Massive Subcutaneous Emphysema and Pneumo-Mediastinum after Percutaneous Lung Biopsy
CC BY 4.0 · Indian J Med Paediatr Oncol 2023; 44(04): 437-439
DOI: DOI: 10.1055/s-0042-1746421
Introduction
Transthoracic percutaneous computed tomography (CT)-guided lung biopsy is an established procedure for obtaining tissue diagnosis in lung masses with diagnostic accuracy up to 98%.[1] Post procedure complications such as pneumothorax and pulmonary hemorrhage, leading to hemoptysis are relatively frequent.[2] Pneumothorax incidence varies from 15% to 54% with subsequent chest drain required in 1.4% to 16.7% of patients.[2] Here, we describe a case of a 69-year-old man who developed mild pneumothorax during CT-guided lung biopsy with bilateral extensive subcutaneous emphysema and pneumomediastinum 48 hours later.
Publication History
Article published online:
28 November 2022
© 2022. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Introduction
Transthoracic percutaneous computed tomography (CT)-guided lung biopsy is an established procedure for obtaining tissue diagnosis in lung masses with diagnostic accuracy up to 98%.[1] Post procedure complications such as pneumothorax and pulmonary hemorrhage, leading to hemoptysis are relatively frequent.[2] Pneumothorax incidence varies from 15% to 54% with subsequent chest drain required in 1.4% to 16.7% of patients.[2] Here, we describe a case of a 69-year-old man who developed mild pneumothorax during CT-guided lung biopsy with bilateral extensive subcutaneous emphysema and pneumomediastinum 48 hours later.
Case Report
A 69-year-old gentleman, a chronic smoker presented with a lung mass for tissue sampling by transthoracic percutaneous CT guided core needle lung biopsy. Routine blood investigations, coagulation profile, and complete blood counts were normal.
After informed consent and procedure counseling about the risks and benefits, the patient was planned for a CT-guided biopsy. During procedure, planning CT, irregular soft tissue density mass lesion was noted in the right lower lobe, limited by an oblique fissure posteriorly. The lesion was approached from the lateral chest wall to avoid the oblique fissure in the prone position. The core needle biopsy was done using an 18G × 10 cm semi-automatic biopsy gun along with its co-axial needle. Mild pneumothorax was noted in the procedural check scan during biopsy without any signs of respiratory distress or dyspnea. Thus, we continued the procedure and successfully performed the CT-guided lung biopsy ([Fig. 1A]). The patient was kept under observation for 4 hours with monitoring of vitals. After 4 hours of observation, a chest radiograph was taken that showed a mild pneumothorax which was stable and mild subcutaneous emphysema at the local site ([Fig. 1B]). The patient was discharged as he was asymptomatic and advised precautionary measures such as bed rest, avoiding heavy exercise and flying. Two days later, the patient presented with subcutaneous swelling and crepitus over the face, neck, and chest regions. He was further evaluated with a thoracic CT scan that showed extensive subcutaneous emphysema extending from the face, neck, and thoracic regions to the upper abdominal wall bilaterally, pneumomediastinum, and persistent right pneumothorax ([Fig. 2C,] [2D]).
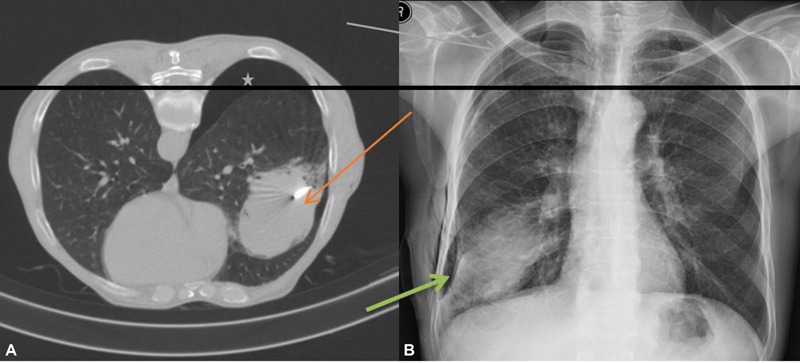
| Figure 1:(Right lung mass lesion was approached in the prone position with coaxial needle in situ (red arrow), mild pneumothorax (asterisk) in the CT scan (B) Mild subcutaneous emphysema at the local site and mild pneumothorax in the apical region in the chest X-ray (green arrow).
