Mental Wellbeing among Children with Cancer during COVID-19 Pandemic in Indonesia: A Cross-sectional Study
CC BY 4.0 · Indian J Med Paediatr Oncol 2025; 46(01): 040-048
DOI: 10.1055/s-0043-1768053
Abstract
Introduction Coronavirus disease 2019 (COVID-19) has affected both physical and mental aspect of people worldwide, especially the high-risk group such as pediatric cancer patients. Children with cancer were considered both clinically and mentally vulnerable during this pandemic. They were also affected by the self-isolation, quarantine, and social distancing policy taken as a respond to public threat.
Objectives To evaluate the impact of social distancing and health protocol during COVID-19 on the mental health profile of children with cancer in Indonesia.
Materials and Methods A cross-sectional study evaluating the mental health of children with cancer during COVID-19 pandemic was conducted in Cipto Mangunkusumo Hospital, Jakarta, Indonesia from June to September 2020. An online questionnaire was used to collect demographics of parents and children, children's Strength and Difficulties Questionnaire (SDQ) score, and parents' Self-Reporting Questionnaire (SRQ). SDQ score consists of five subscales, including the emotional symptoms, conduct problems, hyperactivity, peer relationships problems and prosocial behavior. Cancer types were grouped into retinoblastoma, nonretinoblastoma (other solid tumors), and leukemia.
Results There were 156 valid responses, consisting of 42 patients with retinoblastoma, 34 patients with nonretinoblastoma (other solid tumors), and 80 patients with leukemia. Pandemic-related lifestyle changes did not significantly impact emotional or behavioral problems. Children with normal total SDQ (odds ratio [OR]: 473, p = 0.001) and emotional scores (OR: 3.19, p = 0.07) had parents with normal SRQ scores (<6 class="i" xss=removed>p = 0.01). On the contrary, leukemia inpatients had better prosocial scores than outpatients (p = 0.03). More bilateral retinoblastoma patients (p = 0.04) with longer duration of cancer diagnosis (p = 0.03) faced peer problems.
Conclusions Our study revealed that lifestyle changes during early COVID-19 pandemic were not major factors impacting emotional and behavioral problems in children with cancer. However, disease-related factors pose great challenges; thus, a holistic mental health support system should be available to both children and parents.
Keywords
mental health - pediatric cancer patients - COVID-19 - psychiatry - hematology - medical oncology - ophthalmologyAuthors' Contributions
R. S. S., T. T. S., T. W., S. D. E., and I. S. W. designed and conceptualized the study. R. M., A. S. N., and N. S. carried out the survey. R. S. S., T. T. S., T. W., S. D. E., I. S. W., N. S., and S. T. analyzed the data and wrote and edited the manuscript. All authors have read and approved this manuscript.
Supplementary MaterialPublication History
Article published online:
28 April 2023
© 2023. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Awareness, Psychological State, and Coping Skills among the Frontline Doctors during the COVID-19 Pandemic—A Cross-Sectional StudyMittal Apurva, Journal of Health and Allied Sciences NU
- Knowledge, Attitude, and Practice Toward Mask-Wearing Behaviors During Covid-19 Pandemic Among Mangalore Residents: A Cross-Sectional StudyNidhish Krishna, Journal of Health and Allied Sciences NU
- Food Insecurity Associated with Evening Types: Cross-sectional Study with University Students during the COVID-19 PandemicG. C. S. Leão, Aktuelle Neurologie, 2023
- Reading fluency during the COVID-19 pandemic: a longitudinal and cross-sectional analysisLuciana Mendonça Alves, VCOT Open, 2022
- Use of Natural Products During the COVID-19 Pandemic: An Exploratory Cross-Sectional Study in Saudi ArabiaO Alghamdi, Planta Medica, 2022
- Tracking Turnover Among Health Care Workers During the COVID-19 Pandemic: A Cross-sectional StudyBianca K. Frogner, JAMA Health Forum, 2022
- Moral Stress among Swedish Health Care Workers During the COVID-19 Pandemic: A Cross-Sectional StudyFilip K. Arnberg, Scandinavian Journal of Work and Organizational Psychology, 2023
- Impact on mental health due to COVID-19 pandemic: A cross-sectional study in BangladeshRefat Pathan, Clinical eHealth, 2023
- Children and Teens Struggling with Mental Health During COVID-19 PandemicJoan Stephenson, JAMA Health Forum, 2021
- Mental Well-Being Among Adversity-Exposed Adolescents During the COVID-19 PandemicJulia H. Raney, JAMA Network Open, 2024
Abstract
Introduction Coronavirus disease 2019 (COVID-19) has affected both physical and mental aspect of people worldwide, especially the high-risk group such as pediatric cancer patients. Children with cancer were considered both clinically and mentally vulnerable during this pandemic. They were also affected by the self-isolation, quarantine, and social distancing policy taken as a respond to public threat.
Objectives To evaluate the impact of social distancing and health protocol during COVID-19 on the mental health profile of children with cancer in Indonesia.
Materials and Methods A cross-sectional study evaluating the mental health of children with cancer during COVID-19 pandemic was conducted in Cipto Mangunkusumo Hospital, Jakarta, Indonesia from June to September 2020. An online questionnaire was used to collect demographics of parents and children, children's Strength and Difficulties Questionnaire (SDQ) score, and parents' Self-Reporting Questionnaire (SRQ). SDQ score consists of five subscales, including the emotional symptoms, conduct problems, hyperactivity, peer relationships problems and prosocial behavior. Cancer types were grouped into retinoblastoma, nonretinoblastoma (other solid tumors), and leukemia.
Results There were 156 valid responses, consisting of 42 patients with retinoblastoma, 34 patients with nonretinoblastoma (other solid tumors), and 80 patients with leukemia. Pandemic-related lifestyle changes did not significantly impact emotional or behavioral problems. Children with normal total SDQ (odds ratio [OR]: 473, p = 0.001) and emotional scores (OR: 3.19, p = 0.07) had parents with normal SRQ scores (<6 class="i" xss=removed>p = 0.01). On the contrary, leukemia inpatients had better prosocial scores than outpatients (p = 0.03). More bilateral retinoblastoma patients (p = 0.04) with longer duration of cancer diagnosis (p = 0.03) faced peer problems.
