |
|---|---|
|
Median age (years) (range) |
42 (9-77) |
|
Male |
55(74) |
|
Female |
19 (26) |
|
Symptom at presentation |
|
|
Lump in the neck |
58 (78) |
|
Nasal block |
13 (18) |
|
Others |
3 (4) |
|
Histology |
|
|
WHO Type 2 |
69 (93) |
|
WHO Type (1 or 3) |
5 (7) |
|
T stage |
|
|
T1-T2 |
42 (57) |
|
T3-T4 |
32 (43) |
|
N stage |
|
|
N0-N1 |
18 (24) |
|
N2-N3 |
56 (76) |
|
Site of metastasis |
|
|
Bone only |
70 (95) |
|
Visceral |
4 (5) |
The median PFS was 11 months (range 1–201 months), and the 3-year PFS was better in patients who received chemoradiation (35%) as compared to only radiation (19%). The median OS was 19 months (range 1–201 months), and the 3-year OS rate was 36%. The median OS for patients with bony only metastasis and visceral metastasis was 23 months and 4 months, respectively.
The factors included in the univariate analysis [Table 2] were age, sex, histology, stage, number of sites of bone metastasis, and treatment modality. Univariate analysis showed that type of treatment (chemoradiation) and oligometastatic bone-only disease correlated with improved outcome. Multivariate analysis [Table 3] showed that patients with extensive bone metastasis >3 correlated with poor outcome (hazard ratio-2.03, confidence interval 1.10–3.74, P = 0.022). [Figure 1] and [Figure 2] show the Kaplan–Meier curve for type of treatment and bone metastasis, respectively.
Table 2Univariate analysis
|
Variable |
n |
Median survival (months) |
3-year OS (%) |
HR |
CI |
P |
|---|---|---|---|---|---|---|
|
HR – Hazard ratio; CI – Confidence interval; OS – Overall survival |
||||||
|
Age |
||||||
|
less than42 |
36 |
26 |
44.4 |
1.00* |
0.81-2.29 |
0.233 |
|
>42 |
38 |
18 |
34.2 |
1.36 |
||
|
Sex |
||||||
|
Male |
55 |
19 |
38.2 |
1.00* |
0.59-1.87 |
0.857 |
|
Female |
19 |
22 |
31.6 |
1.05 |
||
|
Histology |
||||||
|
WHO Type 2 |
69 |
19 |
36.2 |
1.00* |
0.17-1.75 |
0.309 |
|
WHO Type (1/3) |
5 |
36 |
40 |
0.54 |
||
|
T stage |
||||||
|
T1-T2 |
42 |
19 |
34.7 |
1.00* |
0.45-1.30 |
0.332 |
|
T3-T4 |
32 |
23 |
38.7 |
0.76 |
||
|
N stage |
||||||
|
N0-N1 |
18 |
23 |
50 |
1.00* |
0.68-2.30 |
0.457 |
|
N2-N3 |
56 |
18 |
35.7 |
1.25 |
||
|
Treatment modality |
||||||
|
Chemoradiation |
53 |
25 |
39.5 |
1.00* |
1.02-3.06 |
0.039 |
|
Radiation only |
21 |
17 |
23.8 |
1.77 |
||
|
Type of metastasis |
||||||
|
Oligometastasis |
51 |
36 |
51 |
1.00* |
1.30-4.14 |
0.004 |
|
Multiple metastasis |
19 |
13 |
15.8 |
2.32 |
||
Multivariate analysis
|
Variable |
HR |
CI |
P |
|---|---|---|---|
|
HR – Hazard ratio; CI – Confidence interval |
|||
|
Treatment modality |
|||
|
Chemoradiation |
1.00* |
0.84-2.77 |
0.161 |
|
Radiation only |
1.53 |
||
|
Type of metastasis |
|||
|
Oligometastasis |
1.00* |
1.10-3.74 |
0.022 |
|
Extensive metastasis |
2.03 |
||
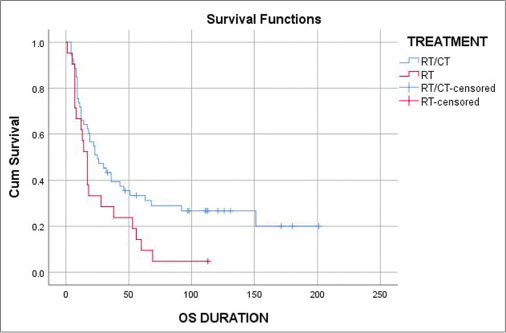
