Imaging Recommendations for Diagnosis, Staging, and Management of Breast Cancer
CC BY 4.0 · Indian J Med Paediatr Oncol 2023; 44(02): 207-228
DOI: DOI: 10.1055/s-0042-1760326
Abstract
In a rapidly evolving world, with a steep rise in breast cancer incidence, there has been many advances in imaging and therapeutic options of breast cancer care. In this review article, we are trying to cover imaging guideline for cancer detection and their therapeutic options. These help in the reduction of morbidity and mortality.
Publication History
Article published online:
04 May 2023
© 2023. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
In a rapidly evolving world, with a steep rise in breast cancer incidence, there has been many advances in imaging and therapeutic options of breast cancer care. In this review article, we are trying to cover imaging guideline for cancer detection and their therapeutic options. These help in the reduction of morbidity and mortality.
Keywords
breast cancer - early detection - imaging guidelinesIntroduction
According to latest GLOBOCAN statistics,[1] breast cancer (BC) is the leading cause of mortality amongst all cancers. Early detection of BC improves survival. There are various societies like JCC, NCCN, ASCO, ACR, RSNA, ESR, IRIA/ICRI, National Cancer Grid (NCG) which have their guidelines for the evaluation and treatment of BC. Here in this review, we are aiming to cover imaging guidelines for the evaluation of BC.
Epidemiology, Clinical presentation in India and Globally
Globally, BC is the leading cancer among women, contributing to 2,261,419 new cases and 684,996 deaths annually.[1] There is a wide variation in incidence rates, with some countries like Netherlands and Belgium having estimated age adjusted incidence (AAI) of over 100 and others like Bhutan with AAI of 5.[2] Globally, both incidence and mortality of BC have increased significantly in all age groups since 1990. Mortality increased by 0.23%-per year and incidence by 1.28%-per year in age group of 50 to 69 and by 1.55%-per year (under 50).[3] BC is the most common cancer among Indian women both in terms of incidence and mortality. There are estimated 178,361 (13.5%-cancers among women) cases and 90,408 (10.6%) deaths due to BC in India.[3]
The AAI is 25.8 in India overall, with the highest burden being observed in metropolitan cities. Around 57%-of BCs are diagnosed at the locally advanced stage.[4]
Risk Factors and Etiopathogenesis
Cancer, in general, is a multistep process and after decades of studies we are now aware that there are three types of risk factors: (1) exogenous modifiable risk factors like oncogenic viruses, tobacco usage, atmospheric radiation, chemical carcinogens, lack of exercise, obesity, low activity level, etc.; (2) endogenous partially modifiable risk factors like hereditary risk, hormones, inflammation, growth factors, and (3) intrinsic risk factors which are non-modifiable and created due to random errors in DNA replication.[5] The later may be responsible for over 60%-of tissue cancer burden.[5] If a cause is known, it is much easier to know whether it can (e.g., tobacco use) or cannot (e.g., ionizing radiation in the atmosphere) be avoided easily.[6] These factors then result in uncontrolled growth and the etiopathogenesis of cancer is summarized in [Fig. 1].
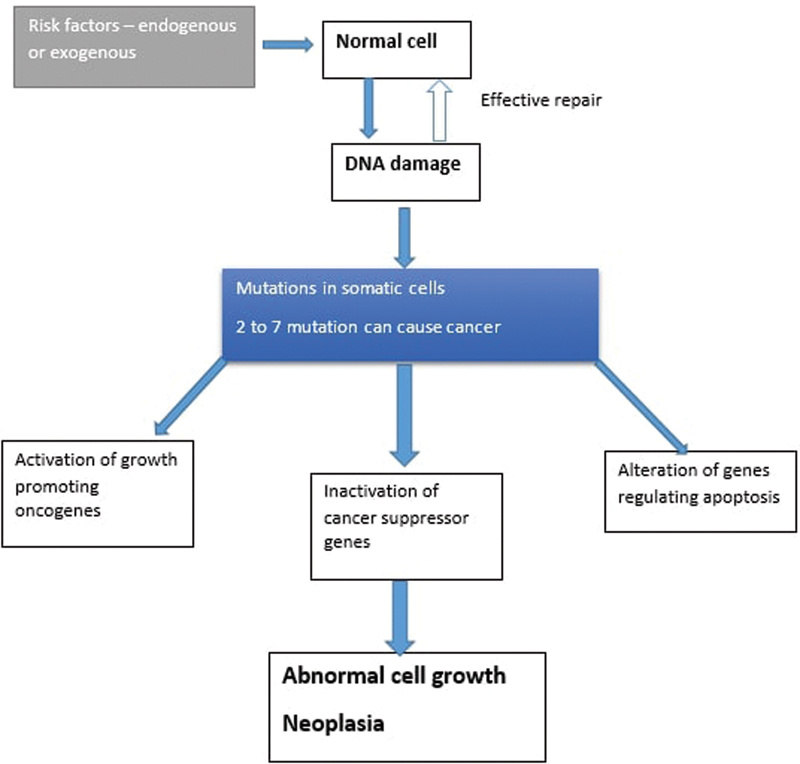
| Fig. 1 :Etiopathogenesis of cancer.
Various specific risk factors for BC are as follows.
Non-modifiable risk factors are the one which cannot be changed. These are increasing age, genetic mutations (BRCA1, BRCA 2, and p53), early menarche, late menopause, dense breast, family and personal history of BC, history of radiation to chest wall, and exposure to certain drugs like diethylstilbestrol used to prevent abortion till 1970s.
