Macrodystrophia Lipomatosa: Clinico patho radiological Correlation
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(04): 559-562
DOI: DOI: 10.4103/ijmpo.ijmpo_65_16
Abstract
Macrodystrophia lipomatosa is a rare congenital nonhereditary developmental anomaly. It is characterized by hamartomatous proliferation of the soft tissue leading to disproportionate enlargement of the limbs and digits. Since it leads to diagnostic dilemma, it has to be differentiated from various other conditions as they differ in course, prognosis,complications, and treatment. Herein, we present two cases with localized gigantism and discuss the various differential diagnoses and need for clinico-patho-radilogical correlation for diagnosis of this rare entity.
Publication History
Article published online:
04 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used forcommercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Macrodystrophia lipomatosa is a rare congenital nonhereditary developmental anomaly. It is characterized by hamartomatous proliferation of the soft tissue leading to disproportionate enlargement of the limbs and digits. Since it leads to diagnostic dilemma, it has to be differentiated from various other conditions as they differ in course, prognosis, complications, and treatment. Herein, we present two cases with localized gigantism and discuss the various differential diagnoses and need for clinico-patho-radilogical correlation for diagnosis of this rare entity.
Introduction
Macrodystrophia lipomatosa (ML) is a rare form of nonhereditary congenital macrodactyly characterized by progressive overgrowth of mesenchymal elements with a disproportionate increase in the amount of fibroadipose tissue. This abnormality occurs most frequently along the median nerve distribution in the upper extremities and the plantar nerve in the lower extremities.[1,2,3] Usually, one or more digits of the unilateral limb are affected. There is no gender predilection; however, males are more affected than females.[1] Due to rarity, the incidence is unknown. Earlier, a variety of descriptive terms were used for this condition, especially in the pediatric age group such as macrodactyly, megalodactyly, digital gigantism, macromelia, partial acromegaly, macrosomy, and limited gigantism. ML leads to diagnostic dilemma and has to be differentiated from various other conditions as they differ in course, prognosis, complications, and treatment. The patient outcome is dependent on the severity of the disease. In the present cases, cytology in conjunction with radio imaging aided in reaching the diagnosis, followed by subsequent corrective surgical management.
Case Reports
Case 1
A 3-year-old female child presented with a progressive disproportionate enlargement of the second and third toes of the right foot since birth [Figure 1]. There were no history of any pain or neurovascular symptoms and also no family history of extremity gigantism. The developmental milestones were according to the age. On physical examination, there was nontender enlargement of the second and third toes of the right foot. No overlying cutaneous changes, pitting edema, or bruit was seen. All the other extremities were found to be normal on examination. A plain X-ray of the right foot was performed that revealed soft-tissue swelling involving the second and third toes with hypertrophy of the phalanges [Figure 2]. Gray-scale ultrasound and color flow Doppler revealed diffuse soft-tissue thickening, without any abnormal calcifications or abnormal blood flow. Fine-needle aspiration from the second digit yielded blood-tinged fatty aspirate. Smears examined revealed fragments of mature adipose tissue [Figure 3]. No malignant cells were identified. The background revealed fat droplets admixed with red blood cells (RBCs) and few inflammatory cells. Correlating the lesion's clinical presentation, imaging and cytological finding possibility of benign mesenchymal lesion of lipomatous origin was considered with a differential diagnosis of ML and fibrolipomatous hamartoma. Debulking surgery was performed. Histopathological examination of the sent material showed mature fibroadipose tissue involving the subcutaneous plane. The nerve sheath and the surrounding muscle fibers were free of fatty infiltration. Thus, a definitive diagnosis of ML was rendered which confirmed the initial cytological possibilities.

