Malignant ectomesenchymoma of the nasal cavity
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2011; 32(04): 242-243
DOI: DOI: 10.4103/0971-5851.95164
Abstract
Malignant ectomesenchymomas are rare tumors. This tumor affects predominantly young children. Most common site is head and neck. A multi modality approach should be appropriate for this soft-tissue tumor. We present a 43 year old female with malignant ectomesenchymoma of the nasal cavity.
Publication History
Article published online:
06 August 2021
© 2011. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Malignant ectomesenchymomas are rare tumors. This tumor affects predominantly young children. Most common site is head and neck. A multi modality approach should be appropriate for this soft-tissue tumor. We present a 43 year old female with malignant ectomesenchymoma of the nasal cavity.
INTRODUCTION
Malignant ectomesenchymoma is a rare tumor reported in the head and neck, abdomen, and perineal regions.[1] It consists of mesenchymal and neuroectodermal elements. In this tumor group, the neoplastic cells are differentiated into neuronal cells. It also has at least one malignant mesenchymal element, generally rhabdomyosarcoma. In this report we present a 43-year-old female, with malignant ectomesenchymoma of the nasal cavity.
CASE REPORT
A 43-year-old female presented with a history of epistaxis and left-sided nasal block of a one-month duration. Examination revealed a fleshy growth in the left nasal cavity and a left level II cervical lymph node enlargement. Computerized tomography (CT) scan of the local part revealed a large mass in the left nasal cavity, extending to the left maxillary antrum and ethmoidal sinus [Figure 1]. The left medial wall of the maxillary antrum and inferior orbital plate was breached by the tumor.
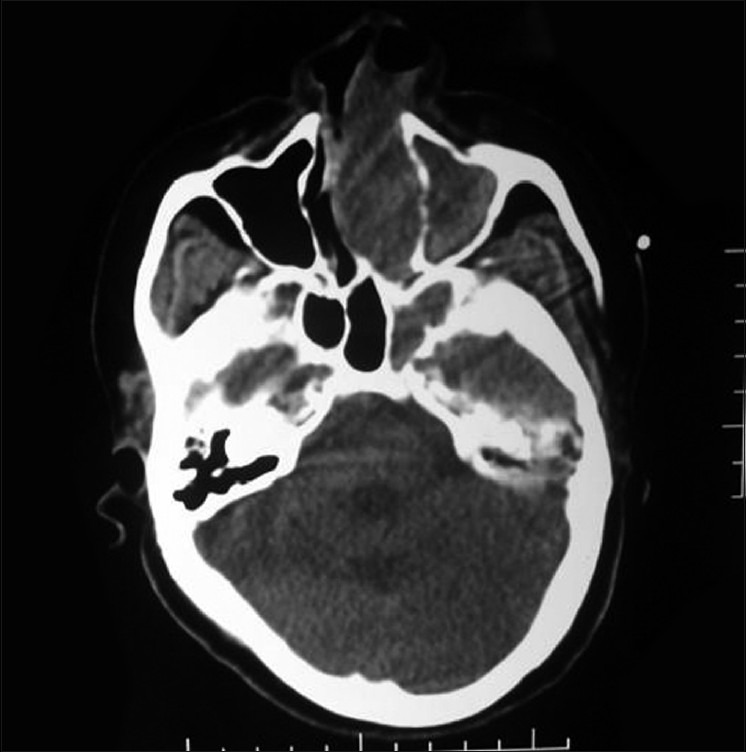
| Figure 1:Computerized tomography scan of the local part revealed a large mass in the left nasal cavity, extending to the left maxillary antrum and the ethmoidal sinus
A biopsy revealed that the tumor tissue was lined by respiratory epithelium. The cells were arranged in sheets and alveolar masses and were composed of round-to-oval cells of moderate size with a moderate amount of cytoplasm. The nuclei were round-to-oval and hyperchromatic. Mitoses varied from one to two/high power field. Moderate cellular and nuclear pleomorphism was seen. Few elongated cells were also seen among the rounded cells.
