Incidentally Discovered Appendiceal Mucinous Neoplasm in a 5-month-old Patient: A Case Report and Review of Literature
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(02): 250-253
DOI: DOI: 10.4103/ijmpo.ijmpo_82_18
Abstract
Mucocele of the appendix is a rare entity in pediatrics, and few case reports have been reported in the literature. We present the case of a 5-month-old male with abdominal distension, constipation, and vomiting who was found to have an appendiceal mucocele while being evaluated for total colonic aganglionosis. Laparoscopic-assisted resection was performed, with pathology confirming a low-grade mucinous neoplasm of the appendix. He underwent complete resection, rendering him cured without the need for any further resection or treatment.
Keywords
Appendix - low-grade mucinous neoplasm - mucocele
Publication History
Received: 11 April 2018
Accepted: 18 October 2018
Article published online:
23 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Mucocele of the appendix is a rare entity in pediatrics, and few case reports have been reported in the literature. We present the case of a 5-month-old male with abdominal distension, constipation, and vomiting who was found to have an appendiceal mucocele while being evaluated for total colonic aganglionosis. Laparoscopic-assisted resection was performed, with pathology confirming a low-grade mucinous neoplasm of the appendix. He underwent complete resection, rendering him cured without the need for any further resection or treatment.
Keywords
Appendix - low-grade mucinous neoplasm - mucocele
Introduction
Appendiceal mucocele (AM) was first described by Rokitansky in 1842 as a dilation of the appendiceal lumen due to the accumulation of mucinous secretions.[1] AM has an incidence of 0.2%–0.3% of all appendectomies with predilection for females aged above 50 years.[2] Clinical presentation is variable, and it most often presents as an incidental finding in asymptomatic patients.[2] Less frequently, patients may present with acute appendicitis or abdominal fullness with an associated mass in the iliac fossa.[3] [4] Mucoceles due to appendiceal mucinous neoplasms are exceedingly rare in the pediatric population.[5] We describe the case of a 5-month old child who presented with abdominal distension, constipation, and vomiting and was suspected as total colonic aganglionosis. Mucocele of the appendix was an incidental finding observed while performing exploratory laparotomy for the same. Microscopy revealed low-grade mucinous neoplasm of the appendix. To the best of our knowledge, this is the first case report of low-grade mucinous neoplasm of the appendix in a 5-month-old child.
Case Report
A 5-month-old boy presented with abdominal distension and constipation for 2 weeks. The patient also had multiple episodes of vomiting which was nonprojectile and nonbilious. On X-ray, dilated bowel loops were seen. Exploratory laparotomy was done in view of the diagnosis of total colonic aganglionosis. Intraoperatively, the whole of the small intestine up to the cecum was dilated and the whole of the colon beyond the cecum was collapsed. The cecum was mobile and present in the right iliac fossa. Divided ileostomy was performed, and biopsy from the ascending colon and sigmoid colon was taken. Biopsy from the ascending colon showed unremarkable mucosa and occasional ganglion cells in the mesenteric plexus. Biopsy from the sigmoid colon was inadequate for any opinion. The patient was discharged 3 days after the symptomatic improvement. Two months after the procedure, the patient developed distal stoma prolapse for which the parents consulted the surgeon. The patient again had episodes of vomiting and stopped accepting feeds. Repeat surgery was done for reduction of the prolapsed loop. Biopsy from the stomal end of the ileum, transverse colon, and rectosigmoid junction was taken. Mucocele of the appendix was observed. There was no free fluid or any mucinous deposits in the peritoneal cavity. The appendix was removed and sent for histopathology. The gross specimen of the appendix was dilated and measured 4 cm in length with luminal diameter of 1.5 cm. External surface was unremarkable. Lumen was filled with mucoid material. Multiple small cysts measuring 0.1–0.2 cm were identified in mesoappendix filled with mucoid and chalky material [Figure 1]. No solid area was seen. Microscopy revealed dilated appendix lined by cuboidal epithelium [Figure 2]a with focal presence of apical mucin vacuoles. Nuclei showed mild hyperchromasia and pleomorphism. The wall was composed of fibrocollagenous tissue [Figure 2]a. No submucosa or muscle layer was identified. There was no evidence of cellular infiltration. Mucin pools [Figure 2]b and foci of calcification were also noted in mesoappendix; however, no epithelial lining was seen. Surrounding tissue showed mild chronic inflammation, vascular congestion, and surface fibrinous exudate. Section from the proximal resected margin also revealed similar findings. No parasite, stone, or fecolith was identified. Biopsy from the transverse colon and sigmoid colon revealed the presence of ganglion cells. Biopsy from the stomal margin showed largely unremarkable mucosa with focal surface denudation, edema, and congestion in the submucosa. Diagnosis of low-grade appendiceal mucinous neoplasm (LAMN) with low risk of recurrence was given.
