Incendiary Appearance of a Scalp Lesion: Whether Benign or Malignant?
CC BY 4.0 · Indian J Med Paediatr Oncol 2025; 46(01): 093-095
DOI: 10.1055/s-0044-1795093
Case Summary
A 46-year-old woman presented to the surgical outpatient department with a 10-year history of scalp swelling in the occipital region. The swelling was initially small in size, which gradually increased to attain the size of a pebble ([Fig. 1]). There was no history of trauma preceding the onset of swelling. The patient did not complain of any pain, itching, or discoloration. On examination, the skin overlying the swelling was normal. The swelling was freely mobile in all directions and was not adherent to overlying skin or underlying structures. The consistency was soft to firm on palpation. The patient underwent surgical excision, and the specimen was sent for histopathological examination.

| | Fig 1Swelling in occipital region of the scalp. The overlying skin appears normal.|
Patient Consent
The authors certify that they have obtained all appropriate patient concent forms. in the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Publication History
Article published online:
13 December 2024
© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Benign versus malignant nodular breast lesion by using elastosonography: preliminary reportA. I. Ciurea, Ultraschall in der Medizin - European Journal of Ultrasound, 2008
- Malignant nodular hidradenoma of scalpDhaval Shukla, Journal of Neurosciences in Rural Practice, 2014
- Malignant nodular hidradenoma of scalpDhaval Shukla, Journal of Neurosciences in Rural Practice, 2014
- Metal Stents for Benign and Malignant Bile Duct Strictures Stents for Benign and Malignant Bile Duct StrictuesT. Rösch, Endoscopy, 1998
- Diagnostic Management of Benign and Malignant PheochromocytomaT. Scholz, Experimental and Clinical Endocrinology & Diabetes, 2007
- Uterine lipoleiomyoma: a benign entity with malignant transformation potential?Yunzhe Wan, European Journal of Gynaecological Oncology, 2022
- Antibiotic reduces appearance-based trustUsefulScience
- The last word on whether a union may ignore its constitutionVerushka Reddy, Without Prejudice, 2020
- Appearance of Endoproteolytic Enzymes during the Germination of BarleyRadoslawa Wrobel, Plant Phyisol, 1992
- Walking, whether outside or on a treadmill, leads to more creative thinkingUsefulScience
Case Summary
A 46-year-old woman presented to the surgical outpatient department with a 10-year history of scalp swelling in the occipital region. The swelling was initially small in size, which gradually increased to attain the size of a pebble ([Fig. 1]). There was no history of trauma preceding the onset of swelling. The patient did not complain of any pain, itching, or discoloration. On examination, the skin overlying the swelling was normal. The swelling was freely mobile in all directions and was not adherent to overlying skin or underlying structures. The consistency was soft to firm on palpation. The patient underwent surgical excision, and the specimen was sent for histopathological examination.

| | Fig 1Swelling in occipital region of the scalp. The overlying skin appears normal.|
Differential Diagnosis
The differential diagnoses considered on clinical examination in this case were lipoma, epidermoid cyst, and sebaceous cyst.
Histopathological Workup
Gross Examination
A partially skin-covered globular tissue mass measuring 2.0 × 1.4 × 0.8 cm was observed. It had a well-demarcated solid cystic swelling with a glossy white cyst wall ([Fig. 2]). The cut surface showed a firm whitish ovoid area measuring 1 × 0.6 × 0.6 cm with other cystic area filled with yellowish material ([Fig. 3]).
