Malignant Ossifying Fibromyxoid Tumor of the Tongue: A Rare Case
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(03): 415-417
DOI: DOI: 10.4103/ijmpo.ijmpo_201_18
Abstract
Ossifying fibromyxoid tumors (OFMTs) are rare musculoskeletal tumors of uncertain malignant potential. Most OFMTs arise from the subcutaneous tissue, skeletal muscles of extremities, trunk, or head-and-neck region. OFMTs are usually benign, but atypical and malignant OFMT have been described with recurrence and distant metastasis. Till date, the etiopathogenesis and exact line of differentiation of OFMT is still doubtful. We are presenting an unusual case of malignant OFMT of the tongue. It is a rare case of malignant OFMT affecting an unusual site.
Publication History
Received: 12 September 2018
Accepted: 10 November 2019
Article published online:
28 June 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Ossifying fibromyxoid tumors (OFMTs) are rare musculoskeletal tumors of uncertain malignant potential. Most OFMTs arise from the subcutaneous tissue, skeletal muscles of extremities, trunk, or head-and-neck region. OFMTs are usually benign, but atypical and malignant OFMT have been described with recurrence and distant metastasis. Till date, the etiopathogenesis and exact line of differentiation of OFMT is still doubtful. We are presenting an unusual case of malignant OFMT of the tongue. It is a rare case of malignant OFMT affecting an unusual site.
Introduction
Ossifying fibromyxoid tumors (OFMTs) are rare musculoskeletal tumors of uncertain malignant potential, initially reported by Enzinger et al.[1] Most OFMTs arise from the subcutaneous tissue, skeletal muscles of extremities, trunk, or head-and-neck region. OFMTs frequently present in the middle-aged adults as a painless, slow-growing, and well-defined mass.[1] The masses are usually <10 href="https://www.thieme-connect.com/products/ejournals/html/10.4103/ijmpo.ijmpo_201_18#JR_2" xss=removed>2]
We are presenting an unusual case of malignant OFMT of the tongue. It is the second case of malignant OFMT tongue, to the best of our knowledge, the first case of malignant OFMT of the tongue was described by Ohta et al. in 2013.[3]
Case Report
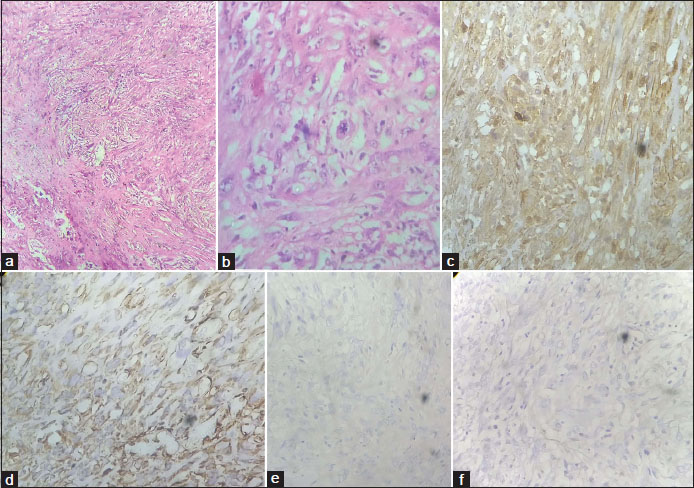
A 35-year-old female presented with a painless firm mass at the right lateral border of the tongue for 1½ months, rapidly increasing in size up to 3 cm. The mass was biopsied thrice with inconclusive reports from different centers. Finally, wide local excision was performed and sent for histopathological examination in our department. Grossly, the tumor was circumscribed gray-brown soft-tissue piece measuring 3 cm × 2.5 cm × 1 cm. Cut section was solid and gray white in color [Figure 1]. Microscopic examination showed the presence of central areas of osteoid and woven bone with spindle cell tumor arranged in loose and compact fascicles having round-oval nucleus showing moderate nuclear pleomorphism with prominent nucleolus and atypical mitoses and many giant cells. On performing immunohistochemical (IHC) analysis, the tumor cells showed diffuse positivity for vimentin and S100 and negative for cytokeratin and P63 [Figure 2]. A final diagnosis of malignant OFMT (high grade with 5 mitoses/10 HPF) was made.

