Impact of dental considerations on the quality of life of oral cancer patients
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2014; 35(01): 66-70
DOI: DOI: 10.4103/0971-5851.133724
Abstract
Aim: To evaluate the significance of pre-treatment dental care in oral cancer patients and to assess its impact on the quality of life of these patients. Materials and Methods: The sample size included 50 oral cancer patients who were visiting to a palliative care unit at Jaipur. Assessment was based on thorough case history, complete dental examination. Quality of life was estimated by W.H.O quality of life questionnaire. Result: On analysis, patients of age group 50-59 avoided to prophylactic dental treatment before cancer treatment and therapy. Seventy-eight percent patients experienced worst quality of life after the treatment as a result of dental complications. Out of those 78%, only 2% of patients took preventive dental treatments before the cancer therapy. Conclusion: Dental negligence is still a major cause of worsening of post treatment quality of life of an individual. Therefore, the treating oncologist should always take these considerations seriously to provide quality treatment to the patient.
Publication History
Article published online:
19 July 2021
© 2014. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Aim:
To evaluate the significance of pre-treatment dental care in oral cancer patients and to assess its impact on the quality of life of these patients.
Materials and Methods:
The sample size included 50 oral cancer patients who were visiting to a palliative care unit at Jaipur. Assessment was based on thorough case history, complete dental examination. Quality of life was estimated by W.H.O quality of life questionnaire.
Result:
On analysis, patients of age group 50-59 avoided to prophylactic dental treatment before cancer treatment and therapy. Seventy-eight percent patients experienced worst quality of life after the treatment as a result of dental complications. Out of those 78%, only 2% of patients took preventive dental treatments before the cancer therapy.
Conclusion:
Dental negligence is still a major cause of worsening of post treatment quality of life of an individual. Therefore, the treating oncologist should always take these considerations seriously to provide quality treatment to the patient.
INTRODUCTION
The importance of dental care is often overlooked due to the omission of the dentist as a member of the palliative care team. However, many terminal patients exhibit problems in oral cavity that affects their quality of life. Palliative care dentists must exhibit empathy and compassion, and should be excellent communicators. Dentists can play an important role in alleviating both the physical and psychological pain of dying.[1]
Surgery, chemotherapy and radiotherapy are the options for the treatment of head and neck cancers. These treatments include delivery of high-energy radiation and cytotoxic drugs, which is used to destroy cancer cells and to stop them from multiplying. It may result in both acute and long-term consequences to the oral mucosa, salivary glands, teeth and bone. The most frequently documented source of sepsis in the immunosuppressed cancer patient is the mouth. Therefore, early and definitive dental intervention, including comprehensive oral hygiene measures, reduces the risk for oral and associated systemic complications.[2]
The clinical management of squamous cell carcinoma of the head and neck causes oral sequelae that can compromise patients’ quality of life. There should be a symbiotic relationship in between an oncologist and a dentist to reduce or eliminate the dreadful complications like radiation mucositis, xerostomia, osteoradionecrosis, etc.[3]
A consultation with a dental team experienced in caring for patients undergoing treatment for head and neck cancer should be done before the start of therapy. Many oral conditions, such as poor oral hygiene, broken teeth, defective restorations and periodontal disease, are likely to precipitate complications during and after a course of radiation therapy.[3]
Few reports from developed countries have shown lack of awareness about the various aspects of oral cancer among the public. There is an urgent need to deliver education to the patient as well as family members about the potential role of optimal oral care before, during, and after cancer treatment. There exists an array of acute and long-term effects of the therapy in the oral cavity and the craniofacial complex[4]. So, this study was done with an aim to have an insight about the dentist's role and the impact on the quality of life in an oral cancer patient in a palliative care unit.
MATERIALS AND METHODS
The study was conducted among the out patients with oral cancer visiting to the Palliative care unit during the period of January 2012 to February 2012, to assess the correlation between clinical findings and occurrence of post-treatment dental problems.
Research design and study population
The purpose of research was to assess the importance of dental treatment before undergoing cancer treatment. This is a cross-sectional observational study which comprised of multi-ethnic groups, selected from among those attending our palliative care unit with oral cancer. Fifty patients depicting oral cancer were selected. Proper history regarding pre-treatment (radiotherapy, chemotherapy or surgery, dental considerations and dental treatment) was taken. Thorough examination was done to evaluate oral status along with recording of a quality of life questionnaire.