| Figure 1:Clinical image showing enlargement of the second and third toes of the right foot

| Figure 2:X-ray image showing hypertrophy of soft tissues of the 2nd and 3rd digit of the right foot
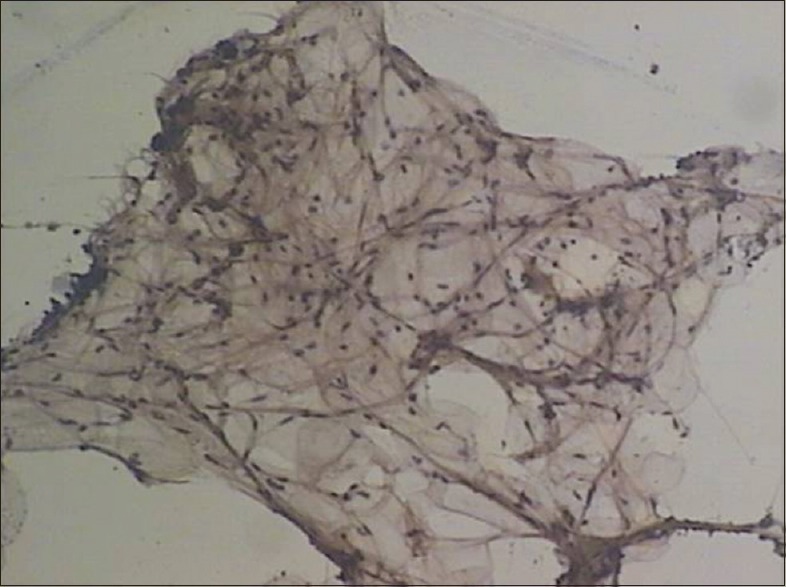
| Figure 3:Cytosmears reveal mature adipocytes (Pap, ×100)
Case 2
A 21-year-old right hand dominated female presented with a progressive disproportionate enlargement of distal arm and digits of the right hand since birth. The patient denied having any pain or neurovascular symptoms, and there was no family history of extremity gigantism. Twelve years back, she had a history of amputation of index and middle fingers at some periphery hospital. However, no records of the same were available. On physical examination, a nontender, soft-tissue mass was palpable on the volar aspect of the enlarged thumb with disfigurement of digits and distal arm [Figure 4]. There were no overlying cutaneous changes, pitting edema, or bruit. A plain radiograph demonstrated soft-tissue swelling along the volar aspect of the thumb, enlarged phalanges of the digits [Figure 5]. Gray-scale ultrasound and color flow Doppler revealed diffuse soft-tissue thickening, without any abnormal calcifications or abnormal blood flow. Fine-needle aspiration from the disproportionate areas yielded blood-tinged fatty aspirate. Smears examined revealed fragments of mature adipose tissue. No malignant cells were identified. No other spindle cell component was identified. The background revealed fat droplets admixed with RBCs and few inflammatory cells. Correlating the lesion's clinical presentation, imaging and cytological finding possibility ML was considered. The multidisciplinary team decided to perform a debulking surgery. On gross examination a yellowish soft-tissue mass was received which on cut section was fibrofatty. No firm areas or hemorrhage or necrosis was identified. Microscopic examination revealed mature fibroadipose tissue involving the subcutaneous plane [Figure 6]. The nerve sheath and the surrounding muscle fibers were free of fatty infiltration. Thus, a definitive diagnosis of ML was rendered which confirmed the initial possibility.

| Figure 4:Clinical image showing soft-tissue mass of the enlarged limb with disfigurement of digits and distal arm of the right upper limb
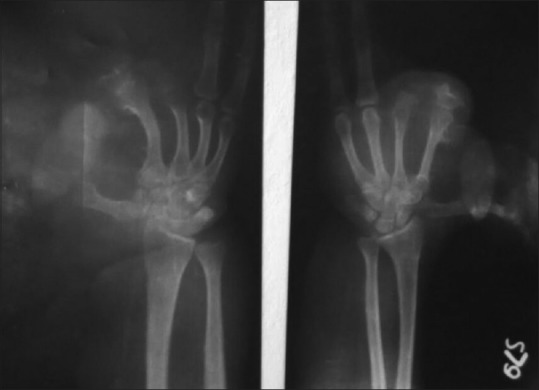