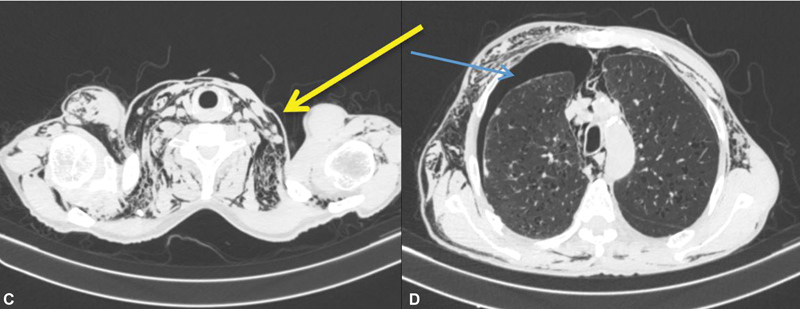
| Figure 2: (C and D) Severe bilateral subcutaneous emphysema in the neck and thorax region with mild pneumothorax, pneumomediastinum in the CT scan (arrows) after 2 days.
In view of no pressure symptoms or respiratory distress/vascular compromise, the patient was managed conservatively with antibiotics and pain medications and requested to follow-up. Further, in due course, the emphysematous changes improved and the patient was started on further treatment as the biopsy revealed non-small cell lung carcinoma (NSCLC) favoring squamous cell carcinoma.
Discussion
Transthoracic percutaneous CT-guided lung biopsy is an established diagnostic tool for getting tissue diagnosis in lung masses with diagnostic accuracy up to 98%[1]. Post-procedure complications such as pneumothorax and hemoptysis are relatively common. Pneumothorax is the most common complication with an incidence of 25% with subsequent chest drain required in 5.6% of patients in a recent meta-analysis of 12,753 lung biopsies.[2] Patient position, small size of the lesion, multiple pleural punctures, and distance of the lesion from the pleura increases the risk of pneumothorax proportionally.[1] [3] [4]
Subcutaneous emphysema (SE) is the leakage of air from the respiratory or gastrointestinal system that diffuses under the skin and myofascial planes.[5] It is found more commonly in association with pneumothorax[6] and is often accompanied by pneumomediastinum.[5] Causes of subcutaneous emphysema in the thoracic region are post-surgery, trauma, infectious, iatrogenic, etc. Post-transthoracic lung biopsy, the incidence of subcutaneous emphysema (SE) is very rare. Very few number of case reports of severe SE have been reported in the literature.[4] [5]
Free air in the subcutaneous thoracic region can be caused due to parietal pleural injury that further diffuses in myofascial planes dissecting them to cause severe subcutaneous emphysema, as discussed in our case. There is a significant correlation between the underlying lung parenchymal condition, which in our case study showed emphysematous changes and the increase in the risk of pneumothorax, and further in subcutaneous emphysema.
Conservative management is the mainstay of treatment of SE; however, it can be individualized depending on the clinical context and severity of symptoms. The increased pressures can cause serious complications, such as upper airway compression and vascular compromise, requiring emergent intervention as necessary. Hence, the patients should be kept under close follow-up.
Conclusion
This case highlights the importance of knowing about this rare but manageable complication and the interventional radiologist should be aware of this.
The appearance can be alarming; however, it typically follows a benign course and patients should be kept under close follow-up.
Conflict of Interest
None declared.
Acknowledgments
We thank the patients and their families for their munificence in contributing to this study. We would also like to thank all members of the IRB committee who gave their approval for this study.
