Metabolic toxicities in patients undergoing treatment for nonhematological malignancy: A cross-sectional study
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(04): 256-259
DOI: DOI: 10.4103/0971-5851.195737
Abstract
Objectives: The objective of this study was to evaluate the prevalence of metabolic toxicities in patients with different nonhematological malignancies admitted in oncology ward of a tertiary cancer care center while on treatment. Methods: We did this cross-sectional study over a period of 7 months (January–July 2013) for all adult patients (n = 280) who, while undergoing anti-cancer therapy at our center, got admitted to our oncology inpatient ward with metabolic toxicity. Grading of toxicity was done using National Cancer Institute Common Terminology Criteria for Adverse Events Version 4.0. Results: A total of 46 events of metabolic toxicities were noted in 31 patients over this period. The most common of them was hyperglycemia (n = 10). The others were hypokalemia (n = 9), hyponatremia (n = 9), hypernatremia (n = 5), hyperkalemia (n = 5), tumor lysis syndrome (n = 4), hypercalcemia (n = 2), and grade ≤2 hypomagnesemia (n = 2). Majority of the patients were asymptomatic (n = 26). However, death occurred in five patients. Treatment interruptions took place in 19 patients. Age ≤40 years (P = 0.03), Eastern Cooperative Oncology Group performance status ≥2 (P = 0.023), history of addiction (P = 0.02), comorbidities (P = 0.037) were associated with increased risk of having metabolic toxicities on univariate analysis. While on multivariate analysis, only age, performance status, and history of addiction retained their statistical significance. Age ≤40 years (P = 0.02), use of more than one modality of treatment (P = 0.013), and hyperglycemia (P = 0.037) were associated with higher risk of death. Conclusion: Metabolic toxicities are common phenomena among cancer patients, especially those with young age, comorbidities, and having history of addictions. In young age, they might even be fatal, especially when they are treated with combined modality of treatment.
Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Objectives:
The objective of this study was to evaluate the prevalence of metabolic toxicities in patients with different nonhematological malignancies admitted in oncology ward of a tertiary cancer care center while on treatment.
Methods:
We did this cross-sectional study over a period of 7 months (January–July 2013) for all adult patients (n = 280) who, while undergoing anti-cancer therapy at our center, got admitted to our oncology inpatient ward with metabolic toxicity. Grading of toxicity was done using National Cancer Institute Common Terminology Criteria for Adverse Events Version 4.0.
Results:
A total of 46 events of metabolic toxicities were noted in 31 patients over this period. The most common of them was hyperglycemia (n = 10). The others were hypokalemia (n = 9), hyponatremia (n = 9), hypernatremia (n = 5), hyperkalemia (n = 5), tumor lysis syndrome (n = 4), hypercalcemia (n = 2), and grade ≤2 hypomagnesemia (n = 2). Majority of the patients were asymptomatic (n = 26). However, death occurred in five patients. Treatment interruptions took place in 19 patients. Age ≤40 years (P = 0.03), Eastern Cooperative Oncology Group performance status ≥2 (P = 0.023), history of addiction (P = 0.02), comorbidities (P = 0.037) were associated with increased risk of having metabolic toxicities on univariate analysis. While on multivariate analysis, only age, performance status, and history of addiction retained their statistical significance. Age ≤40 years (P = 0.02), use of more than one modality of treatment (P = 0.013), and hyperglycemia (P = 0.037) were associated with higher risk of death.
Conclusion:
Metabolic toxicities are common phenomena among cancer patients, especially those with young age, comorbidities, and having history of addictions. In young age, they might even be fatal, especially when they are treated with combined modality of treatment.
INTRODUCTION
Burden of cancer is progressively increasing in economically developing countries such as India. The International Agency for Research on Cancer GLOBOCAN project has predicted that India's cancer burden will nearly double in the next 20 years, from slightly over a million new cases in 2012 to more than 1.7 million by 2035.[1] With increasing burden, more number of patients are now-a-days undergoing cancer-directed therapy, which is essentially a sign of increasing awareness and advancement of oncologic facilities in this part of the world. This has led to a steep rise in toxicities of anticancer therapy in these countries. Such toxicities often lead to treatment interruption, deterioration of quality of life of patients, and can be fatal at times. We tried to introspect into the plethora of metabolic toxicities which necessitate admission of patients with different nonhematological malignancies, while on treatment, in the oncology ward of a tertiary cancer care center.