Modifiable risk factors are obesity, lack of exercise, hormones in the form of HRT and contraceptive pills, late pregnancy, avoiding breastfeeding and alcohol consumption.[7]
Clinical/Diagnostic Work-Up
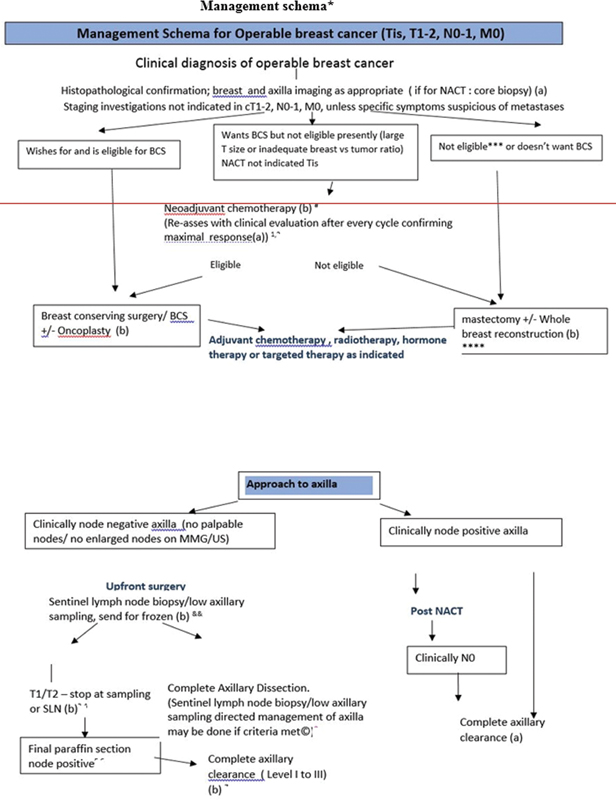
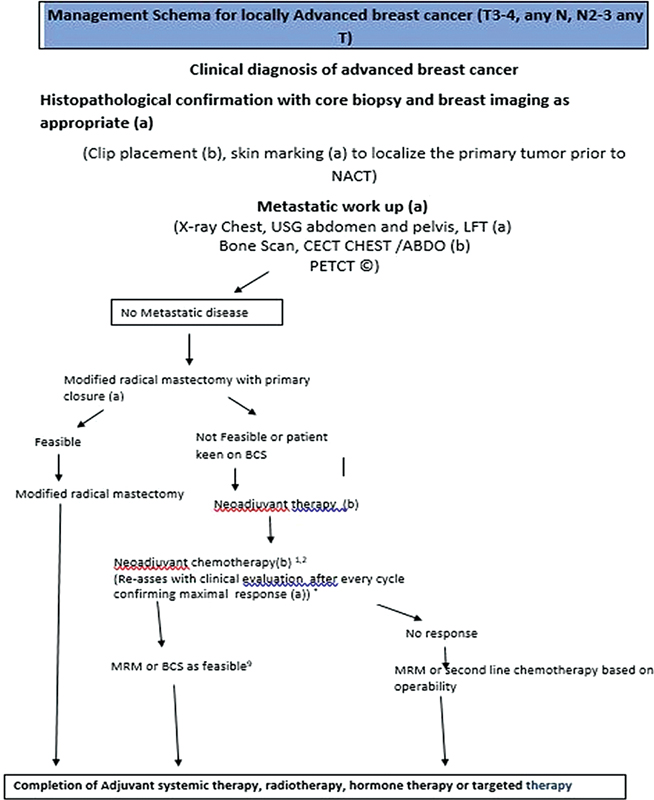
The triad of diagnosis of BC involves a good history taking or symptom evaluation and thorough clinical examination of both breasts, axillae and supraclavicular fossae and systemic examination, if necessary. This is followed by imaging to ascertain the risk of harboring malignancy.[8] BC is clinically classified into operable (T1–2, N0–1, M0) (OBC), locally advanced (T3–4, N2–3, M0) (LABC), and metastatic BCs (T any N any M1).[9] [10] This clinical classification helps in deciding the need of metastatic work-up versus not. Since <5>
Imaging Recommendations for Diagnosis, Staging, and Management of BC
Screening mammography has resulted in the increase in the detection of early BC. Various screening guidelines are in place, which are specific to countries and societies. These guidelines vary for women with average and high risk of BC. Discussing guidelines for screening is out of scope of this article. These are discussed in depth in Annexure 1.