Conclusions Our study revealed that lifestyle changes during early COVID-19 pandemic were not major factors impacting emotional and behavioral problems in children with cancer. However, disease-related factors pose great challenges; thus, a holistic mental health support system should be available to both children and parents.
Keywords
mental health - pediatric cancer patients - COVID-19 - psychiatry - hematology - medical oncology - ophthalmologyIntroduction
The coronavirus disease 2019 (COVID-19) pandemic has posed a global threat since December 2019. It affected both physical and mental health of the public, leading to detrimental effects on quality of life. The World Health Organization expressed concern over the psychosocial consequences of COVID-19, as it stated that the new measures including quarantine and social distancing have disrupted people's routines, thus increasing the feeling of anxiety, depression, loneliness, insomnia, and self-harm.[1] [2] [3] [4] [5]
Following government responses to COVID-19 on schools, educational institutions, and closure of public places, ample evidence has revealed the psychological impact of COVID-19 pandemic toward children and adolescents manifesting as behavioral and emotional problems.[6] [7] [8] [9] [10] A study showed that children who have more highly educated parents, live in big cities, come from either high- or low-income households, and have parents with mental problems are the most vulnerable group during the pandemic. There is also evidence that extended period of parental stress during the pandemic is related to child behavioral problems.[11]
Children and adolescents faced emotional struggles while experiencing social isolation and disrupted education. Children encountered fear, uncertainties, and isolation, resulting in conditions such as poor appetite, physical discomfort, agitation and inattention, clinginess, separation problems, and poor sleep.[6] [7] [8] [9] [10] In published research on stress levels among students during the pandemic, the values ranged from 24.7 to 71.2%, mostly related to the adaptation of long-distance learning.[12] [13] [14] In addition, the increased use of digital devices during lockdown has also been used as indicator of developing the internet addiction, gaming disorder, anxiety, depression, irritability, sleep disturbance, and poor mental health in children during the pandemic.[12] [13] [14] [15]
Pediatric cancer patients are not indifferent to the dramatic impact of COVID-19. The uncertainty regarding their condition is now worsened by the risk of contracting viral infection and disruption in cancer treatment protocol.[16] [17] Even before the pandemic, children with cancer were already at risk of developing mental health disorders precipitated by the anxieties following diagnosis, treatment, and alteration of daily activities. The side effects of cancer treatments, including surgery, chemotherapy, and radiotherapy, may lead to cognitive problems, behavioral disorders, and poor coping skills. There are also increased levels of depression, anxiety, and concerns related to mortality.[18] [19] [20]
Children with cancer are considered as clinically vulnerable during this pandemic due to their immunocompromised status caused by cancer and anticancer treatments.[17] [20] [21] Hence, they are recommended to undergo stricter rules to keep them safe by always remaining at home and avoiding contact with anyone beyond their household, except attending medical care in the hospital. There is an emerging concern regarding the damage of these measures on the mental wellbeing of pediatric cancer patients.[16] [22] [23] [24] [25] A study in Milan showed that majority of adolescent cancer patients were worried and felt personally at risk during this pandemic, as they encountered high levels of stress and anxiety, facing dilemmas regarding continuation of their treatment and access to health care facility under these threatening circumstances.[17] [22] [23] [24] [25] [26]
Not only the patients but also the families of children with cancer experience challenges in balancing their life during the pandemic. A study in UK found that parents/caregivers were worried that their children would get infected by the virus and felt that hospital was not a safe place, thus increasing parents' anxiety and concerns about their child's care.[26] [27] Another study also stated that hospital restriction increased parent's psychosocial distress during the pandemic, especially regarding the risk of suboptimal care received by their children.[27] [28] [29]
There are limited data on the mental health status of pediatric patients with cancer during the COVID-19 pandemic. Therefore, we conducted the first Indonesian study that aimed to evaluate the experience and psychological impact of COVID-19 toward children with cancer and their parents in Indonesia. These findings can provide comprehensive foundation for the development of mental health programs to support children with cancer during this pandemic.
Materials and Methods
Study Design and Data Collection
A cross-sectional survey study of parents and children with cancer diagnosed between 2015 and 2020 was conducted to assess their mental health and experience during the social isolation of COVID-19 pandemic. The data were collected by clinicians who are members of the research team (R. M., A. S. N., N. S.) from June to September 2020, 3 months after the start of social distancing and lockdown implementation in Indonesia.
The variables in our study are as follows: gender, age, education level, parent's marital status, time from diagnosis to data collection (TDD), treatment status, place of stay during self-isolation, duration of study from home per day, total duration of using gadget per day, cancer staging, treatment received, phase of treatment, number of eyes affected (retinoblastoma patients), children's Strength and Difficulties Questionnaire (SDQ) score, emotional problems score, conduct problems score, hyperactivity score, peer problems score, prosocial score, and parents' Self-Reporting Questionnaire (SRQ) score. The primary outcomes of this study are the association between patient's clinical characteristics (cancer staging, types of treatment, and TDD) and their total SDQ score (and its domain) during the COVID-19 self-isolation period. The secondary outcomes are the patients' and their parents' demographic characteristics (gender, age, total screen time, treatment status, place of stay during pandemic, marital status, parents' marital status, and parent's SRQ score) and their association with the SDQ score (and its domain), in addition to the comparison between each cancer group.
The inclusion criteria of this study were parents and their children aged between 0 and 18 years, who were clinically diagnosed with cancer (either were still undergoing treatment or had completed their treatment) and were literate and able to respond to questions in Indonesian language. Patients were recruited from Pediatric Oncology and/or Pediatric Ophthalmology Department outpatient clinics, Ciptomangunkusumo Hospital. We exclude parents and children who refused to complete the questionnaire or are not able to comprehend and respond to questions.
Instrument
We gathered information on parents' and children's demographics and then evaluated their experiences during the COVID-19 pandemic including the social distancing practice, work/study from home practice, problems, and hopes during this pandemic. A questionnaire was developed to address the lifestyle-related behavior changes during the pandemic including the duration of work from home and study from home, source of COVID-19 information, and problems experienced during the pandemic.