METHODS
This cross-sectional study was carried out over a period of 7 months (January–July 2013) for all adult patients with nonhematological malignancies who, while undergoing treatment, got admitted to our oncology in-patient ward with features of metabolic toxicity. The clinicodemographic details including age, sex, performance status (Eastern Cooperative Group performance status score), socioeconomic background, comorbidities, and addiction were collected. We also reviewed the diagnosis and the treatment charts of these patients. As some of the patients got admitted multiple times with more than one type of metabolic toxicity, we calculated each admission with its cause as an event. Sometimes, there were two toxicities present simultaneously in one patient, so we have counted them as separate events. In the modern era of multimodality management of malignancies, the toxicities of different therapeutic modalities might overlap with each other. Moreover, each of these therapeutic modalities might precipitate the morbidities and toxicities of the other one. In contradistinction to the popular belief, even local oncologic treatment modalities such as surgery and radiation therapy are associated with their own spectrum of metabolic toxicities such as dyselectrolytemia. Hence, we decided to include them in our study. Grading of toxicity was done using National Cancer Institute Common Terminology Criteria for Adverse Events Version 4.0. Impact of different variables such as age, sex, performance status, addiction, comorbidities, primary malignancy, treatment intent, treatment modality on incidence of metabolic toxicities, and death were analyzed. Chi-square and Fisher's exact test were used to evaluate the univariate and multivariate odd's ratio (OR) along with 95% confidence interval (CI) although multivariate analysis was skipped for influence of different factors on death due to extremely small sample size. All P values were two-sided and P < 0.05 was considered to be statistically significant. Statistical Package for Social Sciences version 20.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. Clearance from institutional medical records review board was taken before starting the study. The study procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975 as revised in 2000.
RESULTS
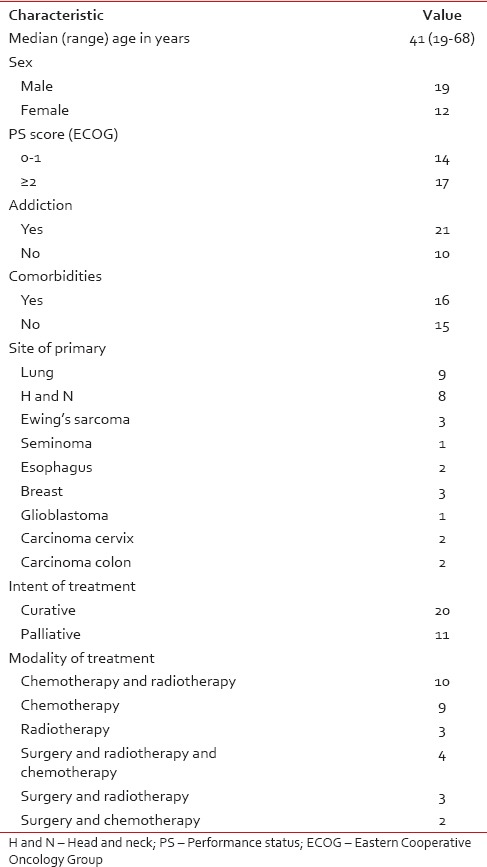
A total of 647 patients were admitted in the specified ward over the period of study, of which, 31 patients got admitted for management of metabolic toxicities and a total of 46 events of metabolic toxicities were noted over this period. The median age of the study cohort was 41 years (range: 19–68 years). The male:female ratio was 1:0.63. Majority of them had a history of addiction (n = 21) or comorbidities (n = 16). Most of them belonged to higher socioeconomic background (n = 18). Majority of the patients (n = 26) were asymptomatic. Among the patients who were symptomatic, the common presenting symptoms were palpitation (n = 3), profuse sweating (n = 2), and dizziness (n = 2). The site of primary including treatment details are described in Table 1.