Screening
Mammography from the age of 40 years is recommended for women at average risk of developing BC.[11] [12] The upper age limit for screening mammography should ideally be when a woman's life expectancy exceeds 5 to 7 years so that the benefits of screening could be fully realized[11] and an age limit of 70 years may be deemed appropriate.[12] [13] Ultrasound can be used as an adjunct to screening mammography for women with dense breasts, but is not recommended as a standalone screening test.[14] For women with a lifetime risk of BC ≥20%-according to risk assessment tools, with known BRCA1 and BRCA2 mutation or with a first degree relative to the mutation, with radiation therapy (RT) to the chest between ages of 10 and 30 years, screening can be started earlier.[14] Annual mammography and contrast-enhanced magnetic resonance imaging of breasts (CEMRI) are recommended starting at 30 years of age or 10 years before the age of diagnosis of first-degree relative with BC, whichever is later. Women with RT to chest can start screening 8 years after RT. However, screening mammography is not recommended before the age of 25 years.[11] [14] Only MRI screening is advisable for women with Li-fraumeni syndrome and A-T homozygotes.[15]
Diagnosis
Ultrasound is the modality of choice for women less than 30 years of age as well as pregnant and lactating women.[16] Symptomatic women above the age of 40 years benefit from a combination of mammography and ultrasound. Between the ages of 30 and 39 years the initial investigation of ultrasound could be followed by mammography, if required. However in the presence of strong clinical suspicion of BC, a combination of mammography and ultrasound can be performed at the outset in this group.[12] [17] All women diagnosed with BC should have mammography irrespective of their age.[17] Digital breast tomosynthesis has shown improved cancer detection rate as compared with digital mammogram alone.[18] CEMRI (contrast-enhanced MRI) is indicated if there is a discrepancy in clinical and radiological findings, if breast conservation is considered with a diagnosed lobular cancer, for tumors occult on mammography, in cases of Paget's disease of the nipple if breast conservation is contemplated, if conventional imaging is suspicious for but does not confirm multifocal/multicentric disease, in cases of occult primary breast cancer such as proven metastatic axillary nodes without primary detected on mammogram and USG.[12] [17] A recognized reporting system like the American College of Radiology (ACR) Breast Imaging – Reporting and Data System (BI-RADS) should be used to report the radiological investigations. Image-guided biopsy of lesions suspicious for malignancy (BI-RADS 4) or highly suggestive of malignancy (BI-RADS 5) is advised. Probably benign (BI-RADS 3) lesions may also be biopsied if another malignant mass is detected in either breast.[19] [20] [21]
Women presenting with breast symptoms should undergo triple assessment with clinical examination, breast imaging, and histopathology.[22] Fourteen gauge core biopsy with an automated spring-loaded biopsy device under ultrasound guidance is advised for histological diagnosis in both screening and symptomatic setting.[23] Stereotactic biopsy under mammography guidance is advised for abnormalities visualized on mammography but not on ultrasound. Suspicious lesions demonstrated only on MRI should be subjected to a second-look ultrasound. If no correlating abnormality is visualized, these MRI-only lesions should be subjected to MRI-guided biopsy.[24] [25] CEMRI is not an alternative to biopsy as it does not provide tissue diagnosis. MRI-guided vacuum-assisted breast biopsy (VABB) is performed for MRI-only lesions, whereas stereotactic VABB is performed for abnormalities seen on mammography only.[26] VABB uses a suction system, which allows a larger tissue sample to be obtained from a single insertion. Certain imaging modalities demonstrate certain abnormalities better. For example small clusters of microcalcifications are well demonstrated on mammography whereas small intraductal masses are well seen on breast ultrasound.
Contrast-enhanced mammogram (CEM) is a relatively new imaging investigation which is fast getting popularity due to its shorter imaging time and low cost as compared with MRI. Iodinated contrast is used and images are obtained based on dual energy imaging. Evaluation of CEM is performed on subtracted post-processed images.[27] CEM is used to evaluate abnormality seen on mammogram such as asymmetry, architectural distortion, mass, calcification, etc. It is also used for detecting and evaluating additional abnormalities in ipsilateral or contralateral breast.[27]
Imaging Appearance of Various Types of Cancer
BCs are broadly divided in four categories depending on IHC (immune histochemical) marker status. These are Luminal A (ER + , PR + , Her2/Neu -), Luminal B (ER + , PR + , Her2/Neu + or ER + , PR + , any Her2/Neu with High Ki67), Her2/Neu enriched (ER-, PR-, Her2/Neu +) and TNBC (Triple Negative BC) (ER-, PR-, Her2/Neu -). This classification is for the treatment and prognostication of patient.[28] However, radiologically there are certain differences in imaging appearances of these common invasive cancers. Luminal cancers commonly have spiculated mass, whereas Her2/Neu-enriched tumors have mass with indistinct margin. Calcifications are more commonly associated with Her2-enriched tumors. TNBCs are more commonly associated with distinct well-defined edges.[29] [30] Details about different types of invasive and preinvasive cancer and its imaging appearance on various modalities are out of scope of this article.
In patients with reconstructed breast, imaging appearance of cancer is similar. However, additional care must be taken for imaging as well as interpretation as in cases of breast implants, additional, implant displaced views must be obtained. While evaluating cases of breast reconstruction with flaps or oncoplasty, fat necrosis is a common occurrence, and care must be taken to differentiate it from recurrence. Many times comparison with prior imaging is problem solving.
Staging
For T1 or T2, N0 or N1, M0, BCs which constitute up to T2N1M0 of stage 2B ([Fig. 2]) of anatomical staging as per the eighth edition of AJCC Cancer Staging Manual of the American College of Surgeons,[10] staging investigations to detect occult distant metastasis is not advised due to the low yield of these investigations as well as false positive studies that follow. However suspicious findings in clinical history, clinical examination, abnormal serological tests for liver or bone function may necessitate staging investigations in this cohort of patients[31] From T3N0M0 of stage 2B of AJCC staging, including T3–4anyN and N2–3anyT cancers, the preferred tests are contrast-enhanced computed tomography (CECT) chest and abdomen and Tc99m-methylene diphosphonate bone scan ([Fig. 3]).
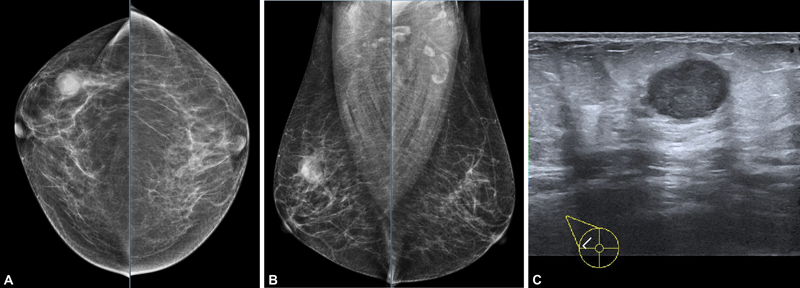
| Figure 2:A 50-year-old female with right breast lump since 1 month. No other complains. On mammogram (A and B) and USG: a well-defined high-density mass with partly obscured margins is seen in the upper outer quadrant of right breast, measuring approximately 1.9 × 2.2 × 2.3 cm. No suspicious microcalcifications are seen. No other associated features are seen. On USG (C) irregular mass with microlobulated margin is seen at 10 o'clock position in right breast. The lesion is predominantly hypoechoic with posterior acoustic enhancement. The lesion is parallel in orientation. No suspicious axillary lymph nodes are seen on imaging. Histopathology of lesion is TNBC. As this lesion is early stage breast cancer without nodal involvement (stage IIA), further metastatic work-up is not needed. (TNBC, triple-negative breast cancer; USG, ultrasonography).
