Juvenile granulosa cell tumor associated with Ollier disease
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(04): 293-295
DOI: DOI: 10.4103/0971-5851.195749
Abstract
Juvenile granulosa cell tumor (JGCT) is a rare neoplasm of childhood. Interestingly, it is known to be associated with Ollier disease, which is a rare bone disease characterized by multiple enchondromatosis. There is paucity of literature about the co-occurence of these two conditions. However, this association is noteworthy because these two conditions share a common pathogenesis. We report a case of JGCT in a 2.5-year-old female child in which multiple enchondromas mimicking bony metastasis were an incidental finding during routine workup for tumor staging, thus leading to a diagnosis of Ollier disease.
Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Juvenile granulosa cell tumor (JGCT) is a rare neoplasm of childhood. Interestingly, it is known to be associated with Ollier disease, which is a rare bone disease characterized by multiple enchondromatosis. There is paucity of literature about the co-occurence of these two conditions. However, this association is noteworthy because these two conditions share a common pathogenesis. We report a case of JGCT in a 2.5-year-old female child in which multiple enchondromas mimicking bony metastasis were an incidental finding during routine workup for tumor staging, thus leading to a diagnosis of Ollier disease.
INTRODUCTION
Ovarian juvenile granulosa cell tumor (JGCT) is an extremely rare sex cord-stromal tumor of the ovary that accounts for 2%–5% of malignant ovarian neoplasms.[1] Its association with Ollier disease has rarely been described in the literature.[2] Enchondromatosis or Ollier disease, which has an estimated prevalence of 1 in 100,000, is a condition of mesodermal dysplasia characterized by the derangement of cartilaginous growth resulting in incorporation of fragments of the epiphyseal plate within mature bone which subsequently develop into multiple enchondromas within the metaphysis.[3] When enchondromatosis is associated with hemangiomas or lymphangiomas, then the condition is known as Maffucci syndrome.[4,5] Chondrosarcoma is a frequently encountered malignancy in Ollier disease with an estimated risk of 30%–50%, but its association with JGCT draws attention toward the fact that there is a generalized mesodermal dysplasia in patients with enchondromatosis.[6,7] This case report is an attempt to address the fact that patients with Ollier disease should be screened for mesodermal neoplasms.