Table 1
The patient demographics (n=31)
Among the toxicities, the most common toxicities were hyperglycemia (n = 10), followed by hypokalemia (n = 9) and hyponatremia (n = 9). Other common toxicities were hypernatremia (n = 5), hyperkalemia (n = 5), tumor lysis syndrome (n = 4), hypercalcemia (n = 2), hypomagnesemia (n = 2).
Majority of the toxicity events were grade ≤2 (n = 31), of which, the majority were hyperglycemia (n = 7) and hyponatremia (n = 7) followed by hypokalemia (n = 6). The rest were hyperkalemia (n = 4), hypernatremia (n = 3), hypomagnesemia (n = 2), and hypercalcemia (n = 2). Fifteen events were more severe (grade ≥3). They were tumor lysis syndrome (n = 4), hyperglycemia (n = 3), hypokalemia (n = 3), hyponatremia (n = 2), hypernatremia (n = 2), and hyperkalemia (n = 1), respectively. Majority of these grade ≥3 toxicities were nonfatal; however, death occurred in five patients (hypergycemia-2, tumor lysis syndrome-1, hypernatremia-1, and hyperkalemia-1). Treatment interruptions took place in 19 patients (median: 8.8 days; range: 1–24 days). Prolonged hospital admission (>14 days), intensive care, and artificial ventilation support were required in ten, seven, and two patients, respectively. There was no difference in the treatment and pattern of care between symptomatic and asymptomatic patients. The management was decided based on grade and type of the toxicity.
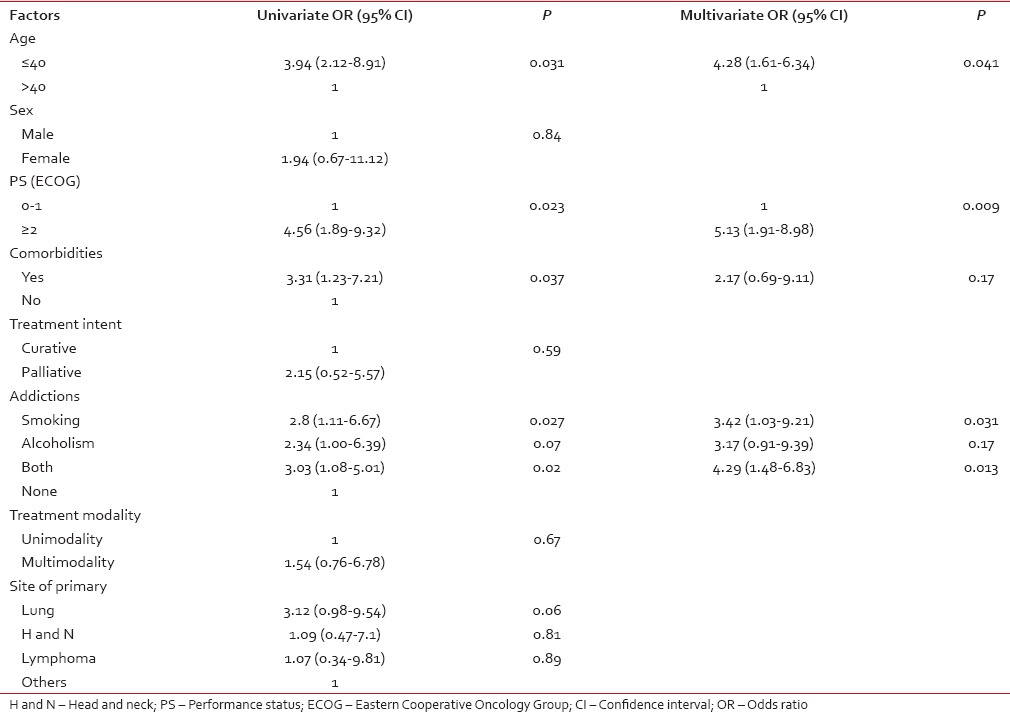
Univariate analysis revealed that age, performance status, addiction history, and comorbidities had a significant influence on incidence of such toxicities; however, on multivariate analysis age, performance status, and history of both alcoholism and smoking retained their statistical significance [Table 2].