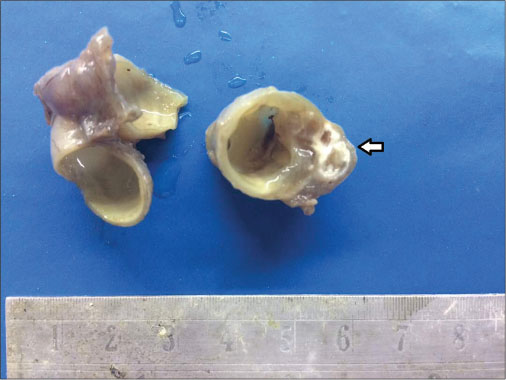
| Figure 1: Dilated appendix with the thinned out wall. Chalky white calcification and gelatinous material is also noted (arrow)
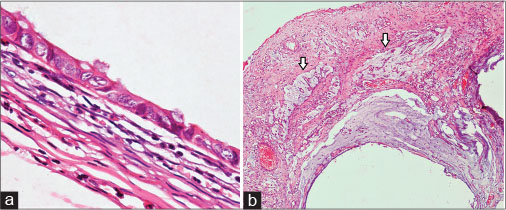
| Figure 2: (a) Cyst lined by cuboidal epithelium with mildly hyperchromatic and pleomorphic nuclei. The wall shows fibrocollagenous tissue (H and E, ×40). (b) Mucin pools in mesoappendix (arrow) (H and E, ×40)
Discussion
Primary neoplasms of the appendix are present in <2% of appendectomy specimens.[6] These are rare in the pediatric population and are found in <0.5% of specimens submitted.[5] Mucinous neoplasms of the appendix are a complex group of neoplasms which usually cause cystic dilation of the appendix due to the accumulation of gelatinous material and are morphologically referred to as mucoceles. Mucinous appendiceal adenocarcinomas are most commonly found incidentally on imaging studies as a cystic right lower quadrant mass or in a patient with increasing abdominal girth secondary to pseudomyxoma peritonei (PMP). Less than one-third of mucinous appendiceal adenocarcinomas manifest as acute appendicitis. AMs are frequently misdiagnosed on imaging studies. AMs are distinguished from acute appendicitis by radiologic criteria with an appendiceal outer diameter 15 mm or greater and possible visualization of mucinous effusion. Contrast-enhanced computed tomography (CT) is most commonly used for the preoperative diagnosis. CT findings of appendiceal lumen >1.3 cm, with cystic dilation and wall calcification, suggest mucocele. Mucinous cystadenomas specifically present with cystic masses, low contrast attenuation, irregular wall thickening, and absence of inflammation.[7]
Appendiceal mucinous neoplasms are rarely seen in the pediatric population, as they present in the sixth decade of life. Alemayehu et al. did not find a single case of mucinous neoplasm while reporting the incidence of unexpected pathology findings after appendectomy in 3602 children over a 16-year period.[5] Pai et al. found only two patients aged below 20 years in 116 cases of appendiceal mucinous neoplasms observed over 30 years.[8] Blecha et al. reported the case of a 10-year old boy who found to have a mucocele of the appendix with a cystadenoma.[9]
Appendiceal mucinous tumors represent a diverse group ranging from benign to malignant neoplasms, with numerous proposed classifications and subtypes. Carr and Sobin, Pai and Longacre, Misdraji et al. and WHO 2010 classification were similar in that they all define benign neoplastic adenoma as the entity which is confined to the mucosa, without the penetration of the muscularis mucosa by the cells and mucin. They all described invasive adenocarcinoma as a neoplastic lesion with cellular invasion beyond the muscularis mucosa. All the proposed schemes differ in their classification of adenomatous growths with mucin dissection beyond the muscularis mucosa or mural perforation, where peritoneal dissemination could lead to PMP. The latter were variably referred to as appendiceal neoplasms of uncertain malignant potential or LAMNs.[10] Pai et al. divided LAMNs into two categories based on the association with acellular or cellular mucinous ascites into low risk of recurrence or at high risk of recurrence, respectively.[11]
The WHO classifies mucinous appendiceal neoplasms into two groups: LAMN and mucinous adenocarcinoma.[12] Appendices with LAMNs may appear grossly unremarkable or may be cystically dilated and filled with mucin. The wall may be thin or fibrotic, hyalinized, and calcified. Gross rupture may show mucin in the wall or on the serosal surface.[13] Microscopically, LAMNs have villous, serrated, or undulating architecture, which often resembles adenoma. These have “broad-front invasion” which is characterized by atrophy and fibrosis of underlying submucosa and muscularis propria, but no desmoplasia. Neoplastic epithelium growing above fibrotic or hyalinized stroma rather than lamina propria and muscularis mucosae is commonly seen and considered as a sign of pushing invasion.[13] Cells may be columnar, cuboidal, or flattened and are present in single layer. Large mucin vacuoles are common in columnar cells which may compress the nuclei to the cell base. Nuclei are small and irregular. Low-grade dysplasia may be present, but mitosis is rare.[12] Usual features of infiltrative-type invasion, such as single-cell invasion, tumor budding, or desmoplastic stromal response, are absent. The wall of the appendix may be totally breached, giving a picture of a ruptured cystic tumor with mucin extrusion onto the peritoneal surface, with or without the presence of mucinous epithelial cells in that mucin. The main diagnostic challenge while evaluating a LAMN is that they resemble adenomas in terms of their low-grade cytology and architecture,[13] but unlike adenomas, LAMNs rest on fibrous tissue rather than lamina propria.[12] When a tumor has disseminated to the peritoneal cavity, it is still a debate about whether the tumor should be classified as LAMN or as adenocarcinoma.[13]