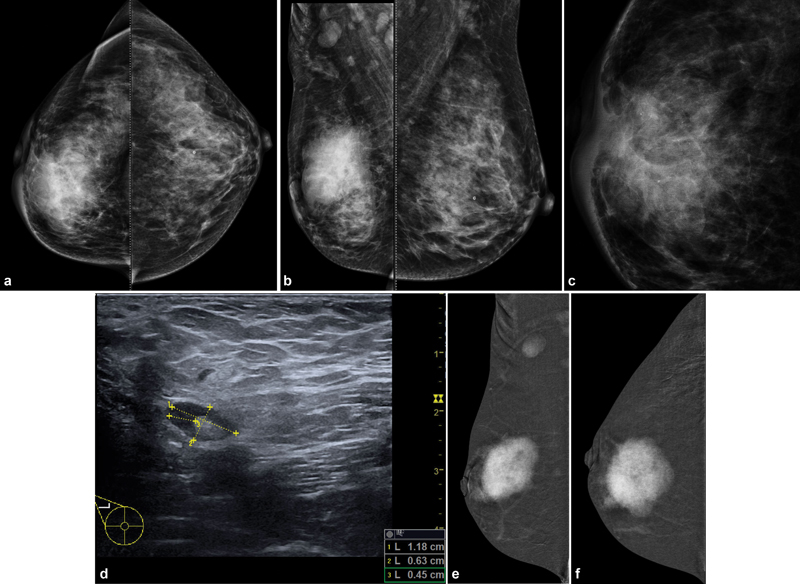
| Figure 3:A 38-year-old female with increasing right breast lump since 15 months. Mammogram (A, B): An irregular high-density mass with indistinct margins is seen in predominantly upper inner quadrant also extending in the outer quadrant measuring approximately 4.4 × 4.4 × 5.5 cm. Pleomorphic microcalcifications (C) are seen within the mass, better seen on magnification view. Diffuse trabecular thickening with nipple areolar complex thickening and retraction is seen. Few suspicious right axillary nodes are seen, largest measuring 1.2 × 0.7 cm with 4.5-mm cortical thickness (D). In view of dense breast parenchyma, further evaluation with CEM was performed to rule out any other lesion in breast, CEM (E, F) is suggestive of large unifocal lesion. This is the case of locally advanced breast cancer (stage IIIA), further metastatic work-up was performed. On CT scan, (G, H) heterogeneously enhancing mass is seen involving right breast with involvement of overlying skin. Enlarged right axillary, right internal mammary, and right supraclavicular lymph nodes are seen. (CEM, contrast-enhanced mammogram.)
Positron emission tomography-computed tomography (PET-CT) is not routinely advised for early stage BC, however, according to NCCN guidelines, it may be advised for higher stage disease if available due to its higher detection of metastatic sites and its whole body coverage.[32] It may be beneficial in inflammatory BC or in oligometastatic disease to confirm absence of metastasis elsewhere in the body if radical treatment is considered for a single involved site.[17] [31] [33] [34]
The clinical and pathological prognostic stage groups may be different from the patient's anatomical stage group. For example, T1N0M0 tumor of anatomical stage group 1A would be pathological prognostic stage group IA if it is grade I tumor which is ER, PR, and HER2 receptor positive. However, if it is grade II ER, PR, and HER2 receptor negative it would change to pathological prognostic stage group IB.[31]
Clinical nodal (cN) category as per AJCC is based on clinical and imaging investigation of nodal basin. Axillary lymph node level depends on the location of lymph node with respect to pectoralis minor muscle. Level I lymph nodes are located lateral to the lateral margin of pectoralis minor muscle; level II lymph nodes are located between lateral and medial margins of the pectoralis minor muscle. Level II also includes interpectoral lymph nodes (Rotter's node). Level III includes lymph nodes that are located medial to medial margin of pectoralis minor muscle.[35] [36]
Suspicious imaging features for axillary lymph nodes on ultrasound are focal eccentric cortical thickness, irregular margin, loss of fatty hilum, and extra nodal extension. Uniformly thin cortex with cortical thickness of less than 3 mm is considered to be normal appearance of axillary lymph node.[37] [38] Metastatic disease is most commonly seen in bones, lungs, brain, and liver.[35] Additional brain imaging is performed for clinical symptoms like headache, mental status alteration, nausea, or vomiting. In such situation brain MRI is preferred over CT scan.[39]
Response Assessment Post NACT
Baseline and end of treatment mammography and ultrasound are the minimum imaging required for the assessment of response to neoadjuvant treatment. However, baseline and end of treatment CEMRI is the ideal modality to assess response.[17] [34] Recent studies have also shown comparable results with the use of CEM for response assessment.[40] Marker clip insertion is advised to mark the tumor bed for reliable identification if there is a radiologic complete response. This is especially important if the breast conservation surgery is planned. It can be placed at the time of initial biopsy or during the first few cycles of treatment if a substantial response is noted.[41] A tissue marker may also be inserted into the biopsied axillary lymph node if local policy includes image-guided localization of the biopsied lymph node and targeted lymph node dissection.[17] Depending on the molecular subtype, response rates of different types BC vary, for e.g., pCR (pathological complete response) is seen in approximately 30%-of the patients with triple negative BC, whereas some newer targeted therapies in Her2 positive cancer are able to achieve pCR rate of up to 60%.-Hormone receptor positive cancers have lowest pCR rate in range of approximately 20%. As per NCCN guidelines, response assessment should be performed on the modality on which prechemotherapy assessment is performed.[42]