A formal ethical clearance to conduct this study was obtained by the ethical committee of the institution. Patients selected for the study were explained in detail about the condition affecting their oral cavity and the procedure that they would be subjected to. A written consent was sought from all patients after explanation about the whole procedure in Hindi/local language for better understanding and cooperation.
Inclusion and exclusion criteria
Patients had oral cancer, undergone prior cancer treatment and visiting palliative care unit were included in the study and those patients without oral cancer, patients visiting for the first time, patients who were uncooperative and patients who were not ready for dental check up were excluded from the study.
MATERIALS
The list of materials used in the study were contemporary dental chair with additional illumination facility, a pair of sterile disposable gloves, mouth mask, head cap, stainless steel kidney tray, mouth mirror and straight probe.
Method of collection of data
Data collection included detailed history and clinical examination. The study involved obtaining detailed case history of patients with oral cancer (Case Performa — Annexure 1) with special focus on the factors such as duration of temporomandibular joint (TMJ) problem, previous history of such problem/with treatment at that time, medical history, family history, habits and stress history. Case history was followed by clinical examination of every patient.
Statistical test
All the recorded data were tabulated and statistically analyzed using Statistical Package for the Social Science (SPSS) software {Version-13; SPSS Inc., Chicago, IL, USA}. The data were subjected to descriptive analysis for mean, standard deviation and standard error of mean. The P value of 0.05 or less was considered significant.
RESULTS
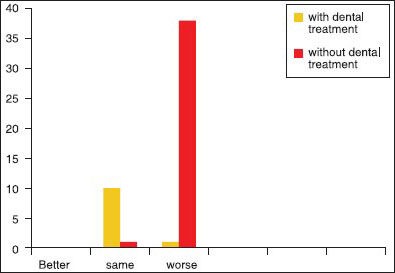
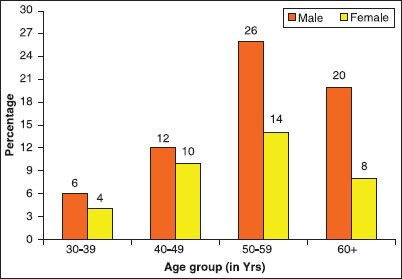
A total of 50 oral cancer patients were investigated that included 32 males and 18 females patients [Graph 1] with a mean age of male patients was 54.6 year old and the mean age of female patients was 49.7 years. Out of 50 patients, 49 (i.e. 98%) had some form of deleterious habits. Only 1 patient (i.e. 2%) patient was not associated with any kind of habit [Graph 2].
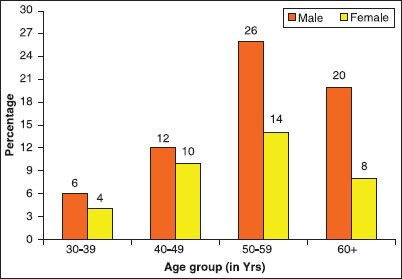
| Figure 1:Distribution according to age and sex of the patients
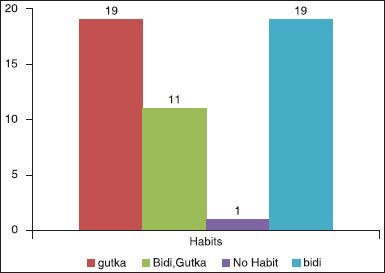
| Figure 2:Distribution of associated habit of the patients
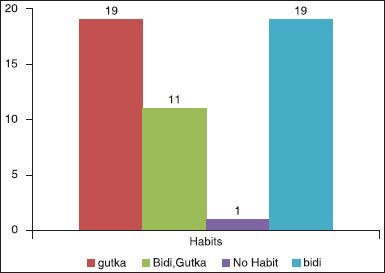
Only 12 patients out of 50 had taken prior dental considerations before undergoing the radiotherapy as well as surgery [Graph 3]. Out of those, 38 patients (74%) had sensitivity and 50% had limited mouth opening. Attrition was the common problem present between both groups [Graph 4].