The main outcome, which is the mental condition of the pediatric cancer patients, was assessed using validated questionnaire. The survey was conducted via an online survey tool (Google Forms) in Indonesian language, available in the [Appendix 1]. Before we performed the statistical analyses, all patient-related medical information was validated through the medical record.
SDQ for Children
The emotional and behavioral problems of the children were assessed using the SDQ.[30] [31] The SDQ questionnaire was each categorized based on the age of the children, which consists of a parent-completed SDQ for ages 2 to 4 years old[30] and 4 to 11 years old,[31] and a self-completed SDQ for ages 11 to 18 years old. SDQ had been officially translated and validated into Indonesian language by one of our authors (T. W.). It is available as online assessment tool for children at www.sdqinfo.com. SDQ for ages 11 to 18 years was filled in by the children themselves, meanwhile SDQ for ages 2 to 11 years was filled in by their parents.[30] [31]
The SDQ questionnaire consists of 25 questions on Likert scale (0 = not true; 1 = somewhat true; 2 = certainly true). It was divided into two major parts including the difficulties domains, which consist of 20 questions (emotional problems, conduct problems, hyperactivity scale, and peer problems), and strength domain, which comprises 5 questions (prosocial scale). The total score for the difficulties domains ranged from 0 to 40. The newer four-band categorization was used as cutoff points for total SDQ score and its domain in our study. The initial three-band categorization divided SDQ scores as “normal,” “borderline,” and “abnormal,” with cutoff points such that 80% of children population scored “normal,” 10%“borderline,” and 10%“abnormal.” New four-band classification with cutoff points such that 80%, of children population were “close to average,” 10%“slightly raised,” 5%“high,” and 5%“very high” for all scales except prosocial, which is 80%“close to average,” 10%“slightly lowered,” 5%“low,” and 5%“very low,” was used.[30] [31]
SRQ for Parents
Parents also completed the SRQ consisting of 20 yes/no questions, which has been translated and validated in Indonesian language, with a cutoff score of 6 to be indicative of common mental disorder.[32]
Definitions
TDD was defined as the duration of time since the patient was diagnosed with cancer until the data were obtained. We classified patients into three groups: retinoblastoma, leukemia, and nonretinoblastoma (other solid tumors) group. We defined combined therapy in both retinoblastoma and nonretinoblastoma (other solid tumors) groups as combination of surgical, chemotherapy, radiotherapy, and other modalities. Monotherapy in the nonretinoblastoma (other solid tumors) group was defined as surgical only or chemotherapy only. The retinoblastoma group was classified into early (stage 1 and 2) and advanced (stage 3 and 4). Cancer staging in nonretinoblastoma (other solid tumors) diagnosis was grouped into early to advanced (stages 1, 2, and 3) and late (stage 4). The treatment phase in leukemia group was categorized into two groups based on the treatment received, namely, inpatient, which consists of induction, consolidation, and intensification phase, and outpatient, which consists of maintenance and remission phase.
Statistical Analyses
From questionnaire results, we excluded housewives and unemployed in the analysis of “work from home” variable. We also excluded patients who received chemotherapy only in the retinoblastoma group from the analysis of “treatment received for cancer” as they have not completed treatment regimen.
Statistical analysis was performed with SPSS version 24.0 for Mac (SPSS Inc., Chicago, IL, United States). Categorical data were reported in the form of frequency (percentage) and assessed using chi-square (χ2) test or Fisher's exact test. Continuous variables were reported in the form of mean ± standard deviation or median (range). Normality of the data was evaluated by using Shapiro–Wilk test. Normally distributed data were analyzed using one-way analysis of variance. Nonnormally distributed data were analyzed using Kruskal–Wallis test.
Analysis was conducted according to the cancer diagnosis, grouped as retinoblastoma, nonretinoblastoma (other solid tumors), and leukemia. Descriptive statistics were carried out to summarize all variables included based on the diagnosis groups. We performed a bivariate analysis and risk assessment on parents' and children's characteristics toward children's SDQ score. A p-value < 0.05 was considered statistically significant.
Ethics
This study has been approved by the Research Ethic Committee in Cipto Mangunkusumo Hospital, Jakarta (KET-476/UN2.F1/ETIK/ PPM.00.02/2020), as listed in [Appendix 2] and conducted in accordance with the tenets of the Declaration of Helsinki. All participants were provided study information and completed electronic consent before completing the online survey.
Results
Patient's Clinical Characteristics
A total of 166 patients were assessed for enrollment. Ten patients were excluded and 156 patients who met the eligible criteria were included in the study, as seen in [Fig. 1]. Among them, 42 patients belonged to the retinoblastoma group, 34 patients were in the nonretinoblastoma (other solid tumors) group, and 80 patients were diagnosed with leukemia. Half of our retinoblastoma patients suffered from unilateral cases (50%, n = 21). Approximately 85.7%, (n = 36) of the children were in the early stage (stages 1 and 2) of the disease. The combination of enucleation and chemotherapy was the most common treatment modality given in accordance with disease stage. Meanwhile, the diagnosis for the other (nonretinoblastoma) solid tumor group in our study included neuroblastoma (26.5%, n = 9), lymphoma (23.53%, n = 8), rhabdomyosarcoma (11.76%, n = 4), osteosarcoma (11.76%, n = 4), and others (26.47%, n = 9). Around 70.58%, (n = 24) came to the hospital during late stage of the disease (stages 3 and 4). The most common types of treatment given to these patients were chemotherapy only (41.2%, n = 14) and combination of chemotherapy and surgery (23.5%, n = 8). Lastly, 75.75%, (n = 59) of leukemia patients in our study were in maintenance phase of chemotherapy treatment. Patient's demographic characteristics are listed in [Table 1]. Patients' clinical information based on the cancer diagnosis is summarized in [Table 2].