CASE REPORT
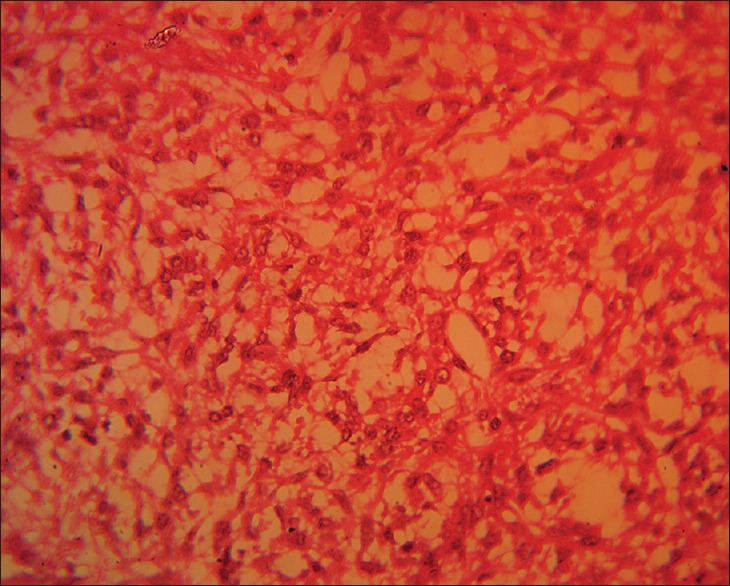
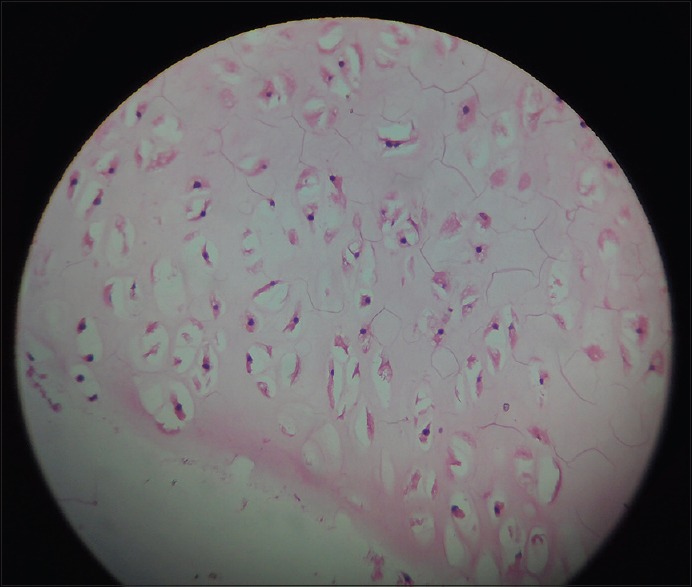
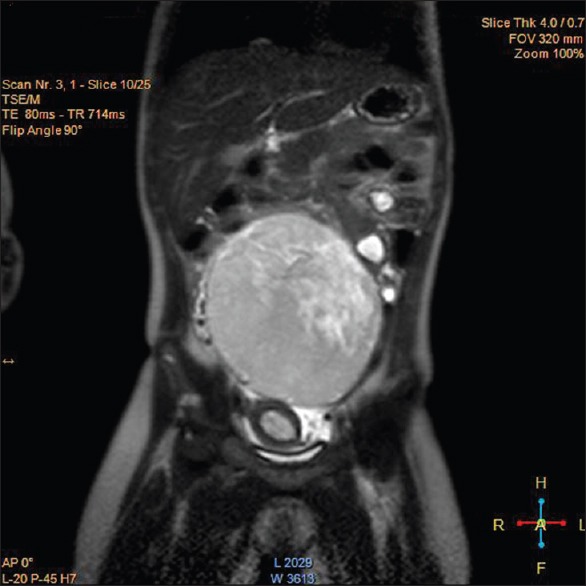
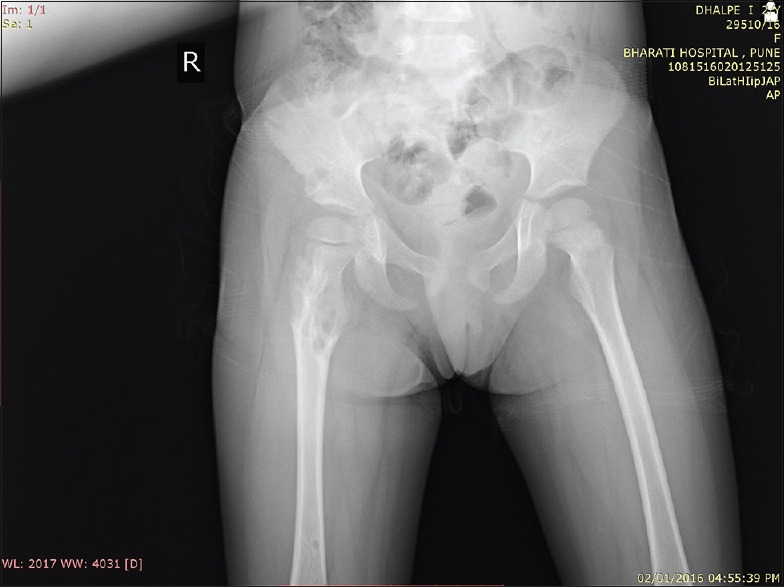
A 2.5-year-old female child presented with precocious puberty. Sexual maturity rating by tanner staging was Stage 2. On abdominal palpation, a hard mass was felt in the right hypochondrium. Magnetic resonance imaging (MRI) of abdomen and pelvis revealed a well-defined right ovarian mass measuring 10 cm × 5 cm × 11 cm with cystic and necrotic areas [Figure 1]. Another incidental finding noted on T2-weighted MRI study was multiple small lobulated foci of increased signal intensity separated by a background mesh of decreased signal intensity in the right femoral neck, greater and lesser trochanter, and the right iliac blade which were reported as metastatic lesions. These incidental MRI findings were correlated with the skeletal radiographs which showed expansile lytic lesions with thinning of the cortex [Figure 2]. No other site apart from those seen in the MRI was involved, thus confirming the unilateral distribution of the lesions. The ovarian tumor was surgically removed [Figure 3]. Tumor microscopy revealed macrofollicles lined by 2–3 layers of granulosa cells. The islands of granulosa cells showed Call-Exner bodies [Figure 4]. Tumor cells expressed inhibin, calretinin, melan-A (focal), and cytokeratin. Although the tumor was well localized but peritoneal aspirate was positive for malignant cell but the omental biopsy specimen was not involved. Thus, the diagnosis of JGCT 1C3 (as per new FIGO staging) was established. Bone scan was done to confirm metastasis, but there was no evidence of osteoblastic skeletal metastasis. She was further subjected to biopsy of the bone lesions to find out the nature of lytic lesions. The biopsy specimen contained cartilaginous elements which were reported as enchondromas [Figure 5]. Hence, the final diagnosis was Ollier disease with JGCT. A significant regression of the breast size and pubic hair was noted few weeks after the surgery. The patient was put on chemotherapy as per germ cell tumor protocol, and parents were counseled about the risk for the development of chondrosarcoma and the need for regular follow-up.