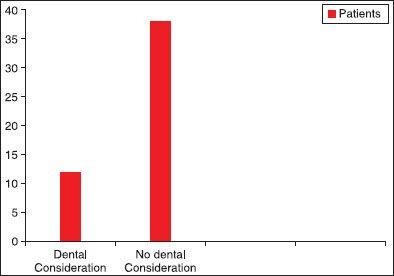
| Figure 3:Distribution of dental consideration of the patients
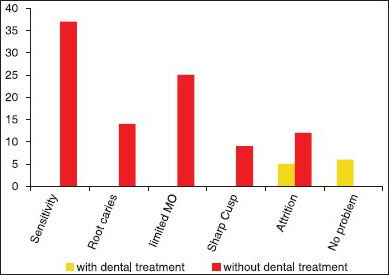
| Figure 4:Distribution of prevalence of dental problems after oral cancer treatment
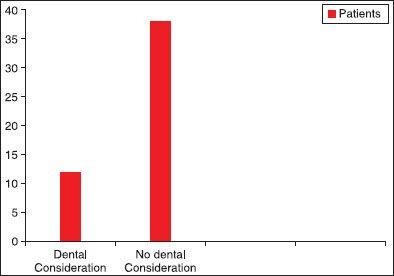
Severe degradation of the QOL was observed in most of the patients. Seventy-eight percent patients had worse quality of life experience out of that only 2% had dental consideration [Graph 5].
| Figure 5:Distribution of quality of life of the patients according to dental consideration
DISCUSSION
It has been well recognized since the beginning of this century that oral cancer is one of the most common cancers in the world. The incidence from the National Cancer Registry Project (Indian Council of Medical Research) confirmed the fact that oral cancer was indeed a common form of cancer in India.
Although palliative care for the terminally ill is based on a multidimensional philosophy to provide whole-person comfort care while maintaining optimal function, it does not usually include dentistry in its team approach. Dentists can have a significant role in the care of these patients by providing total, active comfort care of the oral cavity. Alleviation of pain and prevention of infection in the oral cavity should be a priority of the dentist. Routine assessments and interventions by a dentist in the palliative care team, including psychological comfort, diagnosis of dental conditions and treatments like maintenance of oral hygiene, excavation of dental caries and periodontal problems, fulfillment of prosthetic needs and instructions for proper hydration of the oral mucosa lead to a less stressful event of cancer treatment for a particular patient.[4] Attention to such detail may reduce not only the microbial load of the mouth but the risk for pain and oral infection as well. This multidisciplinary approach to palliative care, including a dentist, may reduce the oral debilities that influence the patient's ability to speak, eat or swallow.[5] Oral cavity can be a mirror of the overall health of an individual. Therefore, dental expression in palliative care may be defined as the extended dental services with a central goal of providing pre-eminent feasible oral care to terminally-ill or far-advanced disease patients.[6]
This study was done to know whether there is any correlation between the importance of dental treatment before treating oral cancer. The study was conducted on 50 subjects and results were tabulated.
Oral cancer is the most common cancer in India accounting for 50-70% of total cancer mortality. Though it is more common in males, the rate is increasing in females.[7] In our study, the majority (64%) of the patients were males. Only 32% were females. Similar sex distribution has been reported by many authors.[8] Analyzing the results, male predilection was seen, which was statistically significant and in agreement with Sherin et al.[5] In a study by Patel et al,[6] in Surat, Gujarat, 75% of the patients were males. Mehrotra et al.[7] from Allahabad reported a male:female ratio of 3.27:1. Iype et al.[8] from Trivandrum, Kerala, found a higher preponderance in males (70%) compared to females (30%). Wahid et al.[9] from Abottabad, Pakistan, found 60% males and 40%-females. Durazzo et al.[10] from Brazil reported 31.8%-cases were females.
The mean age at presentation in our study was 57 years. The maximum number of patients was in the age range of 50-59 years. The youngest patient in our study was 30 years old. Only 5% of the patients were less than 40-years of age. Patel et al.[4] reported 12.9%-of oral and oropharyngeal malignancies were below 35 years of age, 23.8%-between 35 and 45, and 63.3%-cases over 45 years of age. In a study by Mehrotra et al.,[7] the maximum incidence was in the 50-59 years of age range. According to Wahid et al.,[5] in Pakistan, the most common age group affected in oral cavity squamous cell carcinoma was 41-50 years (38%), followed by 51-60 years (34%). In a study by Durazzo et al.[10] the mean age was 57.4 years. Only 8.6 %-of the patients were 40-years or less. The increasing incidence of these cancers in the younger age group can be correlated to the trend of tobacco and alcohol consumption in the young population.