We considered this case as LAMN because of acellular extra-appendiceal mucin and involvement of proximal margin of the appendix.
Benign processes can mimic LAMNs when they are associated with mucinous epithelial hyperplasia, perforation, or mucin extrusion into the wall or onto the serosa. The most common entity which mimics LAMN is appendiceal diverticular disease which may rupture and cause extrusion of mucin into the wall or onto the appendiceal serosa. Ruptured diverticulum can be differentiated from a mucinous neoplasm by the presence of intact diverticula. Hyperplastic and reactive changes of the lining epithelium within the diverticula may also be confused with a neoplastic process, but the architectural changes, such as gland serration, crypt disarray, and hyperplastic changes with abundant mucin-producing cells, are more appreciated in the superficial rather than the basal portions of the mucosa. Typical LAMNs show back-to-back arrangement of the crypts with scant lamina propria and elongated slender villi as compared to the nonneoplastic crypts which are normally separated by lamina propria and show little or no crowding. Another rare differential is endometriosis with intestinal metaplasia which can lead to mucin extrusion on the appendiceal serosa, causing confusion with a ruptured LAMN.[13]
Appendiceal mucinous neoplasms usually express the similar immunophenotype as those of mucinous tumors of lower intestinal tract, i.e., CK20, CDX2, or β-catenin (lower percentage of homogenous CDX2 and β-catenin).[14] The proportion of CK7-positive cells in mucinous neoplasm of the appendix is higher than in the colorectal ones, but significantly lower than the ovary, pancreatic, or upper gastrointestinal mucinous tumors. The universal molecular marker for appendiceal mucinous tumors and PMP is MUC2. MUC5A is positive in >80% of mucinous appendiceal neoplasms, and its overexpression is associated with an intestinal origin for PMP, especially if the appendiceal primary location was reported. The frequency of Ki67 antigen expression may differentiate adenocarcinoma from LAMN and mucinous adenoma. By analyzing the immunochemistry for 24 markers, Yoon et al. tried to identify differential immunoexpression profiles of proteins in mucinous adenoma, LAMN, and mucinous adenocarcinoma and established a panel of nine markers – status representative for appendiceal mucinous adenocarcinoma: cyclin D1 positive, Ki67 high index, nuclear factor-κB positive, vascular endothelial growth factor positive, E-cadherin loss, p53 overexpression, β-catenin loss, MUC2 positive, and MUC5A positive (>80%).[15]
Treatment of mucinous neoplasms of appendix depends on the presence or absence of extra-appendiceal mucin and the status of the proximal margin. If there is no mucin or neoplastic epithelium in the appendiceal base or periappendiceal tissue, laparoscopic appendectomy is preferred. If there is macroscopic mucinous fluid, cytology would be necessary to confirm the presence of the epithelial cells. Once a LAMN ruptures, the risk of developing PMP is defined by whether the mucin extruded is acellular or cellular. LAMNs associated with acellular mucin but confined to the right lower quadrant carry a very low risk of recurrence or progression to PMP, whereas those associated with mucin and neoplastic mucinous epithelial cells in the right lower quadrant carry a relatively high risk of recurrence.[13] Right hemicolectomy has no additional benefit over appendectomy alone for these patients. Appendectomy or cecectomy with a negative margin is preferred. Precautions to avoid rupture in the peritoneal cavity and dissemination of mucin should be taken in the laparoscopic approach. Conversion to open surgery is recommended if the tumor clearly extends beyond the appendix. Surgical debulking and heated intraperitoneal chemotherapy is preferred for the patients with peritoneal deposits.[13]
Our patient was a 5-month old child, and low-grade mucinous neoplasm of the appendix was an incidental finding as the patient was operated for suspected total colonic aganglionosis and appendectomy alone was done. The patient is doing well after 6 months of surgery with no gastrointestinal complications.