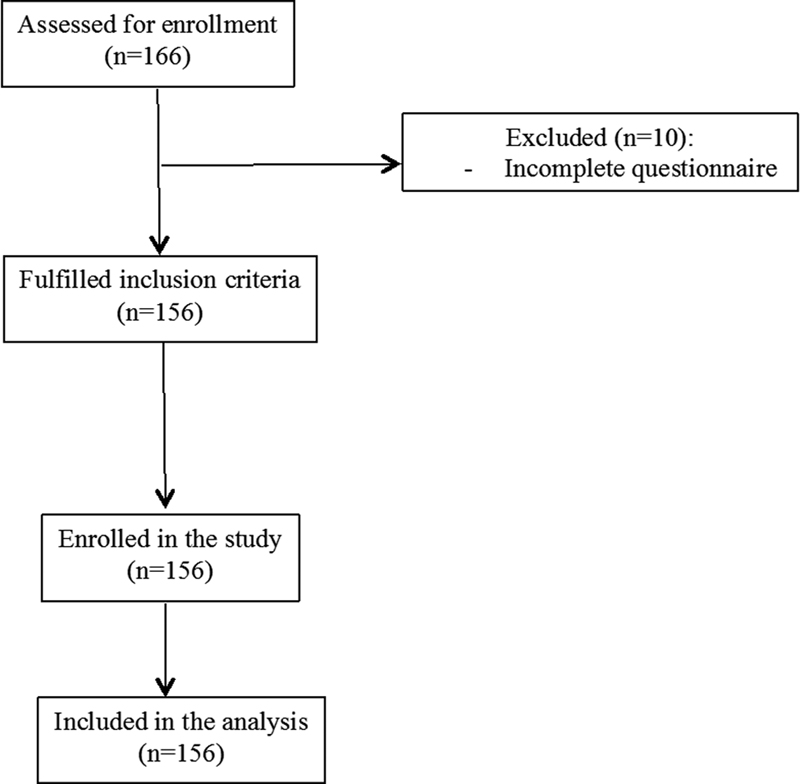
| | Fig 1 Consort diagram showing participants enrollment.|
|
Retinoblastoma (n = 42) |
Solid tumor (nonretinoblastoma) (n = 34) |
Leukemia (n = 80) |
|
|---|---|---|---|
|
Gender |
|||
|
Male |
26 (61.9%) |
20 (58.8%) |
47 (58.8%) |
|
Female |
16 (38.1%) |
14 (41.2%) |
33 (41.3%) |
|
Age (y) |
4 (1–11) |
5 (1–17) |
6 (1–16) |
|
0–5 |
33 (78.6%) |
20 (58.8%) |
34 (42.5%) |
|
6–9 |
8 (19%) |
3 (8.8%) |
17 (21.3%) |
|
10–17 |
1 (2.4%) |
11 (32.4%) |
29 (36.2%) |
|
Education level |
|||
|
Preschool |
29 (69%) |
19 (55.9%) |
30 (37.5%) |
|
Kindergarten |
7 (16.7%) |
2 (5.9%) |
9 (11.3%) |
|
Elementary school |
6 (14.3%) |
4 (11.8%) |
25 (31.3%) |
|
Junior high school |
0 (0%) |
8 (23.5%) |
9 (11.3%) |
|
Senior high school |
0 (0%) |
1 (2.9%) |
6 (7.5%) |
|
University |
0 (0%) |
0 (0%) |
1 (1.3%) |
|
Time from diagnosis to data collection (mo) |
24 (1–96) |
12 (3–48) |
17.5 (1–72) |
|
Treatment status |
|||
|
On treatment |
15 (35.7%) |
30 (88.2%) |
75 (93.8%) |
|
Survivor |
27 (64.3%) |
4 (11.8%) |
5 (6.3%) |
|
Place of stay |
|||
|
Private housing |
16 (38.09%) |
9 (26.47%) |
40 (50%) |
|
Temporary housing |
26 (61.91%) |
25 (73.53%) |
40 (50%) |
|
Duration of study from home per day (min) |
0 (0–120) |
0 (0–240) |
45 (0–300) |
|
Total duration of using gadget per day (min) |
60 (0–540) |
80 (0–540) |
120 (0–780) |
Retinoblastoma patients (n = 42) |
|
|---|---|
|
Number of eyes affected |
|
|
Unilateral |
21 (50%) |
|
Bilateral |
21 (50%) |
|
Cancer staging |
|
|
1 |
21 (50%) |
|
2 |
15 (35.7%) |
|
3 |
4 (9.5%) |
|
4 |
1 (2.4%) |
|
Treatment received for cancer |
|
|
Enucleation |
10 (23.8%) |
|
Enucleation, chemotherapy |
22 (52.4%) |
|
Enucleation, chemotherapy, laser |
6 (14.3%) |
|
Enucleation, chemotherapy, radiation |
2 (4.8%) |
|
Chemotherapy |
2 (4.8%) |
|
Other solid tumor (nonretinoblastoma) patients (n = 34) |
|
|
Diagnosis |
|
|
Neuroblastoma |
9 (26.47%) |
|
Lymphoma |
8 (23.53%) |
|
Rhabdomyosarcoma |
4 (11.76%) |
|
Osteosarcoma |
4 (11.76%) |
|
Others |
9 (26.47%) |
|
Cancer staging |
|
|
1 |
1 (2.94%) |
|
2 |
9 (26.47%) |
|
3 |
12 (35.29%) |
|
4 |
12 (35.29%) |
|
Treatment received for cancer |
|
|
Chemotherapy |
14 (41.2%) |
|
Chemotherapy, operation |
8 (23.5%) |
|
Chemotherapy, radiation |
5 (14.7%) |
|
Chemotherapy, operation, radiation |
3 (8.82%) |
|
Operation |
4 (11.76%) |
|
Leukemia patients (n = 80) |
|
|
Phase of treatment |
|
|
Induction |
3 (3.75%) |
|
Consolidation |
11 (13.75%) |
|
Intensification |
2 (2.5%) |
|
Maintenance |
59 (73.75%) |
|
Remission |
5 (6.25%) |
|
Treatment received for cancer |
|
|
Chemotherapy |
80 (100%) |
References
- Amsalem D, Dixon L, Neria Y. The coronavirus disease 2019 (COVID-19) outbreak and mental health: current risks and recommended actions. JAMA Psychiatry 2021; 78 (01) 9-10
- Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr 2020; 174 (09) 819-820
- Jiao WY, Wang LN, Liu J. et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr 2020; 221: 264-266 .e1
- Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health 2021; 30 (01) 1-2
- Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med 2020; 383 (06) 510-512
- Wiguna T, Anindyajati G, Kaligis F. et al. Brief research report on adolescent mental well-being and school closures during the COVID-19 pandemic in Indonesia. Front Psychiatry 2020; 11: 598756
- Garcia de Avila MA, Hamamoto Filho PT, Jacob FLDS. et al. Children's anxiety and factors related to the COVID-19 pandemic: an exploratory study using the children's anxiety questionnaire and the numerical rating scale. Int J Environ Res Public Health 2020; 17 (16) 5757
- Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health 2020; 17 (22) 8479
- Ramaswamy S, Seshadri S. Children on the brink: risks for child protection, sexual abuse, and related mental health problems in the COVID-19 pandemic. Indian J Psychiatry 2020; 62 (9, suppl 3): S404-S413
- Yue J, Zang X, Le Y, An Y. Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID-19) outbreak in China. Curr Psychol 2022; 41 (08) 5723-5730
- Sifat RI, Ruponty MM, Rahim Shuvo MK, Chowdhury M, Suha SM. Impact of COVID-19 pandemic on the mental health of school-going adolescents: insights from Dhaka city, Bangladesh. Heliyon 2022; 8 (04) e09223
- Limone P, Toto GA. Psychological and emotional effects of digital technology on children in COVID-19 pandemic. Brain Sci 2021; 11 (09) 1126
- Rutkowska A, Cieślik B, Tomaszczyk A, Szczepańska-Gieracha J. Mental health conditions among e-learning students during the COVID-19 pandemic. Front Public Health 2022; 10: 871934