| Figure 1:Gross examination: On cut section of the resected mass, encapsulated gray-brown mass from lateral border of the tongue
| Figure.2:(a) H and E sections, Low power (×10) showing spindle-to-oval cells with indistinct cytoplasm arranged in fascicles and fibromyxoid matrix. Note osteoid formation on lower left end. (b) Atypical mitosis with nuclear pleomorphism seen on high-power view (×40). Immunohistochemical markers: (c) S100 (C + N) and (d) Vimentin (C) positivity, (e) cytokeratin (C) and (f) P63(N) negativity
Discussion
Malignant OFMT of the tongue is an unusual site for a rare tumor. In 1989, a series of 59 cases from the Armed Forces Institute of Pathology revealed the benign nature of majority of cases. However, few cases may recur locally and metastasize.[1]
Folpe and Weiss found that recurrence and metastatic rate of OFMTs were 17% and 5%, respectively, and they considered these lesions to be of borderline malignancy.[2] In their study of 70 cases of OFMTs, 29% of cases showed typical features and 64% of cases showed mixed features of typical and atypical. The tumors occurred as subcutaneous or deeply seated masses in the trunk and proximal extremities. After the analysis, they concluded that tumors with a high nuclear grade, increased cellularity and mitotic count >2/50 HPF should be regarded as sarcoma with a significant potential for metastasis, but after follow-up, six of ten cases had metastatic disease, described later as atypical OFMTs. They had atypical histological features including high nuclear grade, increased cellularity, and increased mitotic activity. The present case also has an increased cellularity, moderate nuclear atypia, and increased mitotic activity with morphological features of OFMTs. The patient had a history of recurrence at the lateral border of the tongue, which is a very unusual site of OFMTs.
Williams et al. reported that one of nine head-and-neck OFMTs have malignant behavior.[4] In 1995, Kilpatrick et al. reported 6 atypical/malignant OFMTs. On follow-up, some cases developed recurrence and few presented with distant metastasis.[5] Graham et al. also suggested the term “malignant OFMT” using IHC and gene expression profiling.[6]
Ohta et al. reported the recurrence of malignant OFMT of the tongue. Recurrent tumor was composed of closely packed cells positive for vimentin and S-100 proliferating in a nodular fashion; tumor cells were arranged in a diffuse or cord-like manner with high cellularity and mitotic activity within an abundant fibromyxoid matrix, along with a small amount of metaplastic ossification, corresponding to the histopathological characteristic of OFMT. The present case also has similar morphological and IHC findings.[3]
The line of differentiation of OFMT is still in doubt. Some literature suggested a Schwannian or neuronal differentiation.[7] While Enzinger et al. proposed its cartilaginous or myoepithelial differentiation. Recently, according to Gebre-Medhin et al., the arrangement of PHF1 gene in these tumors suggests that OFMTs are translocation associated showing scrambled phenotype which is originally hypothesized by Folpe and Weiss in 2003.[8]
A variety of lesions were considered in the differential diagnosis, including sarcomatoid carcinoma, epithelioid smooth muscle tumors, epithelioid nerve sheath tumors, myoepithelioma/myoepithelial carcinoma, and ectomesenchymal chondromyxoid tumors of the tongue. Because of their overlapping IHC markers expression, they were excluded on the basis of clinical, radiological, and histological findings. Peripheral bone formation is a pathognomonic feature of OFMT, aneurysmal bone cyst of the soft tissue, and myositis ossificans. The above-mentioned differential diagnosis does not have peripheral bone formation and they have ossification within the tumor. A final diagnosis of malignant OFMT is made. Because of the possibility of recurrence, understanding OFMT in the tongue with exclusion of other differential diagnoses is essential for proper and prompt management.
Conflict of Interest
There are no conflicts of interest.