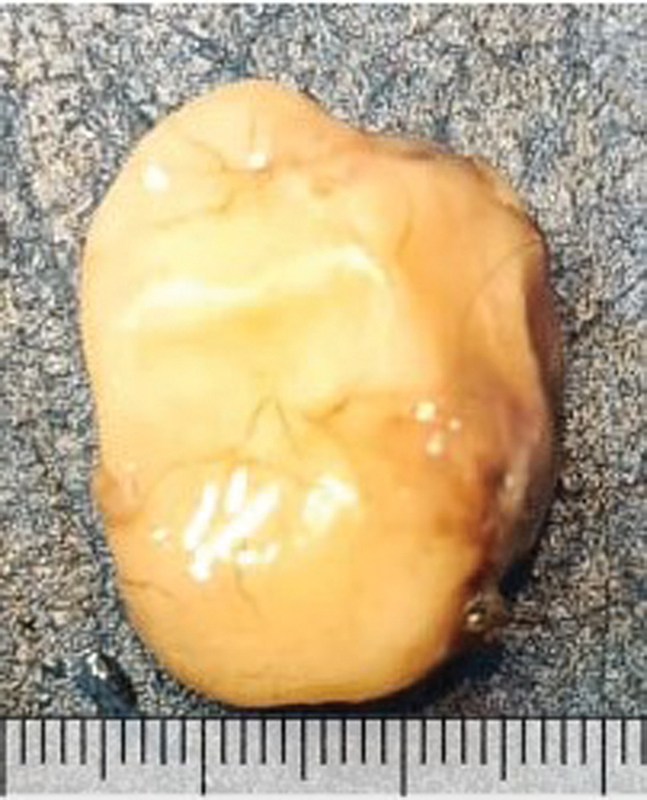
| Fig 2 Excision biopsy of the scalp lesion. The outer surface is glossy white in appearance.|

| Fig 3The cut surface of the solid cystic lesion, which showed a firm whitish ovoid solid area with other cystic area filled with yellowish material.|
|The cut surface of the solid cystic lesion, which showed a firm whitish ovoid solid area with other cystic area filled with yellowish material.|
Microscopy
The cyst wall was lined by a keratinized stratified squamous epithelium with the absence of a granular cell layer. Variable sized lobules of squamous epithelium were noted undergoing abrupt change into eosinophilic amorphous keratin. The proliferating epithelium showed pushing borders. The cyst cavity contained abundant keratin, cholesterol clefts, and areas of calcification. No granuloma or giant cells were present. No dysplasia existed ([Figs. 4],[5],[6],[7]).
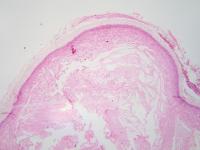
| Fig 4: Cystic cavity lined by keratinized stratified squamous epithelium with the absence of the granular layer. Cholesterol clefts are also evident (hematoxylin and eosin, ×40).|
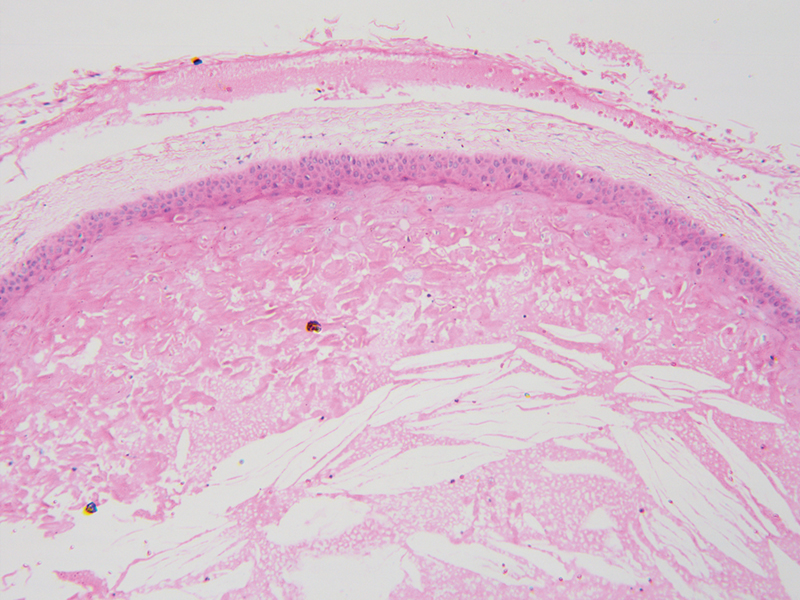
| Fig 5: Similar findings as in Fig. 4 but at a higher magnification. The keratin-filled cavity is better appreciable at this magnification (hematoxylin and eosin, ×100).|