- Kishida K, Tsuda M, Waite P, Creswell C, Ishikawa SI. Relationships between local school closures due to the COVID-19 and mental health problems of children, adolescents, and parents in Japan. Psychiatry Res 2021; 306: 114276
- Pandya A, Lodha P. Social connectedness, excessive screen time during COVID-19 and mental health: a review of current evidence. Front Hum Dyn 2021; 3: 684137
- Moreira DC, Millen GC, Sands S, Kearns PR, Hawkins DS. The care of children with cancer during the COVID-19 pandemic. Am Soc Clin Oncol Educ Book 2021; 41: 1-10
- Mirlashari J, Ebrahimpour F, Salisu WJ. War on two fronts: experience of children with cancer and their family during COVID-19 pandemic in Iran. J Pediatr Nurs 2021; 57: 25-31
- Mavrides N, Pao M. Updates in paediatric psycho-oncology. Int Rev Psychiatry 2014; 26 (01) 63-73
- Young AM, Ashbury FD, Schapira L, Scotté F, Ripamonti CI, Olver IN. Uncertainty upon uncertainty: supportive Care for Cancer and COVID-19. Support Care Cancer 2020; 28 (09) 4001-4004
- Mertens A, Gilleland Marchak J. Mental health status of adolescent cancer survivors. Clin Oncol Adolesc Young Adults 2015; 5: 87-95
- Amicucci M, Mastronuzzi A, Ciaralli I. et al. The management of children with cancer during the COVID-19 pandemic: a rapid review. J Clin Med 2020; 9 (11) 3756
- Liu Y, Sundquist J, Sundquist K, Zheng D, Ji J. Mental health outcomes in parents of children with a cancer diagnosis in Sweden: A nationwide cohort study. EClinicalMedicine 2022; 55: 101734
- Garutti M, Cortiula F, Puglisi F. Seven shades of black thoughts: COVID-19 and its psychological consequences on cancer patients. Front Oncol 2020; 10: 1357
- Tsamakis K, Gavriatopoulou M, Schizas D. et al. Oncology during the COVID-19 pandemic: challenges, dilemmas and the psychosocial impact on cancer patients. Oncol Lett 2020; 20 (01) 441-447
- Wang Y, Duan Z, Ma Z. et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl Psychiatry 2020; 10 (01) 263
- Darlington AE, Morgan JE, Wagland R. et al. COVID-19 and children with cancer: parents' experiences, anxieties and support needs. Pediatr Blood Cancer 2021; 68 (02) e28790
- Davies J, O'Connor M, Halkett GKB, Kelada L, Gottardo NG. Parents' experiences of childhood cancer during the COVID-19 pandemic: an Australian perspective. J Pediatr Psychol 2022; 47 (02) 148-157
- Kotecha RS. Challenges posed by COVID-19 to children with cancer. Lancet Oncol 2020; 21 (05) e235
- van Gorp M, Maurice-Stam H, Teunissen LC. et al. No increase in psychosocial stress of Dutch children with cancer and their caregivers during the first months of the COVID-19 pandemic. Pediatr Blood Cancer 2021; 68 (02) e28827
- Scoring the Strengths & Difficulties Questionnaire for 2–4 years old. Development and Well-Being Assessment (DAWBA). October 2015. Accessed March 3, 2021 at: https://sdqinfo.org
- Scoring the Strengths & Difficulties Questionnaire for age 4–17 or 18 + . Development and Well-Being Assessment (DAWBA). June 2016. Accessed March 3, 2021 at: https://sdqinfo.org
- Domingues-Montanari S. Clinical and psychological effects of excessive screen time on children. J Paediatr Child Health 2017; 53 (04) 333-338
- Bekar P, Erkul M, Efe E. Investigation of coronavirus anxiety and caregiving burden among the parents of children with cancer during the COVID-19 outbreak: a descriptive and cross-sectional study. Eur J Cancer Care (Engl) 2022; 31 (04) e13600
- Zijlmans J, Teela L, van Ewijk H. et al. Mental and social health of children and adolescents with pre-existing mental or somatic problems during the COVID-19 pandemic lockdown. Front Psychiatry 2021; 12: 692853
- Li X, Vanderloo LM, Maguire JL. et al; TARGet Kids! Collaboration. Public health preventive measures and child health behaviours during COVID-19: a cohort study. Can J Public Health 2021; 112 (05) 831-842
- Bergmann C, Dimitrova N, Alaslani K. et al. Young children's screen time during the first COVID-19 lockdown in 12 countries. Sci Rep 2022; 12 (01) 2015
- Twenge JM, Farley E. Not all screen time is created equal: associations with mental health vary by activity and gender. Soc Psychiatry Psychiatr Epidemiol 2021; 56 (02) 207-217
- Feng Y, Zhou C, Jia R, Wang Y, Fan X. Quality of life (QoL) and psychosocial outcomes in adult survivors of unilateral retinoblastoma (RB) in China. J Ophthalmol 2020; 2020: 4384251
- van Dijk J, Imhof SM, Moll AC. et al. Quality of life of adult retinoblastoma survivors in the Netherlands. Health Qual Life Outcomes 2007; 5: 30
- Baytan B, Aşut Ç, Çırpan Kantarcıoğlu A, Sezgin Evim M, Güneş AM. Health-related quality of life, depression, anxiety, and self-image in acute lymphocytic leukemia survivors. Turk J Haematol 2016; 33 (04) 326-330