References
- Enzinger FM, Weiss SW, Liang CY. Ossifying fibromyxoid tumor of soft parts. A clinicopathological analysis of 59 cases. Am J Surg Pathol 1989; 13: 817-27
- Folpe AL, Weiss SW. Ossifying fibromyxoid tumor of soft parts: A clinicopathologic study of 70 cases with emphasis on atypical and malignant variants. Am J Surg Pathol 2003; 27: 421-31
- Ohta K, Taki M, Ogawa I, Ono S, Mizuta K, Fujimoto S. et al. Malignant ossifying fibromyxoid tumor of the tongue: Case report and review of the literature. Head Face Med 2013; 9: 16
- Williams RW, Case CP, Irvine GH. Ossifying fibromyxoid tumour of soft parts--a new tumour of the parotid/zygomatic arch region. Br J Oral Maxillofac Surg 1994; 32: 174-7
- Kilpatrick SE, Ward WG, Mozes M, Miettinen M, Fukunaga M, Fletcher CD. Atypical and malignant variants of ossifying fibromyxoid tumor. Clinicopathologic analysis of six cases. Am J Surg Pathol 1995; 19: 1039-46
- Graham RP, Dry S, Li X, Binder S, Bahrami A, Raimondi SC. et al. Ossifying fibromyxoid tumor of soft parts: A clinicopathologic, proteomic, and genomic study. Am J Surg Pathol 2011; 35: 1615-25
- Donner LR. Ossifying fibromyxoid tumor of soft parts: Evidence supporting Schwann cell origin. Hum Pathol 1992; 23: 200-2
- Gebre-Medhin S, Nord KH, Möller E, Mandahl N, Magnusson L, Nilsson J. et al. Recurrent rearrangement of the PHF1 gene in ossifying fibromyxoid tumors. Am J Pathol 2012; 181: 1069-77
Address for correspondence
Publication History
Received: 12 September 2018
Accepted: 10 November 2019
Article published
online:
28 June 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301
UP, India

| Figure 1:Gross examination: On cut section of the resected mass, encapsulated gray-brown mass from lateral border of the tongue
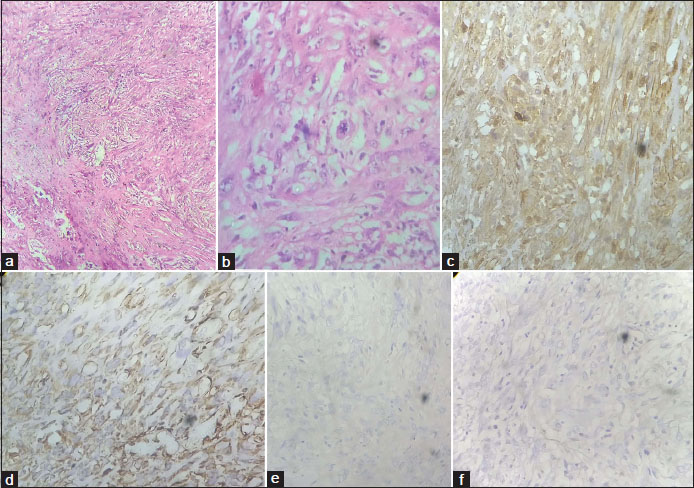
| Figure.2:(a) H and E sections, Low power (×10) showing spindle-to-oval cells with indistinct cytoplasm arranged in fascicles and fibromyxoid matrix. Note osteoid formation on lower left end. (b) Atypical mitosis with nuclear pleomorphism seen on high-power view (×40). Immunohistochemical markers: (c) S100 (C + N) and (d) Vimentin (C) positivity, (e) cytokeratin (C) and (f) P63(N) negativity
References
- Enzinger FM, Weiss SW, Liang CY. Ossifying fibromyxoid tumor of soft parts. A clinicopathological analysis of 59 cases. Am J Surg Pathol 1989; 13: 817-27
- Folpe AL, Weiss SW. Ossifying fibromyxoid tumor of soft parts: A clinicopathologic study of 70 cases with emphasis on atypical and malignant variants. Am J Surg Pathol 2003; 27: 421-31
- Ohta K, Taki M, Ogawa I, Ono S, Mizuta K, Fujimoto S. et al. Malignant ossifying fibromyxoid tumor of the tongue: Case report and review of the literature. Head Face Med 2013; 9: 16
- Williams RW, Case CP, Irvine GH. Ossifying fibromyxoid tumour of soft parts--a new tumour of the parotid/zygomatic arch region. Br J Oral Maxillofac Surg 1994; 32: 174-7
- Kilpatrick SE, Ward WG, Mozes M, Miettinen M, Fukunaga M, Fletcher CD. Atypical and malignant variants of ossifying fibromyxoid tumor. Clinicopathologic analysis of six cases. Am J Surg Pathol 1995; 19: 1039-46
- Graham RP, Dry S, Li X, Binder S, Bahrami A, Raimondi SC. et al. Ossifying fibromyxoid tumor of soft parts: A clinicopathologic, proteomic, and genomic study. Am J Surg Pathol 2011; 35: 1615-25
- Donner LR. Ossifying fibromyxoid tumor of soft parts: Evidence supporting Schwann cell origin. Hum Pathol 1992; 23: 200-2
- Gebre-Medhin S, Nord KH, Möller E, Mandahl N, Magnusson L, Nilsson J. et al. Recurrent rearrangement of the PHF1 gene in ossifying fibromyxoid tumors. Am J Pathol 2012; 181: 1069-77


 PDF
PDF  Views
Views  Share
Share