| Similar findings as in Fig. 4 but at a higher magnification. The keratin-filled cavity is better appreciable at this magnification (hematoxylin and eosin, ×100).|
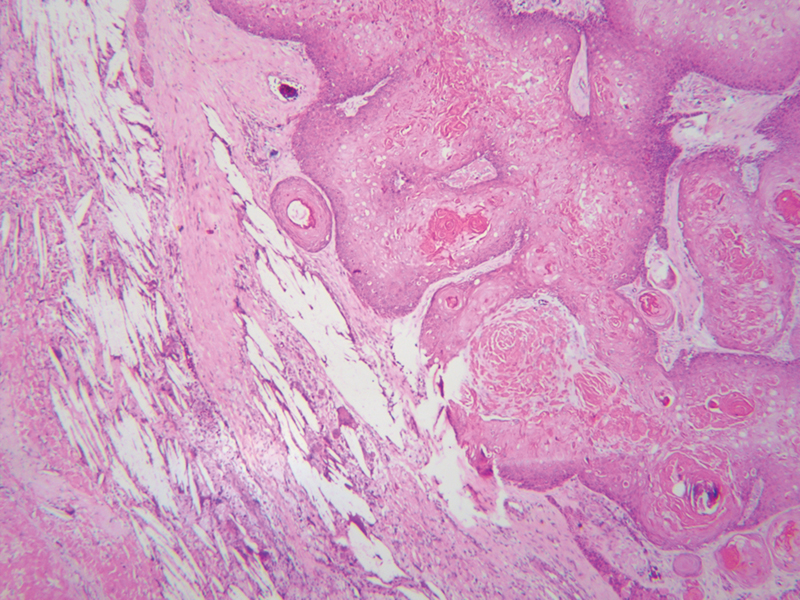
| Fig 6: Variable sized lobules of squamous epithelium undergoing abrupt change into eosinophilic amorphous keratin. The proliferating epithelium shows pushing borders. The lesion is considered a mimic of squamous cell carcinoma (hematoxylin and eosin, ×40).|
| Variable sized lobules of squamous epithelium undergoing abrupt change into eosinophilic amorphous keratin. The proliferating epithelium shows pushing borders. The lesion is considered a mimic of squamous cell carcinoma (hematoxylin and eosin, ×40).|
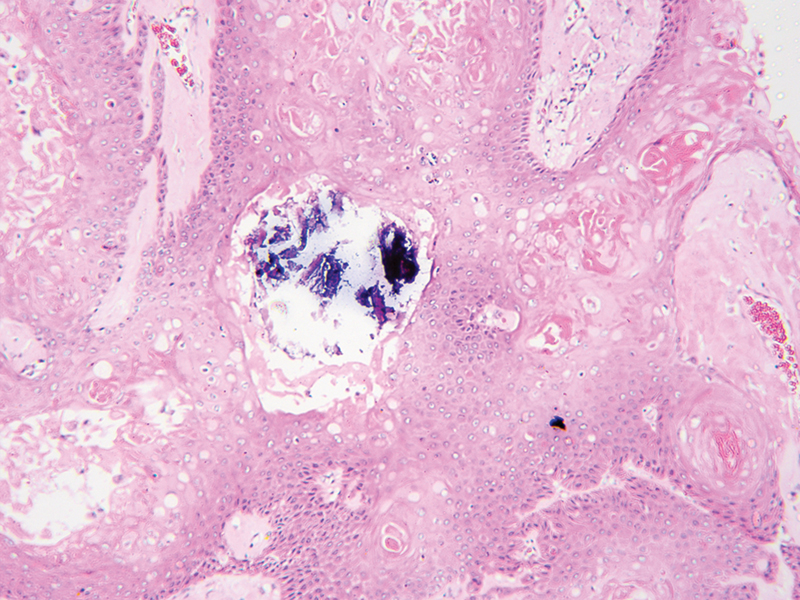
| Fig 7: Areas of calcification, which commonly occur in proliferating pilar tumors.
Diagnosis and Discussion
The low-power histomorphology of the lesion may mimic the appearance of a squamous cell carcinoma. However, the important differentiating points that need to be considered here are pilar-type keratinization, absence of a granular layer, presence of a well-defined capsule, and the presence of the proliferating part only within the capsule, which support the diagnosis of a proliferating pilar tumor.