- Hutchinson AD, Pfeiffer SM, Wilson C. Cancer-related cognitive impairment in children. Curr Opin Support Palliat Care 2017; 11 (01) 70-75
- Cheung YT, Sabin ND, Reddick WE. et al. Leukoencephalopathy and long-term neurobehavioural, neurocognitive, and brain imaging outcomes in survivors of childhood acute lymphoblastic leukaemia treated with chemotherapy: a longitudinal analysis. Lancet Haematol 2016; 3 (10) e456-e466
- Bloom J, Lachman A, Gaxo E, Pillay J, Seedat S. Child, adolescent, and caregiver mental health difficulties and associated risk factors early in the COVID-19 pandemic in South Africa. Child Adolesc Psychiatry Ment Health 2022; 16 (01) 65
- Kauhanen L, Wan Mohd Yunus WMA, Lempinen L. et al. A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur Child Adolesc Psychiatry 2023; 32 (06) 995-1013
- Bignardi G, Dalmaijer ES, Anwyl-Irvine AL. et al. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch Dis Child 2020; 106 (08) 791-797
- Sahril N, Ahmad NA, Idris IB, Sooryanarayana R, Abd Razak MA. Factors associated with mental health problems among Malaysian children: a large population-based study. Children (Basel) 2021; 8 (02) 119
- Cela L, Ardenti Morini F, Cortis E. et al. The psychophysical impact of COVID-19 lockdown on pediatric patients with rheumatological disease. Minerva Pediatr (Torino) 2022; (e-pub ahead of print).
- Guido CA, Amedeo I, Avenoso F. et al. Risk factors and mental health promotion strategies in children during COVID-19. Front Public Health 2020; 8: 580720
- Isabel Tan XW, Mordiffi SZ, Lopez V, Leong K. Psychological distress in parents of children with cancer: a descriptive correlational study. Asia Pac J Oncol Nurs 2020; 8 (01) 94-102
- Aziza YDA, Wang ST, Huang MC. Unmet supportive care needs and psychological distress among parents of children with cancer in Indonesia. Psychooncology 2019; 28 (01) 92-98
- Rihm L, Dreier M, Rezvani F, Wiegand-Grefe S, Dirmaier J. The psychosocial situation of families caring for children with rare diseases during the COVID-19 pandemic: results of a cross-sectional online survey. Orphanet J Rare Dis 2022; 17 (01) 449
- Al-Abdulrazzaq D, Khalifa D, Alqaisi T. et al. Health-related quality of life of children and adolescents with type 1 diabetes during the COVID-19 pandemic in Kuwait. Front Public Health 2022; 10: 1056967
-
Kim SJ,
Lee S,
Han H,
Jung J,
Yang SJ,
Shin Y.
Parental mental health and children's behaviors and media usage during COVID-19-related school closures. J Korean Med Sci 2021; 36 (25) e184
Address for correspondence
R. S. Sitorus, PhDDepartment of OphthalmologyFaculty of Medicine, Universitas Indonesia, Jalan Kimia No. 8-10, Jakarta, 10320 IndonesiaEmail: ritasito@yahoo.comPublication History
Article published online:
28 April 2023© 2023. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, IndiaWe recommend- Awareness, Psychological State, and Coping Skills among the Frontline Doctors during the COVID-19 Pandemic—A Cross-Sectional StudyMittal Apurva, Journal of Health and Allied Sciences NU
- Knowledge, Attitude, and Practice Toward Mask-Wearing Behaviors During Covid-19 Pandemic Among Mangalore Residents: A Cross-Sectional StudyNidhish Krishna, Journal of Health and Allied Sciences NU
- Food Insecurity Associated with Evening Types: Cross-sectional Study with University Students during the COVID-19 PandemicG. C. S. Leão, Aktuelle Neurologie, 2023
- Reading fluency during the COVID-19 pandemic: a longitudinal and cross-sectional analysisLuciana Mendonça Alves, VCOT Open, 2022
- Use of Natural Products During the COVID-19 Pandemic: An Exploratory Cross-Sectional Study in Saudi ArabiaO Alghamdi, Planta Medica, 2022
- Tracking Turnover Among Health Care Workers During the COVID-19 Pandemic: A Cross-sectional StudyBianca K. Frogner, JAMA Health Forum, 2022
- Children and Teens Struggling with Mental Health During COVID-19 PandemicJoan Stephenson, JAMA Health Forum, 2021
- Stress perception among dental practitioners in Saudi Arabia during the COVID-19 pandemic: a cross-sectional surveySaquib Ahmed Shaikh, Signa Vitae, 2022
- Mental Well-Being Among Adversity-Exposed Adolescents During the COVID-19 PandemicJulia H. Raney, JAMA Network Open, 2024
- Mental Health Outcomes Among Italian Health Care Workers During the COVID-19 PandemicRodolfo Rossi, JAMA Network Open, 2021
- Awareness, Psychological State, and Coping Skills among the Frontline Doctors during the COVID-19 Pandemic—A Cross-Sectional Study
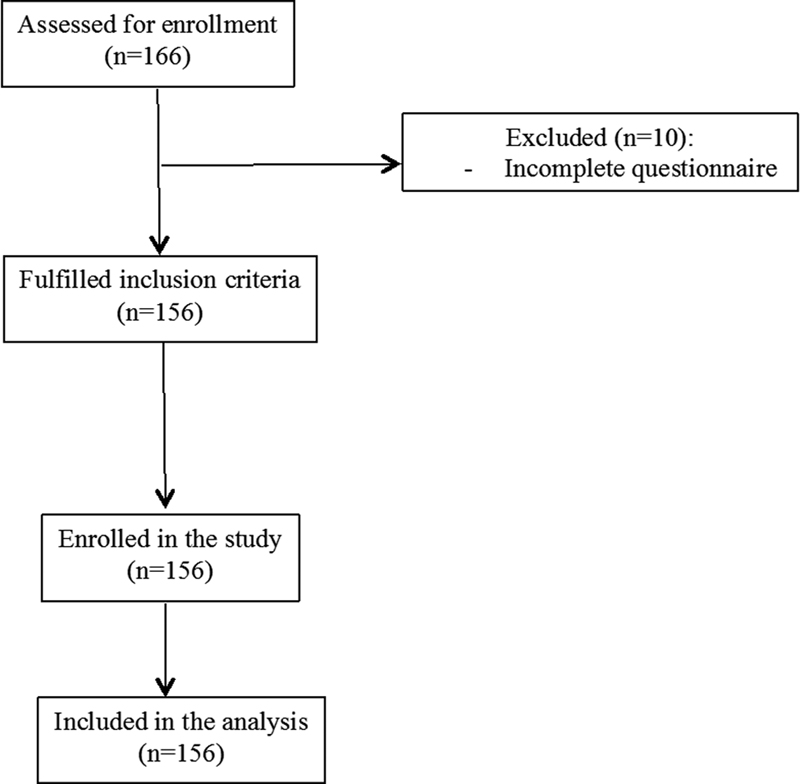
| | Fig 1 Consort diagram showing participants enrollment.|