In our study, out of a total of 50 patients, 58%-patients were smokers. Fifty-two percent were consuming smokeless tobacco in the form of pan or gutkha. Forty-four percent were using tobacco, either smoking or chewing. Smoking was seen only in males. None of the females were smoking because of cultural taboos. Tobacco chewing was found in 25 out of 32 female patients in our study.
In a study by Iype et al.,[8] 56.4%-of the patients were habituated to either tobacco chewing, smoking or alcohol. In the study of Durazzo et al.,[10] tobacco smoking was identified in 80.8%-of the patients. Alcohol consumption history was retrieved in 56.6%-of the patients.
In the present study, dental treatment was not done in 76%-of the patients visiting palliative care unit who had already undergone cancer treatment. Prevalence of sensitivity (74%) and limited mouth opening (50%) was the prevalent findings which could complicate the further treatment if required.
Najafi[11] et al. showed that abnormalities are probably caused by the type, intensity and frequency of treatment and the age of the patients at the time of radiotherapy, which might have important consequences on the children's dental development and also suggested patients that experience cancer treatment are faced with difficult oral health issues before, during and post cancer therapy. In our study, only 2% had prior dental consideration that can be one of the reasons for the 78% patients who experienced worse quality of life.
Palliative dental care should be fundamental in management of patients with active, progressive and far-advanced disease in which the oral cavity has been compromised either by the disease directly or by its treatment. The focus of care is quality of life.[12] Cancer therapies — including surgery, radiation and chemotherapy may unfavorably affect the oral/dental health of patients. Existing dental problems can also result in serious complications that may be prevented by dental intervention prior to cancer therapy.[13] Most cancer patients experience uncontrollable pain that creates a poor quality of life and limits normal function. Oral cancer is unique in that it causes intense pain at the primary site and significantly impairs speech, swallowing, and masticatory functions.[14] The overall five-year survival rate for oral cancer patients is 60%. With the improved survival rate, there is an increase in the burden of pain. Therefore, oral cancer management requires palliative care to address cancer-associated symptoms. Effective palliative care lies in accurate characterization of symptoms, which requires careful analysis of the available quality-of-life studies.
Oral cancer present with significant dental disease prior to radiation therapy. If left unattended diseased dentition may cause serious dental infections after therapy. As a result, pre-radiation dental evaluation has become an integral part of care offered to those patient about to receive cancericidal doses of radiation for head and neck tumors.[15]
When a patient presents with a diagnosis of cancer, he is unlikely to consider the oral implications as a high priority. However, it is important that patients and caregivers are counseled about oral care procedures and their implications of the proposed treatment.[16] The time period between diagnosis of cancer and commencement of treatment is usually short. Ideally, a comprehensive oral evaluation should take place 1 month before cancer treatment starts. It allows adequate time for recovery from any required invasive dental procedures.[17] The pre-treatment evaluation includes a thorough examination of hard and soft tissues, as well as appropriate radiographs to detect possible sources of infection and pathology. Teeth indirect association with the tumor, in the direct path of the radiation beam or teeth with doubtful prognosis (deep caries, deep periodontal pockets, non-vital teeth) should be extracted as soon as possible before radiotherapy, ideally to allow 3 weeks for maximal healing time before radiotherapy.[18] In palliative medicine, an interdisciplinary approach is essential and the importance of dental care is often overlooked due to the omission of dentist as a member of palliative care team. therefore, knowledge and awareness for oral care in cancer patients is mandatory.[19]
Diet counseling holds paramount significance to combat taste changes and ensure oral comfort for patients.
CONCLUSION
Treatment of head and neck cancers still remains a big challenge for the oncologists and dental professionals as well. However, the advent of various advancements has reduced the percentage of complications, but it's a complex and dynamic patho-biological process that hampers the quality of life and leads to physiological and psychological distress in a patient. Therefore, a dentist's role should be anticipated and should always be included in the palliative care unit to avoid further complications and to improve the quality of life of the patient.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- WisemanMA. Palliative care dentistry. Gerodontology 2000;17:49-51.