Conclusion
Appendiceal mucinous neoplasms are rare tumors in the pediatric population, but should be considered when a mucocele is identified preoperatively or intraoperatively. LAMN is a low-grade neoplasm treated by complete surgical resection when confined to the appendix. A laparoscopic-assisted approach with careful handling is advised, and an extracorporeal resection may assist in assuring negative margins and subsequent cure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
References
- Rokitanksy CF. A Manual of Pathological Anatomy. 2. Philadelphia: Blanchard and Lea; 1855
- Malya FU, Hasbahceci M, Serter A, Cipe G, Karatepe O, Kocakoc E. et al. Appendiceal mucocele: Clinical and imaging features of 14 cases. Chirurgia (Bucur) 2014; 109: 788-93
- Hassan S, Dhebri A, Lin L, Haque M. Appendiceal mucocele: A missed diagnosis. BMJ Case Rep 2013;2013. pii: bcr2012007983
- Stocchi L, Wolff BG, Larson DR, Harrington JR. Surgical treatment of appendiceal mucocele. Arch Surg 2003; 138: 585-9
- Alemayehu H, Snyder CL, St Peter SD, Ostlie DJ. Incidence and outcomes of unexpected pathology findings after appendectomy. J Pediatr Surg 2014; 49: 1390-3
- Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: Retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum 1998; 41: 75-80
- Padmanaban V, Morano WF, Gleeson E, Aggarwal A, Mapow BL, Stein DE. et al. Incidentally discovered low-grade appendiceal mucinous neoplasm: A precursor to pseudomyxoma peritonei. Clin Case Rep 2016; 4: 1112-6
- Pai RK, Beck AH, Norton JA, Longacre TA. Appendiceal mucinous neoplasms: Clinicopathologic study of 116 cases with analysis of factors predicting recurrence. Am J Surg Pathol 2009; 33: 1425-39
- Blecha MJ, Gupta A, Hoover JD, Madonna MB. Chronic abdominal pain secondary to a mucous cystadenoma of the appendix in a 10-year-old boy. J Pediatr Surg 2005; 40: 1792-4
- Misdraji J. Appendiceal mucinous neoplasms: Controversial issues. Arch Pathol Lab Med 2010; 134: 864-70
- Pai RK, Longacre TA. Appendiceal mucinous tumors and pseudomyxoma peritonei: Histologic features, diagnostic problems, and proposed classification. Adv Anat Pathol 2005; 12: 291-311
- Carr N, Sobin L. Tumors of the appendix. In: Bosman FT, Carneiro F, Hruban RH, Theise ND. editors World Health Organization Classification of Tumours of the Digestive System. 4th ed. 3. Lyon, France: IARC Press; 2010: 122-5
- Misdraji J. Mucinous epithelial neoplasms of the appendix and pseudomyxoma peritonei. Mod Pathol 2015; 28 Suppl (01) S67-79
- Chu PG, Chung L, Weiss LM, Lau SK. Determining the site of origin of mucinous adenocarcinoma: An immunohistochemical study of 175 cases. Am J Surg Pathol 2011; 35: 1830-6
- Yoon SO, Kim BH, Lee HS, Kang GH, Kim WH, Kim YA. et al. Differential protein immunoexpression profiles in appendiceal mucinous neoplasms: A special reference to classification and predictive factors. Mod Pathol 2009; 22: 1102-12
Address for correspondence
Publication History
Received: 11 April 2018