References
- Amsalem D, Dixon L, Neria Y. The coronavirus disease 2019 (COVID-19) outbreak and mental health: current risks and recommended actions. JAMA Psychiatry 2021; 78 (01) 9-10
- Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr 2020; 174 (09) 819-820
- Jiao WY, Wang LN, Liu J. et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr 2020; 221: 264-266 .e1
- Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health 2021; 30 (01) 1-2
- Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med 2020; 383 (06) 510-512
- Wiguna T, Anindyajati G, Kaligis F. et al. Brief research report on adolescent mental well-being and school closures during the COVID-19 pandemic in Indonesia. Front Psychiatry 2020; 11: 598756
- Garcia de Avila MA, Hamamoto Filho PT, Jacob FLDS. et al. Children's anxiety and factors related to the COVID-19 pandemic: an exploratory study using the children's anxiety questionnaire and the numerical rating scale. Int J Environ Res Public Health 2020; 17 (16) 5757
- Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health 2020; 17 (22) 8479
- Ramaswamy S, Seshadri S. Children on the brink: risks for child protection, sexual abuse, and related mental health problems in the COVID-19 pandemic. Indian J Psychiatry 2020; 62 (9, suppl 3): S404-S413
- Yue J, Zang X, Le Y, An Y. Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID-19) outbreak in China. Curr Psychol 2022; 41 (08) 5723-5730
- Sifat RI, Ruponty MM, Rahim Shuvo MK, Chowdhury M, Suha SM. Impact of COVID-19 pandemic on the mental health of school-going adolescents: insights from Dhaka city, Bangladesh. Heliyon 2022; 8 (04) e09223
- Limone P, Toto GA. Psychological and emotional effects of digital technology on children in COVID-19 pandemic. Brain Sci 2021; 11 (09) 1126
- Rutkowska A, Cieślik B, Tomaszczyk A, Szczepańska-Gieracha J. Mental health conditions among e-learning students during the COVID-19 pandemic. Front Public Health 2022; 10: 871934
- Kishida K, Tsuda M, Waite P, Creswell C, Ishikawa SI. Relationships between local school closures due to the COVID-19 and mental health problems of children, adolescents, and parents in Japan. Psychiatry Res 2021; 306: 114276
- Pandya A, Lodha P. Social connectedness, excessive screen time during COVID-19 and mental health: a review of current evidence. Front Hum Dyn 2021; 3: 684137
- Moreira DC, Millen GC, Sands S, Kearns PR, Hawkins DS. The care of children with cancer during the COVID-19 pandemic. Am Soc Clin Oncol Educ Book 2021; 41: 1-10
- Mirlashari J, Ebrahimpour F, Salisu WJ. War on two fronts: experience of children with cancer and their family during COVID-19 pandemic in Iran. J Pediatr Nurs 2021; 57: 25-31
- Mavrides N, Pao M. Updates in paediatric psycho-oncology. Int Rev Psychiatry 2014; 26 (01) 63-73
- Young AM, Ashbury FD, Schapira L, Scotté F, Ripamonti CI, Olver IN. Uncertainty upon uncertainty: supportive Care for Cancer and COVID-19. Support Care Cancer 2020; 28 (09) 4001-4004
- Mertens A, Gilleland Marchak J. Mental health status of adolescent cancer survivors. Clin Oncol Adolesc Young Adults 2015; 5: 87-95
- Amicucci M, Mastronuzzi A, Ciaralli I. et al. The management of children with cancer during the COVID-19 pandemic: a rapid review. J Clin Med 2020; 9 (11) 3756
- Liu Y, Sundquist J, Sundquist K, Zheng D, Ji J. Mental health outcomes in parents of children with a cancer diagnosis in Sweden: A nationwide cohort study. EClinicalMedicine 2022; 55: 101734
- Garutti M, Cortiula F, Puglisi F. Seven shades of black thoughts: COVID-19 and its psychological consequences on cancer patients. Front Oncol 2020; 10: 1357
- Tsamakis K, Gavriatopoulou M, Schizas D. et al. Oncology during the COVID-19 pandemic: challenges, dilemmas and the psychosocial impact on cancer patients. Oncol Lett 2020; 20 (01) 441-447
- Wang Y, Duan Z, Ma Z. et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl Psychiatry 2020; 10 (01) 263
- Darlington AE, Morgan JE, Wagland R. et al. COVID-19 and children with cancer: parents' experiences, anxieties and support needs. Pediatr Blood Cancer 2021; 68 (02) e28790
- Davies J, O'Connor M, Halkett GKB, Kelada L, Gottardo NG. Parents' experiences of childhood cancer during the COVID-19 pandemic: an Australian perspective. J Pediatr Psychol 2022; 47 (02) 148-157
- Kotecha RS. Challenges posed by COVID-19 to children with cancer. Lancet Oncol 2020; 21 (05) e235
- van Gorp M, Maurice-Stam H, Teunissen LC. et al. No increase in psychosocial stress of Dutch children with cancer and their caregivers during the first months of the COVID-19 pandemic. Pediatr Blood Cancer 2021; 68 (02) e28827