| Figure 1: Kaplan–Meier curve of treatment modality. Blue line - Chemoradiation; Red line - Radiation only
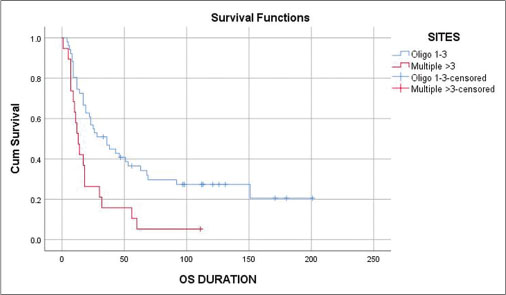
| Figure 2: Kaplan–Meier curve showing type of metastasis. Blue line - Oligometastasis; Red line - Multiple metastasis
Discussion
Nasopharyngeal cancer has a higher incidence of metastasis at presentation than nonnasopharyngeal head-and-neck cancers.[8] [9] [10] [11] In our study, 14.3% of carcinoma of nasopharynx presented with metastasis at presentation. Bone was the most common site (95%) of distant metastasis in our patients. A study from China also reported bone (75%) as the most common site of metastasis.[12]
It is debatable to consider chemoradiation or radiation alone for the treatment of metastatic NPC. A Japanese study[13] showed incorporating radiation in advanced NPC improved the outcome. The National Comprehensive Cancer Network Guidelines recommend concurrent chemoradiation as an option in metastatic NPC.
The median survival of bone-only metastasis was 23 months, whereas, in visceral metastasis, it was 4 months. Consideration to participate in a clinical trial should be strongly recommended in patients with NPC with visceral metastasis.
The majority (72%) of our patients were treated with concurrent chemoradiation with 5-fluorouracil and cisplatin. A meta-analysis of palliative chemotherapy in metastatic NPC showed that the triplet regimen improved response but failed to improve survival and had more toxicity.[14] Among the doublet regimens, the taxane–platinum combination had the best efficacy followed by gemcitabine platinum and then 5-fluorouracil and platinum.[14] Patients who cannot tolerate cisplatin can be considered for carboplatin-based chemotherapy.[15]
In one study, Yeh et al.[13] showed that median and 2 years’ OS of metastatic NPC were 9.7 months and 14%, respectively. In our study, the median survival and 2 years’ OS was 19 months and 45.9%, respectively, and patients treated with concurrent chemoradiation had a better median OS (25 months). Bouaouina et al.[16] showed that cisplatin-based chemoradiation with curative dose improved survival. A case series from Memorial Sloan Kettering Cancer Center[17] also showed that patients treated with chemoradiation had a long-term survival.
A Chinese study[18] showed that patients with >3 metastatic bone lesions have poor OS as compared to patients with <3>
The limitations of this study are the retrospective nature, nonrandomized study, small sample size, physician discretion on type of treatment, lack of EBV testing in tumor, and plasma EBV for surveillance.
Conclusion
Chemoradiation can be an option to treat metastatic NPC. Patients with bone-only oligometastasis (<3>
Conflict of Interest
There are no conflicts of interest.