Table 2
Odd's ratio of different factors related to metabolic toxicities
 Among different factors analyzed, age ≤40 years (univariate OR: 3.17; 95% CI: 1.43–9.01; P = 0.02), use of combined modality treatment (OR: 4.51; 95% CI: 2.91–7.64; P = 0.013), and hyperglycemia (OR: 3.39; 95% CI: 1.27–8.41; P = 0.037) were associated with higher risk of death in these patients.
Among different factors analyzed, age ≤40 years (univariate OR: 3.17; 95% CI: 1.43–9.01; P = 0.02), use of combined modality treatment (OR: 4.51; 95% CI: 2.91–7.64; P = 0.013), and hyperglycemia (OR: 3.39; 95% CI: 1.27–8.41; P = 0.037) were associated with higher risk of death in these patients.DISCUSSION
The present study depicts the incidence and outcome of metabolic toxicities in cancer patients undergoing radical anti-cancer treatment, in a real world situation, in a developing nation. Although a number of publications[2,3,4] exist on hematological toxicities of anti-cancer treatment, literature on metabolic toxicities is sparse. Treatment of malignancies has taken a few long strides over the past two decades, however, it has unveiled newer challenges including different metabolic abnormalities.[5,6,7] Most of the metabolic toxicities described till date are related to the paraneoplastic syndrome of different malignancies such as hypercalcemia and syndrome of inadequate antidiuretic hormone secretion. The present study, to the best of our knowledge, is the first from this subcontinent to describe the spectrum of metabolic toxicities related to treatment of different nonhematological malignancies.
The present study shows that patients with young age are more susceptible to metabolic toxicities and may succumb to death. This seeming paradox can be explained by the use of more aggressive treatment approach in this age group. Moreover, majority of these patients often have underlying concurrent illnesses such as diabetes which negatively influence the overall prognosis in these patients.[8]
The association of addiction with treatment-related toxicities has also been demonstrated in previous studies.[9,10] Poor performance status in cancer patients may be due to underlying compromised nutritional status, heavy disease burden, or concurrent comorbidities. These are the potential factors which can explain the correlation of poor performance status with metabolic toxicities.
In India, quality cancer care is mostly concentrated in the major cities which compel the patients to travel a long distance for comprehensive cancer care. This results in loss of salary for the caregivers and further financial burden adding to the already existing financial constraints toward cost of treatment. Major centers also face the burden of large number of patients thus creating a substantial waiting time for diagnosis, intervention, and therapy.[11] Incidence of toxicities during treatment, therefore, creates additional challenges both for the patients and caregivers, owing to treatment interruption, prolonged hospital stay, and extra expenses of treating these toxicities. These factors also play a contributory role to India's disproportionately high cancer incidence-to-mortality ratios. The aim of the clinical trials and studies done in the next decade should therefore be directed not only to improve the tumor control but also to limit the treatment accompaniments and therefore improve the overall therapeutic ratio.
The study has its own limitation of being a retrospective study with a small sample size, heterogeneity in the cohort demographics, and management protocols. However, studies like this underscore the importance of appropriate selection of patients at the beginning with clear distinction between radical and palliative approach so as to avoid such toxicities. Finally, one must not overlook the cost:benefit ratio of any treatment approach in these patients and should consider providing an optimally safe therapy to an individual along with incorporation of palliative care whenever possible in the plan of action from the very beginning.
CONCLUSION
Treatment-related toxicities result in interruptions of the proposed therapeutic regimen; they can be fatal at times. Metabolic toxicity is one of the major concerns for those undergoing radical anti-cancer therapy in developing nations. Young age, poor performance status, and previous history of addiction are strongly related with incidence of such toxicities.
Financial support and sponsorship
Nil.


 PDF
PDF  Views
Views  Share
Share