In advanced cases with metastatic or oligometastatic disease, response is to be assessed objectively using acceptable criteria of RECIST guidelines. Preferably imaging on which metastatic disease is detected, should be the modality to assess response, like abnormality seen on CT thorax, should be monitored with CT thorax[32]. Multiple studies have shown promising result with the use of serial PET CT in response assessment in metastatic setting.[43] [44]
In non-metastatic setting, clinical examination and imaging studies should be routinely performed during preoperative therapy.[32]
Imaging Guidance for Surgery of Impalpable Malignant Lesions
Ultrasound is the modality of choice for preoperative-guided hook wire localization of nonpalpable masses.[24] Hook wire localization is performed prior to the surgery on the day of surgery. If lesions are not visualized on ultrasound, mammography and MR-guided localizations can be performed for lesions seen on mammography and MR-only lesions, respectively.[25] Radiograph or ultrasound of the excised surgical specimen is advised to confirm total excision of the abnormality. Confirmation of enhancement seen on MRI at the time of localization and follow-up MRI is performed for MRI-only abnormality. Radioactive seeds, magnetic seeds, and electromagnetic-radiofrequency tags can be used as alternatives for hook wire localizations.[45] [46]
Imaging Follow-Up
Annual mammography is recommended after the completion of treatment.[22] It is known that women with mammography detected cancers have better survival rates than clinically detected cancers.[17] Comparison with previous mammograms and biopsy of any new lesion not typically benign are advised.[34] MRI is emerging as a valuable tool in surveillance of patients with BC and has shown clear benefit in differentiating scar tissue from tumor recurrence.[47] [48]
Post-treatment changes in the form of fat necrosis and calcification are commonly seen on mammogram. These changes are commonly seen at the site of surgical suture and need to be carefully evaluated, if suspicious biopsy can be performed. Calcification due to fat necrosis in early stage may mimic suspicious morphology.[49]
If clinically asymptomatic, annual mammography screening should be initiated 6 to 12 months after the completion of radiotherapy.[32]
Supplementary ultrasound may be used. However, breast ultrasound alone is not recommended for routine surveillance.[17] In case of breast reconstruction, routine imaging follow-up for metastasis is not indicated.[32]
In cases of reconstruction with implant, unless there is a clinical concern, routine surveillance systemic imaging to detect metastases is not recommended.[34] There is no significant difference in imaging appearance of locoregional or distant recurrence disease. For follow-up of known visceral metastatic disease from a primary BC, CECT of thorax, abdomen, and pelvis is usually sufficient.[17] Other investigations may be helpful depending on specific clinical needs. Image-guided core biopsy and assessment of hormone receptor status of new distant metastasis are advised as receptor conversion in distant metastasis is known to occur.[50]
Patients on endocrine therapy, like those on tamoxifen – routine age appropriate gynecological screening is recommended. Routine annual pelvic ultrasound is not recommended. While those on aromatase inhibitors, should have periodic bone health monitoring with bone mineral density at baseline and regularly thereafter.[32]
There are no clear surveillance guidelines for patients with bilateral mastectomy and breast reconstruction with implants, however, small studies have shown, no additional benefit with MRI.[51]
Imaging in Pregnant and Lactating Women
Ultrasound is the modality of choice for initial assessment. Physiological changes may make interpretation difficult and hence a lower threshold for follow-up and/or biopsy is advised.[17] Mammography may be safely performed in pregnant women with a negligible risk to the fetus. Wearing a lead apron reduces the radiation dose to the fetus by at least half.[52] [53]
As stochastic risks from radiation have no threshold value, mammography should be carefully used. However, this should not deter us from performing necessary mammographic studies for women suspected to have BC. Breast feeding or pumping milk prior to the examination during lactation reduces breast density.[17] Gadolinium should be limited to situations where benefits clearly outweigh the risks to fetus and hence CEMRI is generally avoided in pregnancy.[54] Breast feeding does not need to be interrupted after gadolinium administration as the water soluble nature of gadolinium-based contrast agents results in a low concentration of gadolinium in the mother's milk.[54]
It is best to perform CEMRI after optimum counseling.