References
- Drumm O, Joyce EA, de Blacam C. et al. CT-guided lung biopsy: effect of biopsy-side down position on pneumothorax and chest tube placement. Radiology 2019; 292 (01) 190-196
- Heerink WJ, de Bock GH, de Jonge GJ, Groen HJ, Vliegenthart R, Oudkerk M. Complication rates of CT-guided transthoracic lung biopsy: meta-analysis. Eur Radiol 2017; 27 (01) 138-148
- Aktas AR, Gozlek E, Yazkan R. et al. Transthoracic biopsy of lung masses: non technical factors affecting complication occurrence. Thorac Cancer 2015; 6 (02) 151-158
- Yuschak E, Michael G, Lanza J, Haq F. Iatrogenic pneumothorax with subsequent subcutaneous emphysema. Cureus 2019; 11 (12) e6480
- Simsek FS, Dag Y. Transthoracic biopsy causes massive subcutaneous emphysema in a low risk patient. J Clin Diagn Res 2016; 10 (11) TD01-TD02
- Melhorn J, Davies HE. The management of subcutaneous emphysema in pneumothorax: a literature review. Curr Pulmonol Rep 2021; 10 (02) 92-97
Address for correspondence
Publication History
Article published online:
28 November 2022
© 2022. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
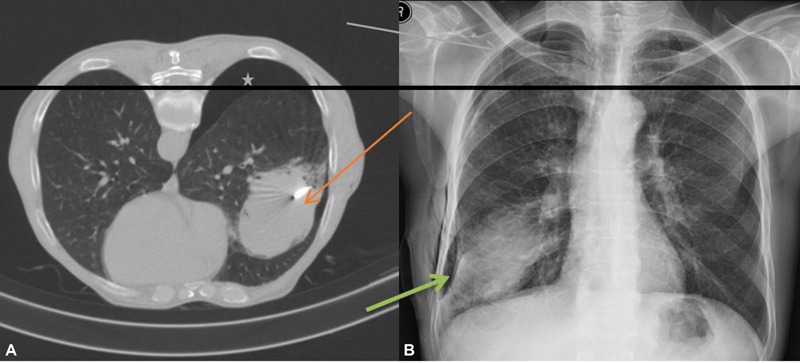
| Figure 1:(Right lung mass lesion was approached in the prone position with coaxial needle in situ (red arrow), mild pneumothorax (asterisk) in the CT scan (B) Mild subcutaneous emphysema at the local site and mild pneumothorax in the apical region in the chest X-ray (green arrow).
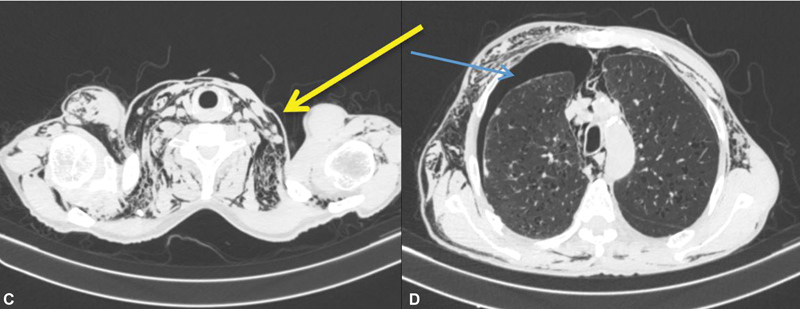
| Figure 2: (C and D) Severe bilateral subcutaneous emphysema in the neck and thorax region with mild pneumothorax, pneumomediastinum in the CT scan (arrows) after 2 days.
References
- Drumm O, Joyce EA, de Blacam C. et al. CT-guided lung biopsy: effect of biopsy-side down position on pneumothorax and chest tube placement. Radiology 2019; 292 (01) 190-196
- Heerink WJ, de Bock GH, de Jonge GJ, Groen HJ, Vliegenthart R, Oudkerk M. Complication rates of CT-guided transthoracic lung biopsy: meta-analysis. Eur Radiol 2017; 27 (01) 138-148
- Aktas AR, Gozlek E, Yazkan R. et al. Transthoracic biopsy of lung masses: non technical factors affecting complication occurrence. Thorac Cancer 2015; 6 (02) 151-158
- Yuschak E, Michael G, Lanza J, Haq F. Iatrogenic pneumothorax with subsequent subcutaneous emphysema. Cureus 2019; 11 (12) e6480
- Simsek FS, Dag Y. Transthoracic biopsy causes massive subcutaneous emphysema in a low risk patient. J Clin Diagn Res 2016; 10 (11) TD01-TD02
- Melhorn J, Davies HE. The management of subcutaneous emphysema in pneumothorax: a literature review. Curr Pulmonol Rep 2021; 10 (02) 92-97


 PDF
PDF  Views
Views  Share
Share