Immunohistochemistry showed a strong, positive reaction for muscle-specific actin, desmin, CD99, and the neuron-specific enolase. Areas showed positivity for synaptophysin, neurofilament, and S-100p, suggestive of neural differentiation. Some of them showed a faint positive reaction for the epithelial membrane antigen and pankeratin. Strap muscle cells and ganglion cells were not recognized. A diagnosis of ectomesenchymoma was made, showing mainly rhabdomyoblastoma- and neuroblastoma-like areas.
CT of the chest and bone marrow biopsy were normal. The bone scan showed uptake in the left nasal bone and the left maxillary antrum. The patient was staged as the International Rhabdomyosarcoma Group (IRSG) Stage III Group III.[2] The patient has completed 50.5 Gy radiotherapy to the local part and has completed combination chemotherapy as per the IRS IV protocol. Primary surgery was not possible as the tumor was very extensive and it would be a mutilating surgery.
DISCUSSION
Malignant ectomesenchymomas are rare tumors composed of neuroblasts and/or ganglion cells and malignant mesenchymal tissue(s) of various types, usually rhabdomyosarcoma.[3] A review of the Literature of 44 reported cases of ectomesenchymoma has shown that this tumor affects predominantly young children: 81.6% were children under 13 years of age and 18.4% were adults. The male-to-female ratio was 20 : 14 (58.8 and 41.2%). Head and neck was the most common site (30.5%), followed by the scrotum (16.7%), the abdomen (13.9%), the retroperitoneal space (11.1%), the pelvis (5.6%), the perineum (2.8%), and the prostate (one case 2.8%).[4]
The first reported case of nasal ectomesenchymoma was in a 62-year-old man who was treated with surgery and adjuvant radiotherapy, and had no recurrence of disease after six months.[5] The best therapeutic approach for ectomesenchymoma seems to be the association of surgery, radiotherapy, and chemotherapy; however, the best standard therapeutic protocol is currently a matter of discussion.[5] As the most common malignant component of ectomesenchymomas is generally represented by a rhabdomyosarcoma, a chemotherapeutic protocol, and a multimodal approach suitable for this soft-tissue tumor should be appropriate. However, because of its rarity, the different sites where it can arise, and the difference in the age of patients who present with this tumor, there is no definitive agreement for treatment. Different therapeutic approaches have been reported in published studies, especially for cases affecting adults.[6–8] Our patient has completed radiotherapy and 42 weeks of chemotherapy and is in remission.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- Govender D, Hadley GP. Ectomesenchymoma of the prostate: Histological diagnostic criteria. Pediatr Surg Int 1999;15:68-70.
- Crist W, Gehan EA, Ragab AH, Dickman PS, Donaldson SS, Fryer C, et al. The Third Intergroup Rhabdomyosarcoma Study. J Clin Oncol 1995;13:610-30.
- Kawamoto EH, Weidner N, Agostini RM Jr, Jaffe R. Malignant ectomesenchymoma of soft tissue. Report of two cases and review of the literature. Cancer 1987;59:1791-802.
- Kösem M, Ibiloðlu I, Bakan V, Köseoðlu B. Ectomesenchymoma: Case report and review of the literature. Turk J Pediatr 2004;46:82-7.
- Brehmer D, Overhoff HM, Marx A. Malignant ectomesenchymoma of the nose. Case report and review of the literature. ORL J Otorhinolaryngol Relat Spec 2003;65:52-6.
- Shuanghoti S, Kasanthikul V, Suwangool P, Chittmittrapap S. Malignant neoplasm of mixed mesenchymal and neuroepithelial origin (ectomesenchymoma) of thigh. J Surg Oncol 1984;27:208-13.
- Mouton SC, Rosenberg HS, Cohen MC, Drut R, Emms M, Kaschula RO. Malignant ectomesenchymoma in childhood. Pediatr Pathol Lab Med 1996;16:607-24.