This tumor was first described by E.W. Jones who referred to it as a proliferating epidermoid cyst, which has also been called a proliferating pilar tumor.[1] Other terms that are used for the condition include proliferating trichilemmal cyst, proliferating trichilemmal tumor, and pilar tumor of the scalp.[2] Although this has been considered a benign mimic of squamous cell carcinoma, there are few reports describing the malignant behavior of these tumors.[3] [4] Most cases are noted in women in the 43- to 66-year age range, with the most common location being the scalp.[5] The incendiary appearance of this lesion may create a diagnostic dilemma, but a thorough microscopic examination would lead to a definite diagnosis.
Conflict of Interest
None declared.
Patient Consent
The authors certify that they have obtained all appropriate patient concent forms. in the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
References
- Jones EW. Proliferating epidermoid cysts. Arch Dermatol 1966; 94 (01) 11-19
- Ye J, Nappi O, Swanson PE, Patterson JW, Wick MR. Proliferating pilar tumors: a clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol 2004; 122 (04) 566-574
- Osto M, Parry N, Rehman R, Ahmed U, Mehregan D. Malignant proliferating trichilemmal tumor of the scalp: a systematic review. Am J Dermatopathol 2021; 43 (12) 851-866
- Joshi TP, Marchand S, Tschen J. Malignant proliferating trichilemmal tumor: a subtle presentation in an African American woman and review of immunohistochemical markers for this rare condition. Cureus 2021; 13 (08) e17289
-
Alarcón Pérez CE,
Gómez Ángulo D,
Olmos Pérez M,
Mora Hernández O,
Morales SD.
Management of 3 proliferating pilar tumors: definition, differential diagnosis, and treatment options. Actas Dermosifiliogr (Engl Ed) 2019; 110 (10) 850-854
Address for correspondence