- Scully C, Epstein JB. Oral health care for the cancer patient. Eur J Cancer B Oral Oncol 1996;32:281-92
- Hancock PJ, Epstein JB, Sadler GR. Oral and dental management related to radiation therapy for head and neck cancer. J Can Dent Assoc 2003;69:585-90.
- Paunovich ED, Aubertin MA, Saunders MJ, Prange M. The role of dentistry in palliative care of the head and neck cancer patient.Tex Dent J 2000;117:36-45.
- Sherin N, Simi T, Shameena P, Sudha S. Changing trends in oral cancer.Indian JCancer 2008;45:93-6.
- Patel MM, Pandya AN. Relationship of oral cancer with age, sex, site distribution and habits. Indian J Pathol Microbiol 2004;47:195-7.
- Mehrotra R, Singh M, Kumar D, Pandey AN, Gupta RK, Sinha US. Age specific incidence rate and pathological spectrum of oral cancer in Allahabad. Indian J Med Sci 2003;57:400-4.
- Iype EM, Pandey M, Mathew A, Thomas G, Sebastian P, Nair MK. Oral cancer among patients under the age of 35 years. J Postgrad Med 2001;47:171-6.
- Wahid A, Ahmad S, Sajjad M. Pattern of carcinoma of oral cavity reporting at dental department of Ayub medical college. J Ayub Med Coll Abbottabad 2005;17:65-6.
- Durazzo MD, de Araujo CE, BrandãoNetoJde S, Potenza Ade S, Costa P, Takeda F, et al. Clinical and epidemiological features of oral cancer in a medical school teaching hospital from 1994 to 2002: Increasing incidence in women, predominance of advanced local disease, and low incidence of neck metastases. Clinics (Sao Paulo) 2005;60:293-8.
- Najafi Sh, Tohidastakrad Z, Momenbeitollahi J. The Long-Term Effects of Chemo Radiotherapy on Oral Health and Dental Development in Childhood Cancer. J Dent 2011;8:39-43.
- Saini R, Marawar P, Shete S, Saini S, Mani A. Dental Expression and Role in Palliative Treatment. Indian J Palliat Care 2009;15:26-9.
- Barker BF, Barker GJ. Oral management of the patient with cancer in the head and neck region. J Calif Dent Assoc 2001;29:619-23.
- Viet CT, Schmidt BL. Biologic Mechanisms of OralCancer Pain and Implicationsfor Clinical Therapy. J Dent Res 2012;91: 447-53.
- Sennhenn-Kirchner S, Freund F, Grundmann S, Martin A, Borg-von Zepelin M, Christiansen H, et al. Dental therapy before and after radiotherapy - an evaluation on patients with head and neck malignancies. Clin Oral Investig 2009;13:157-64.
- Escoda-Francolí J, Rodríguez-Rodríguez A, Pérez-García S, Gargallo-Albiol J, Gay-Escoda C. Dental implications in oral cancer patients. Med Oral Patol Oral Cir Bucal 2011;16:508-13.
- The Oral Management of Oncology Patients Requiring Radiotherapy, Chemotherapyand/or Bone Marrow Transplantation Clinical Guidelines: Updated 2012. The Royal College of Surgeons of England/The British Society for Disability and Oral Health. Available from: www.bsdh.org.uk/guidelines/oncolradio [Last accessed on 2014 Feb 13].
- Makkonen TA, Kiminki A, Makkonen TK, Nordman E. Dental extractions in relation to radiation therapy of 224 patients. Int J Oral Maxillofac Surg 1987;16:56-64.
- SainR i, SainiS, Sugandh RS. Knowledge and awareness of palliative medicine amongst students of a rural dental college in India. Int J Appl Basic Med Res. 2011;1:48-9.
| Figure 1:Distribution according to age and sex of the patients
| Figure 2:Distribution of associated habit of the patients
| Figure 3:Distribution of dental consideration of the patients
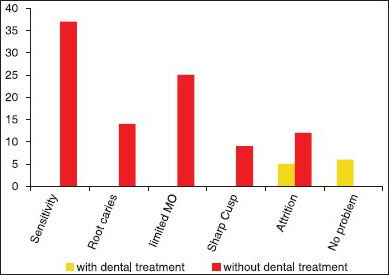
| Figure 4:Distribution of prevalence of dental problems after oral cancer treatment
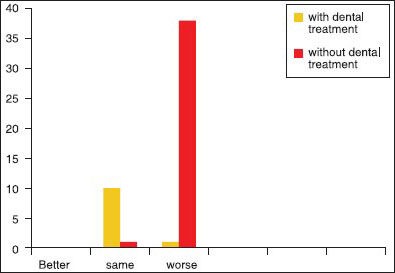
| Figure 5:Distribution of quality of life of the patients according to dental consideration
References
- WisemanMA. Palliative care dentistry. Gerodontology 2000;17:49-51.