| Figure 5:X-ray image showing bulbous enlargement of the thumb of the right hand
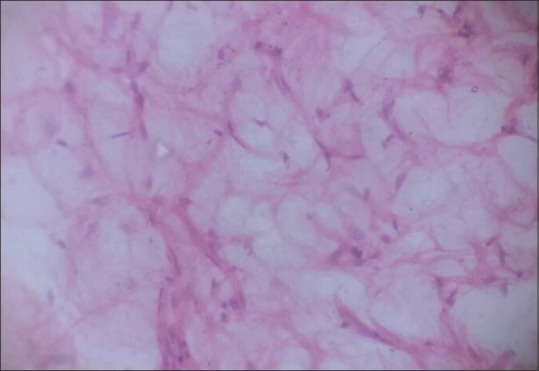
| Figure 6:Section shows abundant adipose tissue (H and E, ×400)
Discussion
ML is an uncommon congenital, nonhereditary developmental anomaly generally presenting hamartomatous proliferation of the soft tissue of the affected area also called as localized gigantism.[1] This disease is characterized by the proliferation of all the mesenchymal elements of a digit or digits and a disproportionate increase of fibroadipose tissue, involving the nerve sheath, muscle, periosteum, and bone marrow.[2,3]
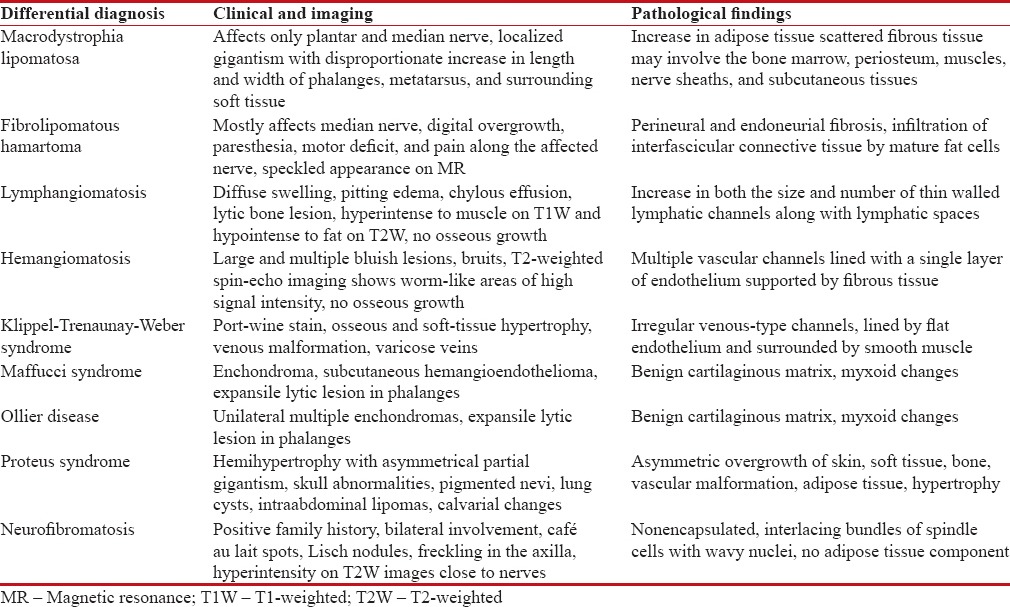
Feriz[4] in 1925 first used the term ML. Barsky[5] divided ML into two types, including the static and progressive forms. In the static form, the growth rate of affected tissues is normal. In the progressive form, the growth rate of mesenchymal tissues is faster when compared with normal tissues and ceases its abnormal growth at puberty. Progressive macrodactyly is more common than static type. Exact etiology is unknown, but various hypotheses have been proposed regarding the etiopathogenesis of ML. These include lipomatous degeneration, fetal circulation abnormality, and damage of extremity bud and alteration of somatic cells in intrauterine life and hypertrophy of the concerned nerve.[6] It may be associated with various abnormalities such as syndactyly, polydactyly, brachydactyly, or clinodactyly. The various differential diagnoses are discussed in Table 1.[1,2,7,8,9,10]
Table 1
Differential diagnosis of macrodactyly
|
The problems associated with a patient of ML can be cosmetic or mechanical. The overgrowth may lead to interference in normal day-to-day activities or make patient prone to repeated injury. Mechanical problems may develop such as secondary osteoarthritis and compression of neurovascular structures causing impairment of function. Cosmetic problem is usual, presenting complaint in all ages, but mechanical problems are encountered in adolescence due to secondary degenerative joint changes causing reduced function. Electroneurography and nerve conduction velocity tests performed in these patients may reveal slowed distal motor and sensory conduction, segmental conduction block, or slowing of the peripheral nerves at the entrapment sites.
