Ischaemic optic neuropathy induced sudden blindness as an initial presentation of acute lymphoblastic leukemia
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2013; 34(04): 335-336
DOI: DOI: 10.4103/0971-5851.125266
Publication History
Article published online:
19 July 2021
© 2013. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Sir,
We report a 18-year-old male with ischaemic optic neuropathy of the left eye, leading to irreversible blindness as an initial presentation of high-risk T-cell acute lymphoblastic leukemia (ALL). Visual symptoms due to optic nerve infiltration by leukemic cells are rarely found in ALL. Blindness due to ischaemic optic neuropathy as the first presentation of ALL is extremely rare.
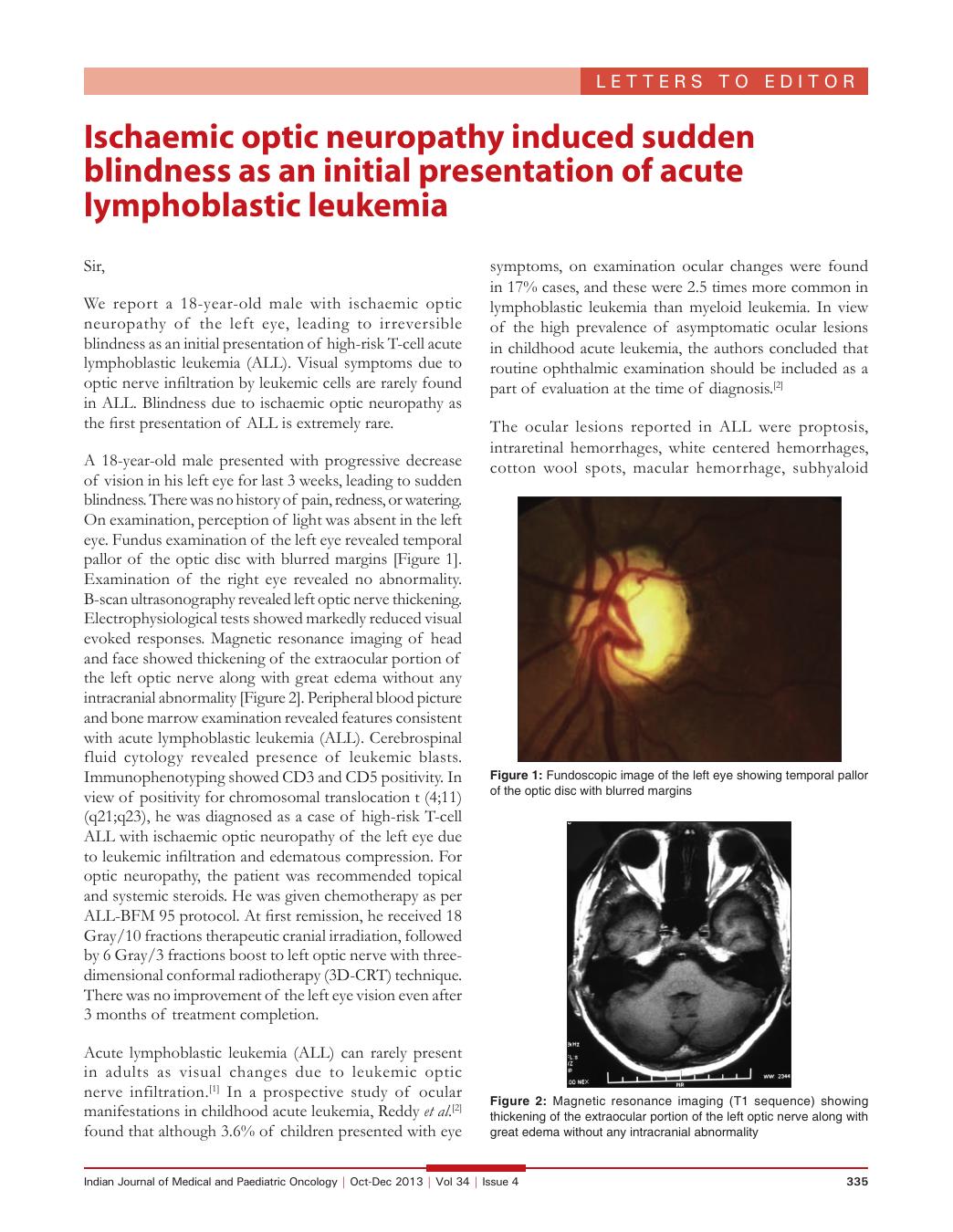
A 18-year-old male presented with progressive decrease of vision in his left eye for last 3 weeks, leading to sudden blindness. There was no history of pain, redness, or watering. On examination, perception of light was absent in the left eye. Fundus examination of the left eye revealed temporal pallor of the optic disc with blurred margins [Figure 1]. Examination of the right eye revealed no abnormality. B-scan ultrasonography revealed left optic nerve thickening. Electrophysiological tests showed markedly reduced visual evoked responses. Magnetic resonance imaging of head and face showed thickening of the extraocular portion of the left optic nerve along with great edema without any intracranial abnormality [Figure 2]. Peripheral blood picture and bone marrow examination revealed features consistent with acute lymphoblastic leukemia (ALL). Cerebrospinal fluid cytology revealed presence of leukemic blasts. Immunophenotyping showed CD3 and CD5 positivity. In view of positivity for chromosomal translocation t (4;11) (q21;q23), he was diagnosed as a case of high-risk T-cell ALL with ischaemic optic neuropathy of the left eye due to leukemic infiltration and edematous compression. For optic neuropathy, the patient was recommended topical and systemic steroids. He was given chemotherapy as per ALL-BFM 95 protocol. At first remission, he received 18 Gray/10 fractions therapeutic cranial irradiation, followed by 6 Gray/3 fractions boost to left optic nerve with three-dimensional conformal radiotherapy (3D-CRT) technique. There was no improvement of the left eye vision even after 3 months of treatment completion.
| Fig. 1 Fundoscopic image of the left eye showing temporal pallor of the optic disc with blurred margins