Accepted: 18 October 2018
Article published online:
23 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
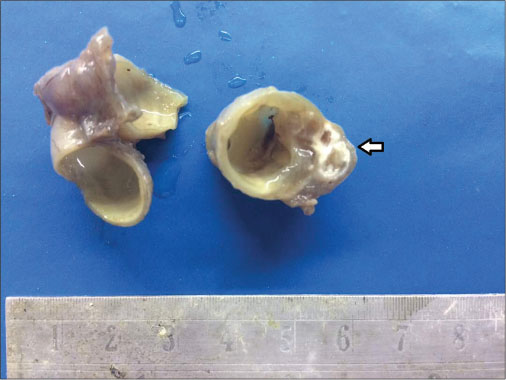
| Figure 1: Dilated appendix with the thinned out wall. Chalky white calcification and gelatinous material is also noted (arrow)
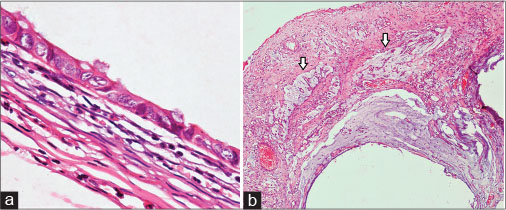
| Figure 2: (a) Cyst lined by cuboidal epithelium with mildly hyperchromatic and pleomorphic nuclei. The wall shows fibrocollagenous tissue (H and E, ×40). (b) Mucin pools in mesoappendix (arrow) (H and E, ×40)
References
- Rokitanksy CF. A Manual of Pathological Anatomy. 2. Philadelphia: Blanchard and Lea; 1855
- Malya FU, Hasbahceci M, Serter A, Cipe G, Karatepe O, Kocakoc E. et al. Appendiceal mucocele: Clinical and imaging features of 14 cases. Chirurgia (Bucur) 2014; 109: 788-93
- Hassan S, Dhebri A, Lin L, Haque M. Appendiceal mucocele: A missed diagnosis. BMJ Case Rep 2013;2013. pii: bcr2012007983
- Stocchi L, Wolff BG, Larson DR, Harrington JR. Surgical treatment of appendiceal mucocele. Arch Surg 2003; 138: 585-9
- Alemayehu H, Snyder CL, St Peter SD, Ostlie DJ. Incidence and outcomes of unexpected pathology findings after appendectomy. J Pediatr Surg 2014; 49: 1390-3
- Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: Retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum 1998; 41: 75-80
- Padmanaban V, Morano WF, Gleeson E, Aggarwal A, Mapow BL, Stein DE. et al. Incidentally discovered low-grade appendiceal mucinous neoplasm: A precursor to pseudomyxoma peritonei. Clin Case Rep 2016; 4: 1112-6
- Pai RK, Beck AH, Norton JA, Longacre TA. Appendiceal mucinous neoplasms: Clinicopathologic study of 116 cases with analysis of factors predicting recurrence. Am J Surg Pathol 2009; 33: 1425-39
- Blecha MJ, Gupta A, Hoover JD, Madonna MB. Chronic abdominal pain secondary to a mucous cystadenoma of the appendix in a 10-year-old boy. J Pediatr Surg 2005; 40: 1792-4
- Misdraji J. Appendiceal mucinous neoplasms: Controversial issues. Arch Pathol Lab Med 2010; 134: 864-70
- Pai RK, Longacre TA. Appendiceal mucinous tumors and pseudomyxoma peritonei: Histologic features, diagnostic problems, and proposed classification. Adv Anat Pathol 2005; 12: 291-311
- Carr N, Sobin L. Tumors of the appendix. In: Bosman FT, Carneiro F, Hruban RH, Theise ND. editors World Health Organization Classification of Tumours of the Digestive System. 4th ed. 3. Lyon, France: IARC Press; 2010: 122-5
- Misdraji J. Mucinous epithelial neoplasms of the appendix and pseudomyxoma peritonei. Mod Pathol 2015; 28 Suppl (01) S67-79
- Chu PG, Chung L, Weiss LM, Lau SK. Determining the site of origin of mucinous adenocarcinoma: An immunohistochemical study of 175 cases. Am J Surg Pathol 2011; 35: 1830-6
- Yoon SO, Kim BH, Lee HS, Kang GH, Kim WH, Kim YA. et al. Differential protein immunoexpression profiles in appendiceal mucinous neoplasms: A special reference to classification and predictive factors. Mod Pathol 2009; 22: 1102-12


 PDF
PDF  Views
Views  Share
Share