Different imaging modalities such as X-ray, ultrasonography, computed tomography (CT) scan, and magnetic resonance imaging (MRI) have a role in the evaluation of ML. Typical X-ray findings of ML include hypertrophy of soft tissue as well as osseous tissue, with translucencies in the soft tissue due to increased adipose tissue. The phalanges are elongated, broad, and splayed, sometimes giving rise to a mushroom-like appearance. Secondary osteoarthritic changes such as joint space narrowing, subchondral cysts, and osteophytes may also be seen. Excessive growth of the bone within the area innervated by nerve and fat tissue proliferation within muscle fibers are the characteristic findings detected on CT scan. MRI scans reveal the presence of abundant adipose tissue, which exhibits the same signal intensity as normal subcutaneous fat in the areas affected by the disease. There may be linear hypointense fibrous bands noted within this abnormal fat on T1-weighted imaging. There are osseous hypertrophy and cortical thickening in the affected part of the body, and this may lead to exostoses such as bony outgrowths from the involved bone.[8,9,10]
The treatment is usually surgical, which is carried out due to cosmetic reasons, but since the digital enlargement stops at puberty, management should include an attempt to preserve neurological functions. For lesion involving median and plantar region, conservative approach has been advocated. Multiple debulking procedures, epiphysiodesis, and various osteotomies are indicated for more severe form of the disease. Reconstructive surgery, which achieves a more functional result, should be preferred strategy.[7]
ML is progressive hamartomatous enlargement of the fibrofatty tissue involving all the layers of soft tissue and even bone more commonly leading to cosmetic and mechanical problems. Diagnosis is accomplished on the basis of clinical and radiological evaluation which can be confirmed on histopathological examination. Awareness of the characteristic symptoms, imaging, pathology, and differential diagnosis of the disease is very important for the treatment of the rare entity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Mannan R, Bhasin TS, Kaur p, Kaur H, Singh K. Cytoradiological diagnosis of Macrodystrophia lipomatosa: A report of rare entity with review of literature. Int J Med Health Sci 2013;2:469-71.
- Singla V, Virmani V, Tuli P, Singh P, Khandelwal N. Case report: Macrodystrophia lipomatosa – Illustration of two cases. Indian J Radiol Imaging 2008;18:298-301.
- Choudhary S, Ray S, Prabhakaran N. Macrodystrophia lipomatosa: A case report with review of literature. J Evol Med Dent Sci 2013;2:5216-22.
- Feriz H. Makrodystrophia lipomatosa progressiva. Virchows Arch 1925;260:308-68.
- Barsky AJ. Macrodactyly. J Bone Joint Surg Am 1967;49:1255-66.
- Ly JQ, Beall DP. Quiz case. Macrodystrophia lipomatosa. Eur J Radiol 2003;47:16-8.
- Watt AJ, Chung KC. Macrodystrophia lipomatosa: A reconstructive approach to gigantism of the foot. J Foot Ankle Surg 2004;43:51-5.
- Celebi F, Karagulle K, Oner AY. Macrodystrophia lipomatosa of foot: A case report. Oncol Lett 2015;10:951-3.
- Prasetyono TO, Hanafi E, Astriana W. A review of Macrodystrophia lipomatosa: Revisitation. Arch Plast Surg 2015;42:391-406.
- Upadhyay D, Parashari UC, Khanduri S, Bhadury S. Macrodystrophia lipomatosa: Radiologic-pathologic correlation. J Clin Imaging Sci 2011;1:18.