Dr. (Maj) Chinmay Shrikrishna Pendharkar, MBBS, MD, DNBDepartment of Pathology, Armed Forces Medical CollegePune 411040, MaharashtraIndiaPublication History
Article published online:
13 December 2024© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, IndiaWe recommend- Benign versus malignant nodular breast lesion by using elastosonography: preliminary reportA. I. Ciurea, Ultraschall in der Medizin - European Journal of Ultrasound, 2008
- Malignant nodular hidradenoma of scalpDhaval Shukla, Journal of Neurosciences in Rural Practice, 2014
- Malignant nodular hidradenoma of scalpDhaval Shukla, Journal of Neurosciences in Rural Practice, 2014
- Metal Stents for Benign and Malignant Bile Duct Strictures Stents for Benign and Malignant Bile Duct StrictuesT. Rösch, Endoscopy, 1998
- Dysphagia in Indian Patients—Benign Outnumber MalignantKapil Dhingra, Journal of Digestive Endoscopy, 2019
- Benign versus malignant nodular breast lesion by using elastosonography: preliminary report

| | Fig 1Swelling in occipital region of the scalp. The overlying skin appears normal.|
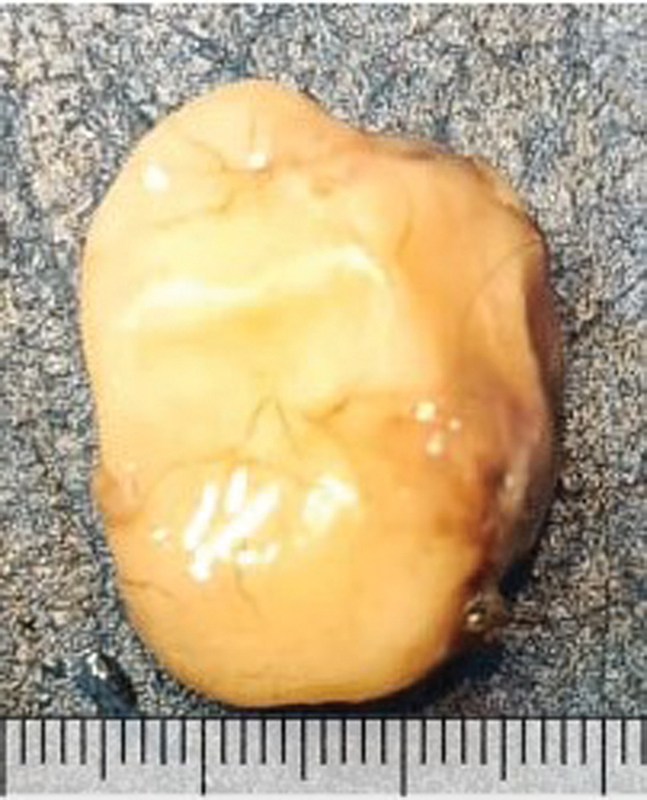
| Fig 2 Excision biopsy of the scalp lesion. The outer surface is glossy white in appearance.|

| Fig 3The cut surface of the solid cystic lesion, which showed a firm whitish ovoid solid area with other cystic area filled with yellowish material.|
|The cut surface of the solid cystic lesion, which showed a firm whitish ovoid solid area with other cystic area filled with yellowish material.|
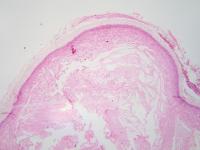
| Fig 4: Cystic cavity lined by keratinized stratified squamous epithelium with the absence of the granular layer. Cholesterol clefts are also evident (hematoxylin and eosin, ×40).|
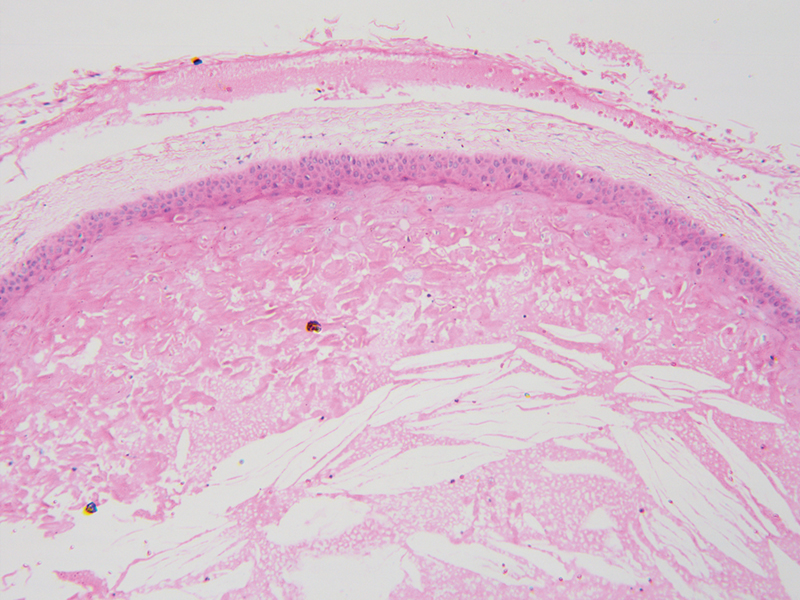
| Fig 5: Similar findings as in Fig. 4 but at a higher magnification. The keratin-filled cavity is better appreciable at this magnification (hematoxylin and eosin, ×100).|