- Freitas AB, Aguiar PH, Miura FK, Yasuda A, Soglia J, Soglia F, et al. Malignant ectomesenchymoma. Case report and review of literature. Pediatr Neurosurg 1999;30:320-30.
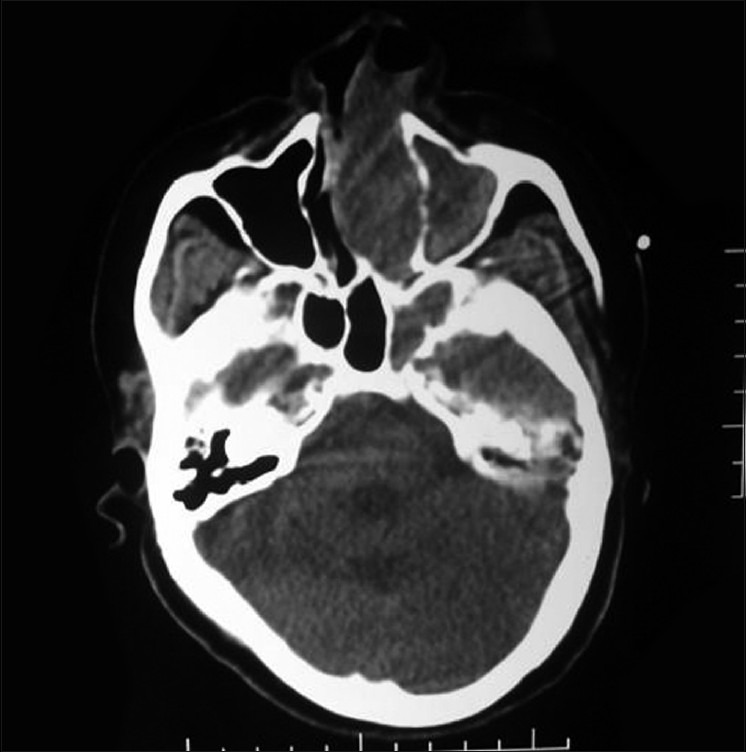
| Figure 1:Computerized tomography scan of the local part revealed a large mass in the left nasal cavity, extending to the left maxillary antrum and the ethmoidal sinus
References
- Govender D, Hadley GP. Ectomesenchymoma of the prostate: Histological diagnostic criteria. Pediatr Surg Int 1999;15:68-70.
- Crist W, Gehan EA, Ragab AH, Dickman PS, Donaldson SS, Fryer C, et al. The Third Intergroup Rhabdomyosarcoma Study. J Clin Oncol 1995;13:610-30.
- Kawamoto EH, Weidner N, Agostini RM Jr, Jaffe R. Malignant ectomesenchymoma of soft tissue. Report of two cases and review of the literature. Cancer 1987;59:1791-802.
- Kösem M, Ibiloðlu I, Bakan V, Köseoðlu B. Ectomesenchymoma: Case report and review of the literature. Turk J Pediatr 2004;46:82-7.
- Brehmer D, Overhoff HM, Marx A. Malignant ectomesenchymoma of the nose. Case report and review of the literature. ORL J Otorhinolaryngol Relat Spec 2003;65:52-6.
- Shuanghoti S, Kasanthikul V, Suwangool P, Chittmittrapap S. Malignant neoplasm of mixed mesenchymal and neuroepithelial origin (ectomesenchymoma) of thigh. J Surg Oncol 1984;27:208-13.
- Mouton SC, Rosenberg HS, Cohen MC, Drut R, Emms M, Kaschula RO. Malignant ectomesenchymoma in childhood. Pediatr Pathol Lab Med 1996;16:607-24.
- Freitas AB, Aguiar PH, Miura FK, Yasuda A, Soglia J, Soglia F, et al. Malignant ectomesenchymoma. Case report and review of literature. Pediatr Neurosurg 1999;30:320-30.


 PDF
PDF  Views
Views  Share
Share