Multidisciplinary Management of BC
Surgical Oncology
Management of BC needs a personalized multimodality approach. In the current era of de-escalation of therapy, we cannot lose sight of the spectrum theory. BC management has seen a paradigm shift from the Halstedian approach of radical local surgery to more conservative approaches based on Fishers' theory that BC is a systemic disease at inception. The current approach is personalized and straddles the spectrum of aggressive biology and genomics to more indolent cases.[55]
Surgery for BC has seen a trend toward conservation of both primary and axillary lymph nodes and increased focus on cosmetic outcome and quality of life (QOL). Oncoplastic techniques have allowed for conservative surgery even in larger tumors and better cosmetic outcomes.[56]
Sequencing of therapy and inclusion of various modalities of therapy (surgery, chemotherapy, targeted therapy, hormone therapy, and radiotherapy) are dependent on patients-related factors like ECOG, co-morbidities, age and tumor-related factors like tumor size, grade, lymph node positivity, hormone and HER2 neu receptor and Ki67 status. Even the 8th AJCC staging system has included grade, receptor status, and ability to take therapy into account when staging BC.[31]
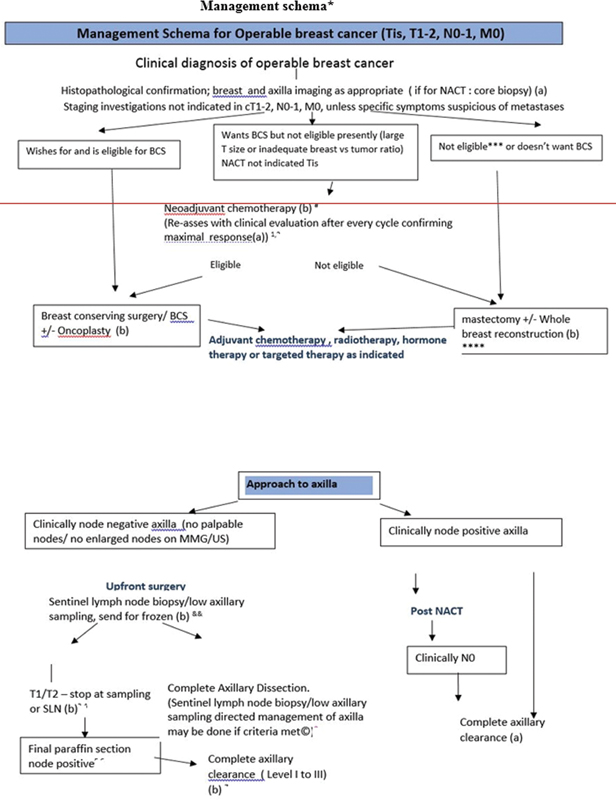
Management Schema for various stages of BC adapted from NCG guidelines 2019[33] is discussed in more details in Annexure 2
Medical Oncology
BC encompasses several subtypes and systemic therapy is indicated depending upon the biology and staging of the disease.
Perioperative Therapy
A multitude of regimens are used with the aim of micrometastases control with comparable outcomes in either NACT or adjuvant chemotherapy (ACT) fashion ([Fig. 4]). Sequential and dose-dense regimens are preferred (Table 1 in Annexure 3). pCR is a robust prognosticator in HER2-positives and triple-negative breast cancer (TNBC) groups.[57] ACT is used to reduce the risk of recurrence (RR). RR risk may be predicted using various clinicopathological factors and genomic signatures (Table 2 in Annexure 3).
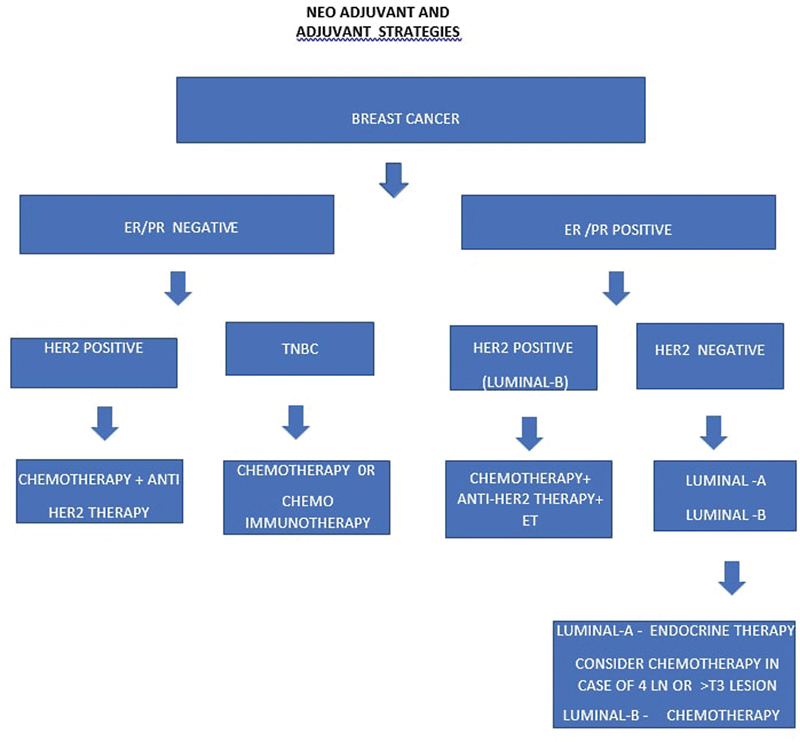
| Figure 4:Neo-adjuvant and adjuvant therapy.
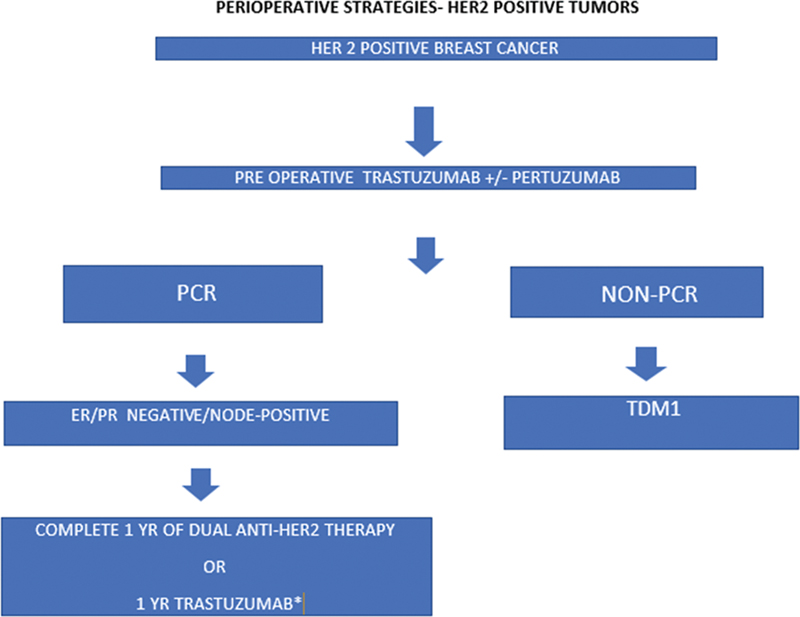
HER2-Positive Tumors
HER2-rich patients should receive perioperative anti-Her2 therapy; 1-year trastuzumab is the current standard with/without pertuzumab (Annexure 4).