References
- Kataki AC, Simons MJ, Das AK, Sharma K, Mehra NK. Nasopharyngeal carcinoma in the Northeastern states of India. Chin J Cancer 2011; 30: 106-13
- Haleshappa RA, Thanky AH, Kuntegowdanahalli L, Kanakasetty GB, Dasappa L, Jacob L. Epidemiology and outcomes of nasopharyngeal carcinoma: Experience from a regional cancer center in Southern India. South Asian J Cancer 2017; 6: 122-4
- Kunheri B, Agarwal G, Sunil PS, Nair AR, Pushpaja KU. Nasopharyngeal carcinoma: Experience and treatment outcome with radical conformal radiotherapy from a tertiary care center in India. Indian J Cancer 2017; 54: 502-7
- Paiar F, di Cataldo V, Zei G, Pasquetti EM, Cecchini S, Meattini I. et al. Role of chemotherapy in nasopharyngeal carcinoma. Oncol Rev 2012; 6: e1
- Bensouda Y, Kaikani W, Ahbeddou N, Rahhali R, Jabri M, Mrabti H. et al. Treatment for metastatic nasopharyngeal carcinoma. Eur Ann Otorhinolaryngol Head Neck Dis 2011; 128: 79-85
- Tan WL, Tan EH, Lim DW, Ng QS, Tan DS, Jain A. et al. Advances in systemic treatment for nasopharyngeal carcinoma. Chin Clin Oncol 2016; 5: 21
- Jain A, Chia WK, Toh HC. Immunotherapy for nasopharyngeal cancer-a review. Chin Clin Oncol 2016; 5: 22
- Chen WZ, Zhou DL, Luo KS. Long-term observation after radiotherapy for nasopharyngeal carcinoma (NPC). Int J Radiat Oncol Biol Phys 1989; 16: 311-4
- Fandi A, Altun M, Azli N, Armand JP, Cvitkovic E. Nasopharyngeal cancer: Epidemiology, staging, and treatment. Semin Oncol 1994; 21: 382-97
- Frezza G, Barbieri E, Emiliani E, Silvano M, Babini L. Patterns of failure in nasopharyngeal cancer treated with megavoltage irradiation. Radiother Oncol 1986; 5: 287-94
- Ho JH. An epidemiologic and clinical study of nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 1978; 4: 182-98
- Huang CJ, Leung SW, Lian SL, Wang CJ, Fang FM, Ho YH. Patterns of distant metastases in nasopharyngeal carcinoma. Kaohsiung J Med Sci 1996; 12: 229-34
- Yeh SA, Tang Y, Lui CC, Huang EY. Treatment outcomes of patients with AJCC stage IVC nasopharyngeal carcinoma: Benefits of primary radiotherapy. Jpn J Clin Oncol 2006; 36: 132-6
- Ma SX, Zhou T, Huang Y, Yang YP, Zhan JH, Zhang YX. et al. The efficacy of first-line chemotherapy in recurrent or metastatic nasopharyngeal carcinoma: A systematic review and meta-analysis. Ann Transl Med 2018; 6: 201
- Kua VF, Ismail F, Chee Ee Phua V, Aslan NM. Carboplatin/5-fluorouracil as an alternative to cisplatin/5- fluorouracil for metastatic and recurrent head and neck squamous cell carcinoma and nasopharyngeal carcinoma. Asian Pac J Cancer Prev 2013; 14: 1121-6
- Bouaouina N, Ouni S, Kanoun SB, Neffeti AB, Kermani W, Abdelkefi M. Metastatic nasopharynx cancer at diagnosis: Clinical and prognostic (study of 51 cases). Pan Afr Med J 2018; 29: 155
- Setton J, Wolden S, Caria N, Lee N. Definitive Treatment of Metastatic Nasopharyngeal Carcinoma: Report of 5 Cases with Review of Literature. Head and Neck 2012; 34: 753-57
- Shen L, Dong J, Li S, Wang Y, Dong A, Shu W. et al. M1 stage subdivision and treatment outcome of patients with bone-only metastasis of nasopharyngeal carcinoma. Oncologist 2015; 20: 291-8
Address for correspondence
Publication History
Received: 31 July 2019
Accepted: 19 January 2020
Article published online:
23 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- 1 Kataki AC, Simons MJ, Das AK, Sharma K, Mehra NK. Nasopharyngeal carcinoma in the Northeastern states of India. Chin J Cancer 2011; 30: 106-13
- 2 Haleshappa RA, Thanky AH, Kuntegowdanahalli L, Kanakasetty GB, Dasappa L, Jacob L. Epidemiology and outcomes of nasopharyngeal carcinoma: Experience from a regional cancer center in Southern India. South Asian J Cancer 2017; 6: 122-4
- 3 Kunheri B, Agarwal G, Sunil PS, Nair AR, Pushpaja KU. Nasopharyngeal carcinoma: Experience and treatment outcome with radical conformal radiotherapy from a tertiary care center in India. Indian J Cancer 2017; 54: 502-7
- 4 Paiar F, di Cataldo V, Zei G, Pasquetti EM, Cecchini S, Meattini I. et al. Role of chemotherapy in nasopharyngeal carcinoma. Oncol Rev 2012; 6: e1
- 5 Bensouda Y, Kaikani W, Ahbeddou N, Rahhali R, Jabri M, Mrabti H. et al. Treatment for metastatic nasopharyngeal carcinoma. Eur Ann Otorhinolaryngol Head Neck Dis 2011; 128: 79-85
- 6 Tan WL, Tan EH, Lim DW, Ng QS, Tan DS, Jain A. et al. Advances in systemic treatment for nasopharyngeal carcinoma. Chin Clin Oncol 2016; 5: 21
- 7 Jain A, Chia WK, Toh HC. Immunotherapy for nasopharyngeal cancer-a review. Chin Clin Oncol 2016; 5: 22
- 8 Chen WZ, Zhou DL, Luo KS. Long-term observation after radiotherapy for nasopharyngeal carcinoma (NPC). Int J Radiat Oncol Biol Phys 1989; 16: 311-4
- 9 Fandi A, Altun M, Azli N, Armand JP, Cvitkovic E. Nasopharyngeal cancer: Epidemiology, staging, and treatment. Semin Oncol 1994; 21: 382-97
- 10 Frezza G, Barbieri E, Emiliani E, Silvano M, Babini L. Patterns of failure in nasopharyngeal cancer treated with megavoltage irradiation. Radiother Oncol 1986; 5: 287-94
- 11 Ho JH. An epidemiologic and clinical study of nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 1978; 4: 182-98
- 12 Huang CJ, Leung SW, Lian SL, Wang CJ, Fang FM, Ho YH. Patterns of distant metastases in nasopharyngeal carcinoma. Kaohsiung J Med Sci 1996; 12: 229-34
- 13 Yeh SA, Tang Y, Lui CC, Huang EY. Treatment outcomes of patients with AJCC stage IVC nasopharyngeal carcinoma: Benefits of primary radiotherapy. Jpn J Clin Oncol 2006; 36: 132-6
- 14 Ma SX, Zhou T, Huang Y, Yang YP, Zhan JH, Zhang YX. et al. The efficacy of first-line chemotherapy in recurrent or metastatic nasopharyngeal carcinoma: A systematic review and meta-analysis. Ann Transl Med 2018; 6: 201
- 15 Kua VF, Ismail F, Chee Ee Phua V, Aslan NM. Carboplatin/5-fluorouracil as an alternative to cisplatin/5- fluorouracil for metastatic and recurrent head and neck squamous cell carcinoma and nasopharyngeal carcinoma. Asian Pac J Cancer Prev 2013; 14: 1121-6
- 16 Bouaouina N, Ouni S, Kanoun SB, Neffeti AB, Kermani W, Abdelkefi M. Metastatic nasopharynx cancer at diagnosis: Clinical and prognostic (study of 51 cases). Pan Afr Med J 2018; 29: 155
- 17 Setton J, Wolden S, Caria N, Lee N. Definitive Treatment of Metastatic Nasopharyngeal Carcinoma: Report of 5 Cases with Review of Literature. Head and Neck 2012; 34: 753-57
- 18 Shen L, Dong J, Li S, Wang Y, Dong A, Shu W. et al. M1 stage subdivision and treatment outcome of patients with bone-only metastasis of nasopharyngeal carcinoma. Oncologist 2015; 20: 291-8


 PDF
PDF  Views
Views  Share
Share