| Figure 1:Clinical image showing enlargement of the second and third toes of the right foot

| Figure 2:X-ray image showing hypertrophy of soft tissues of the 2nd and 3rd digit of the right foot
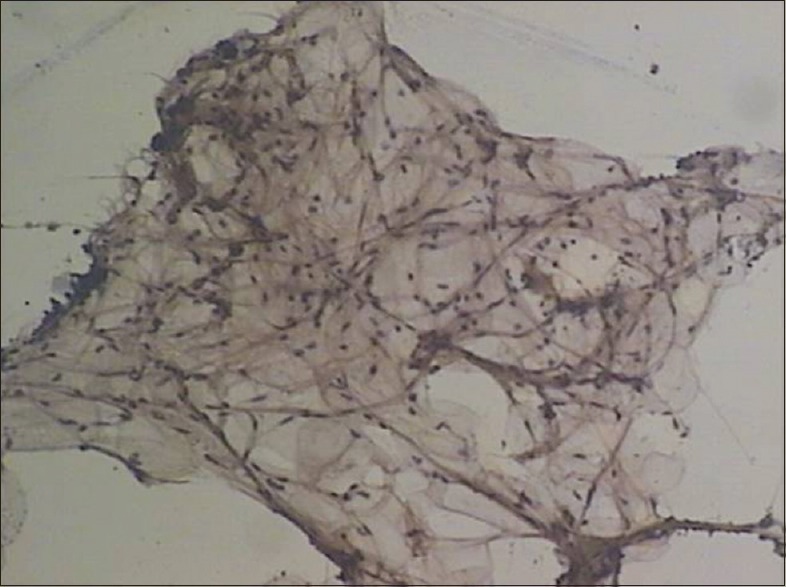
| Figure 3:Cytosmears reveal mature adipocytes (Pap, ×100)

| Figure 4:Clinical image showing soft-tissue mass of the enlarged limb with disfigurement of digits and distal arm of the right upper limb
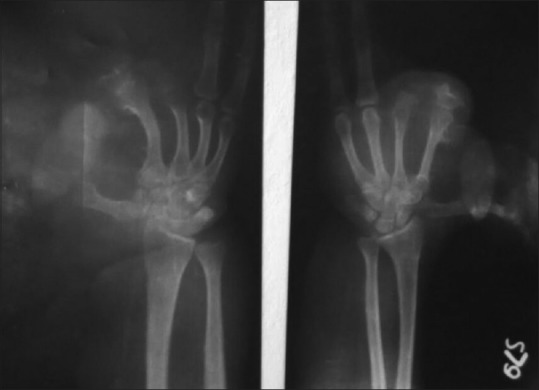
| Figure 5:X-ray image showing bulbous enlargement of the thumb of the right hand
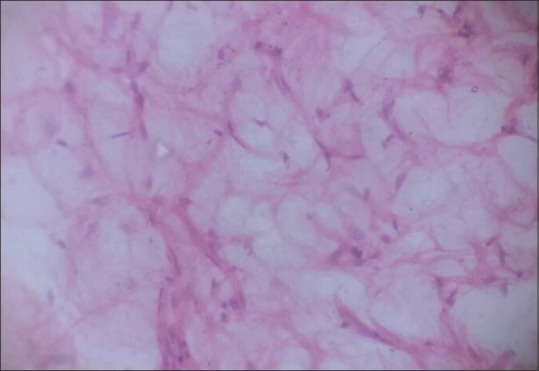
| Figure 6:Section shows abundant adipose tissue (H and E, ×400)
References
- Mannan R, Bhasin TS, Kaur p, Kaur H, Singh K. Cytoradiological diagnosis of Macrodystrophia lipomatosa: A report of rare entity with review of literature. Int J Med Health Sci 2013;2:469-71.
- Singla V, Virmani V, Tuli P, Singh P, Khandelwal N. Case report: Macrodystrophia lipomatosa – Illustration of two cases. Indian J Radiol Imaging 2008;18:298-301.
- Choudhary S, Ray S, Prabhakaran N. Macrodystrophia lipomatosa: A case report with review of literature. J Evol Med Dent Sci 2013;2:5216-22.
- Feriz H. Makrodystrophia lipomatosa progressiva. Virchows Arch 1925;260:308-68.
- Barsky AJ. Macrodactyly. J Bone Joint Surg Am 1967;49:1255-66.
- Ly JQ, Beall DP. Quiz case. Macrodystrophia lipomatosa. Eur J Radiol 2003;47:16-8.
- Watt AJ, Chung KC. Macrodystrophia lipomatosa: A reconstructive approach to gigantism of the foot. J Foot Ankle Surg 2004;43:51-5.
- Celebi F, Karagulle K, Oner AY. Macrodystrophia lipomatosa of foot: A case report. Oncol Lett 2015;10:951-3.
- Prasetyono TO, Hanafi E, Astriana W. A review of Macrodystrophia lipomatosa: Revisitation. Arch Plast Surg 2015;42:391-406.
- Upadhyay D, Parashari UC, Khanduri S, Bhadury S. Macrodystrophia lipomatosa: Radiologic-pathologic correlation. J Clin Imaging Sci 2011;1:18.


 PDF
PDF  Views
Views  Share
Share