Hormone Positive (HR + ) Tumors
Neoadjuvant endocrine therapy alone is sufficient in low RR, HR+ tumors. The duration of ET varies from 5 to 10 years depending upon RR.[58] In premenopausal women, additional ovarian function suppression may be considered if RR is high.
Triple-Negative Tumors
In the NA setting, the addition of immune checkpoint inhibitors (ICIs) has shown benefit.[59] [60] Adjuvant capecitabine and PARP are options in non-pCR groups.[61]
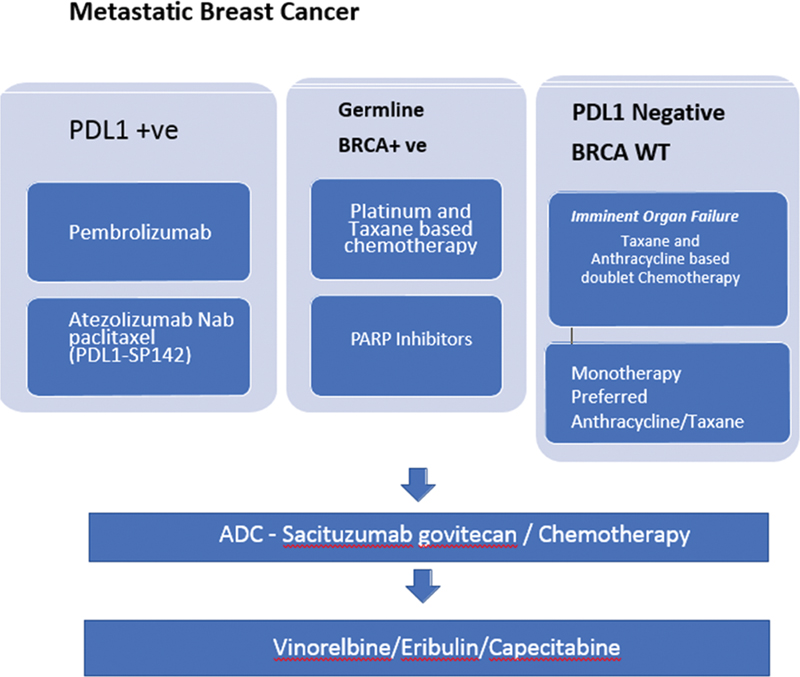
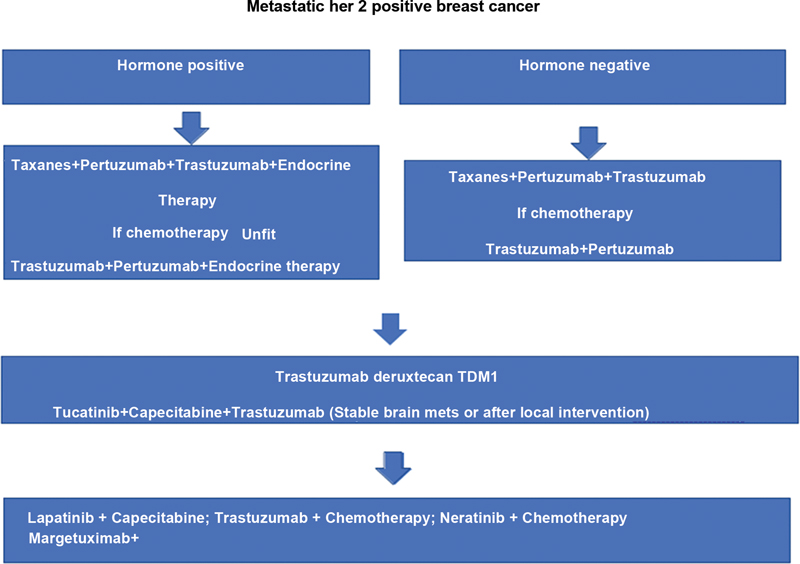
Metastatic Disease
The mainstay of treatment is prolonging life and QOL. The treatment determinants are disease biology, prior therapies, ECOG – performance status, potential toxicities, and patient wishes (Annexures 5, 6, and 7). Interestingly, outcomes of the short course ICI were found comparable to the standard course in a large real-world data.[62]
Specific Populations
Young patients with BC (<40 href="https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0042-1760326#JR22810739-63" xss=removed>63] Pregnancy-associated BC is challenging; however, stage- and biology-matched outcomes are largely comparable if appropriately managed.[64]
Toxicity
Chemotherapy has various side effects including hematological and non-hematological factors (gastrointestinal, cardiac, renal, liver, body image issue, etc.). Chemo-induced alopecia is of major psychological concern; however, a scalp cooling strategy may help in mitigating this issue successfully.[65]
Refer to Table 2 in Annexure 3 for genomic signature, which could help in decide ACT and also regimens for adjuvant setting.