| Fig. 2 Magnetic resonance imaging (T1 sequence) showing thickening of the extraocular portion of the left optic nerve along with great edema without any intracranial abnormality
Acute lymphoblastic leukemia (ALL) can rarely present in adults as visual changes due to leukemic optic nerve infiltration.[1] In a prospective study of ocular manifestations in childhood acute leukemia, Reddy et al.[2] found that although 3.6% of children presented with eye symptoms, on examination ocular changes were found in 17% cases, and these were 2.5 times more common in lymphoblastic leukemia than myeloid leukemia. In view of the high prevalence of asymptomatic ocular lesions in childhood acute leukemia, the authors concluded that routine ophthalmic examination should be included as a part of evaluation at the time of diagnosis.[2]
The ocular lesions reported in ALL were proptosis, intraretinal hemorrhages, white centered hemorrhages, cotton wool spots, macular hemorrhage, subhyaloid hemorrhage, vitreous hemorrhage, papilledema, cortical blindness, sixth nerve palsy, exudative retinal detachment with choroidal infiltration;[1,2] peripheral ulcerative keratitis with bilateral optic nerve involvement;[3] central retinal artery occlusion associated with leukemic optic neuropathy.[4]
Ocular involvement in lymphoproliferative disorders other than ALL have also been reported e.g. in myeloid leukemia,[2] and Hodgkin's disease.[5]
Acute-onset optic neuropathy in a patient with a history of lymphoproliferative disorder may be the only sign of a re-emergence of the malignancy.[5,6]
In some reports, there was dramatic improvement of vision with urgent radiotherapy and high-dose systemic corticosteroids in leukemic or lymphomatous optic nerve infiltration.[1,5] However, no visual gain could be achieved in some reports,[3] like in our patient, and the probable causes might be late presentation with irreversible optic nerve damage and delay in radiotherapy.
| Fig. 1 Fundoscopic image of the left eye showing temporal pallor of the optic disc with blurred margins

| Fig. 2 Magnetic resonance imaging (T1 sequence) showing thickening of the extraocular portion of the left optic nerve along with great edema without any intracranial abnormality


 PDF
PDF  Views
Views  Share
Share