| Similar findings as in Fig. 4 but at a higher magnification. The keratin-filled cavity is better appreciable at this magnification (hematoxylin and eosin, ×100).|
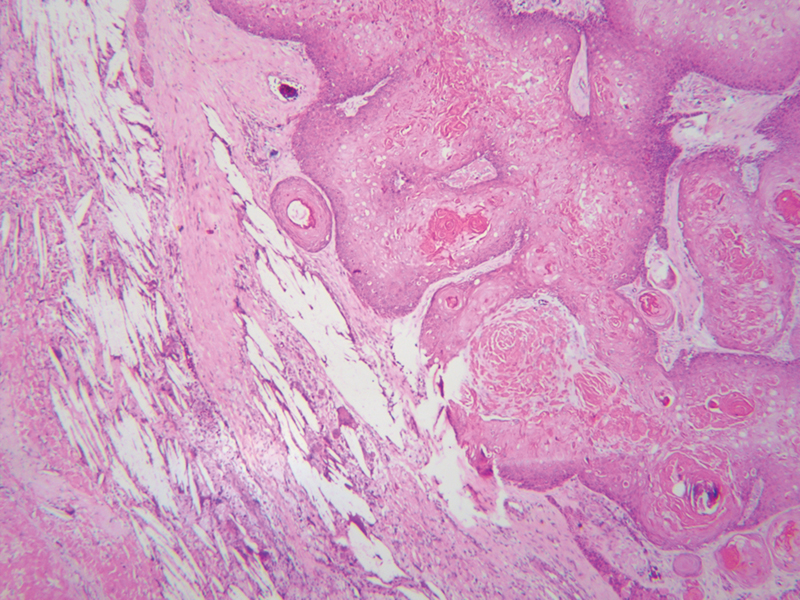
| Fig 6: Variable sized lobules of squamous epithelium undergoing abrupt change into eosinophilic amorphous keratin. The proliferating epithelium shows pushing borders. The lesion is considered a mimic of squamous cell carcinoma (hematoxylin and eosin, ×40).|
| Variable sized lobules of squamous epithelium undergoing abrupt change into eosinophilic amorphous keratin. The proliferating epithelium shows pushing borders. The lesion is considered a mimic of squamous cell carcinoma (hematoxylin and eosin, ×40).|
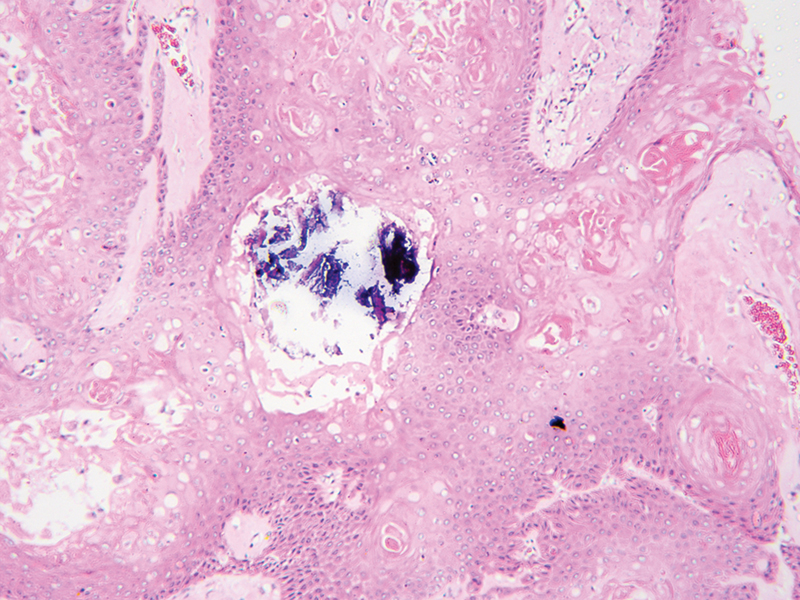
| Fig 7: Areas of calcification, which commonly occur in proliferating pilar tumors.
References
- Jones EW. Proliferating epidermoid cysts. Arch Dermatol 1966; 94 (01) 11-19
- Ye J, Nappi O, Swanson PE, Patterson JW, Wick MR. Proliferating pilar tumors: a clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol 2004; 122 (04) 566-574
- Osto M, Parry N, Rehman R, Ahmed U, Mehregan D. Malignant proliferating trichilemmal tumor of the scalp: a systematic review. Am J Dermatopathol 2021; 43 (12) 851-866
- Joshi TP, Marchand S, Tschen J. Malignant proliferating trichilemmal tumor: a subtle presentation in an African American woman and review of immunohistochemical markers for this rare condition. Cureus 2021; 13 (08) e17289
- Alarcón Pérez CE, Gómez Ángulo D, Olmos Pérez M, Mora Hernández O, Morales SD. Management of 3 proliferating pilar tumors: definition, differential diagnosis, and treatment options. Actas Dermosifiliogr (Engl Ed) 2019; 110 (10) 850-854


 PDF
PDF  Views
Views  Share
Share