- Scully C, Epstein JB. Oral health care for the cancer patient. Eur J Cancer B Oral Oncol 1996;32:281-92
- Hancock PJ, Epstein JB, Sadler GR. Oral and dental management related to radiation therapy for head and neck cancer. J Can Dent Assoc 2003;69:585-90.
- Paunovich ED, Aubertin MA, Saunders MJ, Prange M. The role of dentistry in palliative care of the head and neck cancer patient.Tex Dent J 2000;117:36-45.
- Sherin N, Simi T, Shameena P, Sudha S. Changing trends in oral cancer.Indian JCancer 2008;45:93-6.
- Patel MM, Pandya AN. Relationship of oral cancer with age, sex, site distribution and habits. Indian J Pathol Microbiol 2004;47:195-7.
- Mehrotra R, Singh M, Kumar D, Pandey AN, Gupta RK, Sinha US. Age specific incidence rate and pathological spectrum of oral cancer in Allahabad. Indian J Med Sci 2003;57:400-4.
- Iype EM, Pandey M, Mathew A, Thomas G, Sebastian P, Nair MK. Oral cancer among patients under the age of 35 years. J Postgrad Med 2001;47:171-6.
- Wahid A, Ahmad S, Sajjad M. Pattern of carcinoma of oral cavity reporting at dental department of Ayub medical college. J Ayub Med Coll Abbottabad 2005;17:65-6.
- Durazzo MD, de Araujo CE, BrandãoNetoJde S, Potenza Ade S, Costa P, Takeda F, et al. Clinical and epidemiological features of oral cancer in a medical school teaching hospital from 1994 to 2002: Increasing incidence in women, predominance of advanced local disease, and low incidence of neck metastases. Clinics (Sao Paulo) 2005;60:293-8.
- Najafi Sh, Tohidastakrad Z, Momenbeitollahi J. The Long-Term Effects of Chemo Radiotherapy on Oral Health and Dental Development in Childhood Cancer. J Dent 2011;8:39-43.
- Saini R, Marawar P, Shete S, Saini S, Mani A. Dental Expression and Role in Palliative Treatment. Indian J Palliat Care 2009;15:26-9.
- Barker BF, Barker GJ. Oral management of the patient with cancer in the head and neck region. J Calif Dent Assoc 2001;29:619-23.
- Viet CT, Schmidt BL. Biologic Mechanisms of OralCancer Pain and Implicationsfor Clinical Therapy. J Dent Res 2012;91: 447-53.
- Sennhenn-Kirchner S, Freund F, Grundmann S, Martin A, Borg-von Zepelin M, Christiansen H, et al. Dental therapy before and after radiotherapy - an evaluation on patients with head and neck malignancies. Clin Oral Investig 2009;13:157-64.
- Escoda-Francolí J, Rodríguez-Rodríguez A, Pérez-García S, Gargallo-Albiol J, Gay-Escoda C. Dental implications in oral cancer patients. Med Oral Patol Oral Cir Bucal 2011;16:508-13.
- The Oral Management of Oncology Patients Requiring Radiotherapy, Chemotherapyand/or Bone Marrow Transplantation Clinical Guidelines: Updated 2012. The Royal College of Surgeons of England/The British Society for Disability and Oral Health. Available from: www.bsdh.org.uk/guidelines/oncolradio [Last accessed on 2014 Feb 13].
- Makkonen TA, Kiminki A, Makkonen TK, Nordman E. Dental extractions in relation to radiation therapy of 224 patients. Int J Oral Maxillofac Surg 1987;16:56-64.
- SainR i, SainiS, Sugandh RS. Knowledge and awareness of palliative medicine amongst students of a rural dental college in India. Int J Appl Basic Med Res. 2011;1:48-9.


 PDF
PDF  Views
Views  Share
Share