- Scoring the Strengths & Difficulties Questionnaire for 2–4 years old. Development and Well-Being Assessment (DAWBA). October 2015. Accessed March 3, 2021 at: https://sdqinfo.org
- Scoring the Strengths & Difficulties Questionnaire for age 4–17 or 18 + . Development and Well-Being Assessment (DAWBA). June 2016. Accessed March 3, 2021 at: https://sdqinfo.org
- Domingues-Montanari S. Clinical and psychological effects of excessive screen time on children. J Paediatr Child Health 2017; 53 (04) 333-338
- Bekar P, Erkul M, Efe E. Investigation of coronavirus anxiety and caregiving burden among the parents of children with cancer during the COVID-19 outbreak: a descriptive and cross-sectional study. Eur J Cancer Care (Engl) 2022; 31 (04) e13600
- Zijlmans J, Teela L, van Ewijk H. et al. Mental and social health of children and adolescents with pre-existing mental or somatic problems during the COVID-19 pandemic lockdown. Front Psychiatry 2021; 12: 692853
- Li X, Vanderloo LM, Maguire JL. et al; TARGet Kids! Collaboration. Public health preventive measures and child health behaviours during COVID-19: a cohort study. Can J Public Health 2021; 112 (05) 831-842
- Bergmann C, Dimitrova N, Alaslani K. et al. Young children's screen time during the first COVID-19 lockdown in 12 countries. Sci Rep 2022; 12 (01) 2015
- Twenge JM, Farley E. Not all screen time is created equal: associations with mental health vary by activity and gender. Soc Psychiatry Psychiatr Epidemiol 2021; 56 (02) 207-217
- Feng Y, Zhou C, Jia R, Wang Y, Fan X. Quality of life (QoL) and psychosocial outcomes in adult survivors of unilateral retinoblastoma (RB) in China. J Ophthalmol 2020; 2020: 4384251
- van Dijk J, Imhof SM, Moll AC. et al. Quality of life of adult retinoblastoma survivors in the Netherlands. Health Qual Life Outcomes 2007; 5: 30
- Baytan B, Aşut Ç, Çırpan Kantarcıoğlu A, Sezgin Evim M, Güneş AM. Health-related quality of life, depression, anxiety, and self-image in acute lymphocytic leukemia survivors. Turk J Haematol 2016; 33 (04) 326-330
- Hutchinson AD, Pfeiffer SM, Wilson C. Cancer-related cognitive impairment in children. Curr Opin Support Palliat Care 2017; 11 (01) 70-75
- Cheung YT, Sabin ND, Reddick WE. et al. Leukoencephalopathy and long-term neurobehavioural, neurocognitive, and brain imaging outcomes in survivors of childhood acute lymphoblastic leukaemia treated with chemotherapy: a longitudinal analysis. Lancet Haematol 2016; 3 (10) e456-e466
- Bloom J, Lachman A, Gaxo E, Pillay J, Seedat S. Child, adolescent, and caregiver mental health difficulties and associated risk factors early in the COVID-19 pandemic in South Africa. Child Adolesc Psychiatry Ment Health 2022; 16 (01) 65
- Kauhanen L, Wan Mohd Yunus WMA, Lempinen L. et al. A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur Child Adolesc Psychiatry 2023; 32 (06) 995-1013
- Bignardi G, Dalmaijer ES, Anwyl-Irvine AL. et al. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch Dis Child 2020; 106 (08) 791-797
- Sahril N, Ahmad NA, Idris IB, Sooryanarayana R, Abd Razak MA. Factors associated with mental health problems among Malaysian children: a large population-based study. Children (Basel) 2021; 8 (02) 119
- Cela L, Ardenti Morini F, Cortis E. et al. The psychophysical impact of COVID-19 lockdown on pediatric patients with rheumatological disease. Minerva Pediatr (Torino) 2022; (e-pub ahead of print).
- Guido CA, Amedeo I, Avenoso F. et al. Risk factors and mental health promotion strategies in children during COVID-19. Front Public Health 2020; 8: 580720
- Isabel Tan XW, Mordiffi SZ, Lopez V, Leong K. Psychological distress in parents of children with cancer: a descriptive correlational study. Asia Pac J Oncol Nurs 2020; 8 (01) 94-102
- Aziza YDA, Wang ST, Huang MC. Unmet supportive care needs and psychological distress among parents of children with cancer in Indonesia. Psychooncology 2019; 28 (01) 92-98
- Rihm L, Dreier M, Rezvani F, Wiegand-Grefe S, Dirmaier J. The psychosocial situation of families caring for children with rare diseases during the COVID-19 pandemic: results of a cross-sectional online survey. Orphanet J Rare Dis 2022; 17 (01) 449
- Al-Abdulrazzaq D, Khalifa D, Alqaisi T. et al. Health-related quality of life of children and adolescents with type 1 diabetes during the COVID-19 pandemic in Kuwait. Front Public Health 2022; 10: 1056967
- Kim SJ, Lee S, Han H, Jung J, Yang SJ, Shin Y. Parental mental health and children's behaviors and media usage during COVID-19-related school closures. J Korean Med Sci 2021; 36 (25) e184


 PDF
PDF  Views
Views  Share
Share