| Fig. 3 Surgical removal of the ovarian tumor
| Fig. 4 High-power view of the granulosa cells with call–exner bodies (granulosa cells tend to form primitive follicle seen as empty spaces between granulosa cells)
| Fig. 5 Enchondromas
DISCUSSION
The present case describes unusual association of two rare conditions. Ollier disease is a nonfamilial disorder.[8] There are very few case reports of this association, and these enchondromas were an incidental finding. According to the literature, the mean age of presentation of JGCT is 13 years.[9] The common clinical manifestation of Ollier disease is limb length discrepancy due to its characteristic involvement of one hemiskeleton or enchondromas in the phalanges and metacarpals.[10] However, in our case, Ollier disease was diagnosed on the basis of imaging and biopsy findings, even though the patient had not developed the clinical manifestation of the disease. Although this is an unusual association it emphasizes generalized mesodermal dysplasia in enchondromatosis and points toward the risk of development of ovarian neoplasms in addition to the commonly encountered chondrosarcomas which usually manifest in the second decades of life.[8] Another very interesting aspect of this case was maternal history of intake of ovulation-inducing drugs for a prolonged period of 2 years as a part of infertility treatment before this conception. Hence, this case supports the fact that intake of estrogen containing compounds is an etiological factor for the development of granulosa cell tumors.[11]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
| Fig. 1 Ovarian tumor with multiple small lobulated foci of increased signal intensity in the right femur
| Fig. 2 Lytic lesions in the right femur in the X-ray

| Fig. 3 Surgical removal of the ovarian tumor
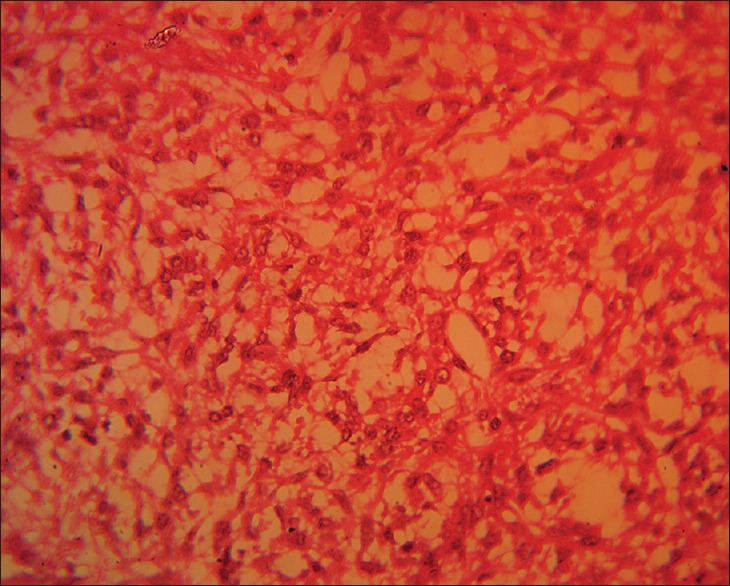
| Fig. 4 High-power view of the granulosa cells with call–exner bodies (granulosa cells tend to form primitive follicle seen as empty spaces between granulosa cells)
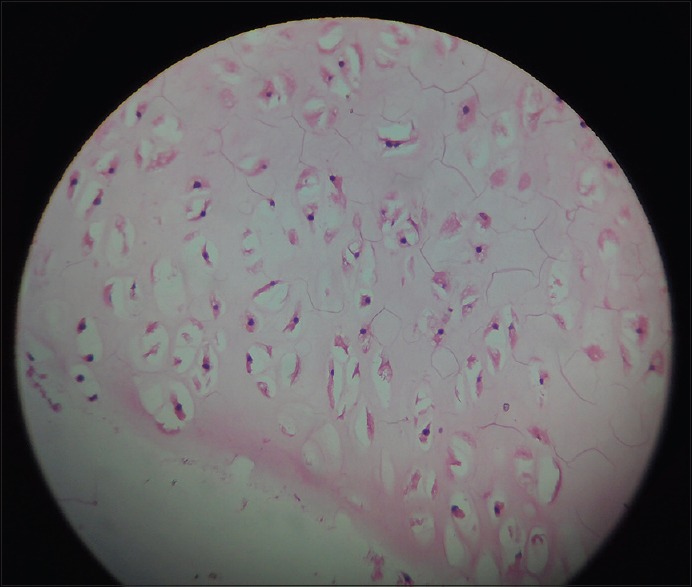
| Fig. 5 Enchondromas


 PDF
PDF  Views
Views  Share
Share