Radiation Oncology
BC patients experience an improvement in locoregional control and overall survival with the addition of adjuvant RT.[66] Nearly 70%-of all BC patients would require RT in their lifetime either in adjuvant or palliative setting and is well tolerated by most. In the adjuvant setting, addition of RT minimizes the microscopic tumor burden in the tumor bed (residual breast or the chest wall) and adjacent regions where the tumor cells are likely to migrate (clinically uninvolved supraclavicular region after a complete axillary clearance). Studies with long-term follow-up show that mastectomy can be avoided if adjuvant whole breast RT is delivered to the conserved breast.[67] In women <50 href="https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0042-1760326#JR22810739-68" xss=removed>68] Whole breast RT can produce acute and late toxicities like radiation dermatitis, induration, breast pain, shrinkage, and leads to poor cosmetic outcomes. Partial breast RT with external beam or brachytherapy delivered over shorter duration helps minimize these toxicities in early, node-negative BC patients after breast conserving surgery.[69] [70]
Palliative RT is recommended to alleviate symptoms such as pain, bleeding, prevent neurological death in brain metastasis and functional loss, and is effective in 60 to 70%-of the patients with minimal side effects.
Management of Locoregional or Distant Recurrence
Locoregional or distant metastatic recurrence is managed depending on the site, however, repeat core biopsy from the first recurrence site is obtained – to look for hormone receptor status evaluation.[32]
Image-Guided Interventions in Palliative Conditions
In symptomatic clinical cases having metastatic bone disease, high intensity focused ultrasound/cryoablation of symptomatic bone metastasis can be performed.[71] [72] Image-guided vertebroplasty is performed for vertebral body collapse.[73] RFA or microwave ablation of liver lesions can be performed by IR (interventional radiology). Chemoport insertion can be performed by IR or surgeons depending on institutional practice.
Summary
There is a rise in the incidence of BC all over the world in recent times. In this era of personalized cancer care, cross specialty knowledge of advances in cancer care is of utmost importance in the management of cancer patients. In this document we have described diagnostic work-up for BC with an emphasis on imaging.
Diagnostic work-up.
Staging of BC.
Response assessment post NACT.
This work-up is followed by philosophies of various treatment approaches (surgery, chemotherapy, or radiotherapy) for different stages and biology of BC. All these has led to decrease in cancer-specific mortality.
Synoptic reporting formats for mammogram, USG, MRI breast, CT scan, and PET CT are discussed in Annexure 8.
ANNEXURE 1 AMERICAN CANCER SOCIETY RECOMMENDS SCREENING MAMMOGRAM (MG)
American Cancer Society recommends screening mammogram (MG) as follows:
|
Age |
Guideline |
|---|---|
|
40–44 years |
Optional – Annual MG |
|
45–54 years |
Annual MG |
|
55 years and older |
Annual/Biennial MG (to be continued till good health or expected life expectancy of at least 10 years) |
( https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html ; last revised January 14, 2022).
American College of Radiology [ACR] and Society of Breast Imaging [SBI] recommends
Annual MG from age 40
( https://www.acraccreditation.org/Mammography-Saves-Lives/Guidelines )
United States Preventive Service Task Force (USPSTF) recommends Biennial screening MG for women from 50 to 74 years (B recommendation)
( https://www.acraccreditation.org/Mammography-Saves-Lives/Guidelines )
European Commission Breast Cancer Guidelines (ECIBC's Guideline Development Group [GDG)]) recommend:
|
Age |
Guideline |
|---|---|
|
40 − 44 |
No screening |
|
45 − 49 |
Biennial/Triennial MG |
|
50 − 69 |
Biennial MG |
|
70 − 74 |
Triennial MG |
Canadian Task Force recommends:
|
Age |
Guideline |
|---|---|
|
40–49 |
No screening, but conditional screening may be adapted by women. |
|
50–69 |
Biennial/Triennial MG |
|
70–74 |
Biennial/Triennial MG |
Abbreviation: MG, mammogram.
( https://canadiantaskforce.ca/guidelines/published-guidelines/breast-cancer-update )
Breast screening program in Australia recommends:
Invitation-based screening MG at biennial interval for 50 to 74 years age. Younger and older women may undergo mammography, without invitation.
Swedish BC guidelines
( https://www.swedish.org/services/womens-health/our-services/mammography/screening-guidelines )
Annual screening MG for age over 40 years
Breast Imaging Society of India (BISI) recommends:
(https://www.bisi.co.in/guidelines/mammography)
| :
*Number of cycles should be based on tumor response/institutional practice.
#Tailoring treatment based on IHC, to be able to consider post NACT adjuvant therapy to non-responders can be discussed with patients ©.
***Contraindications to BCS include: diffuse microcalcification, persistent positive margins, poor patient compliance, previous chest or breast radiation, relative contraindication is multicentricity. Contraindications to radiotherapy, e.g., collagen vascular diseases.
3SNB can be performed either using Dual Dye-Radio Colloid and Blue Dye (preferred method) OR using Blue Dye alone. 1 to 2 mL peritumoral and/or subareolar injection/subdermal injection of patent Blue Dye or 2%-Methylene Blue 10 minutes prior to the surgical incision and 40 MBq in 0.5 mL of 99m-technetium-labeled sulfur/antimony colloid peritumoral and/or subareolar injection/subdermal injection 2 to 12 hours prior to surgery.
5If the patient and tumor characteristics meet the ACOZOG Z-11 (T1, micro metastasis in node, low-grade tumor, ER/PR positive, BCS done, whole breast RT using tangential fields planned) and 1–2 SLN positive, no further axillary surgery may be considered. ©
****Breast reconstruction may be performed by surgeons in motivated and suitable patients following mastectomy. Implant or autologous flap reconstruction can be performed based on patient's suitability and choice of surgeon.
7If cN0 prior to NACT or an OBC with cN1 post chemotherapy cN0: can be considered for SLN/low axillary sampling.
&If FS not available: LAS and final HPR or ALND (level II if no gross enlarged nodes).
Margins in BCS: negative margin defined as no tumor on inked surface. In case of positive margins, should be revised. In case of persistent positive margins, MRM to be considered.
In patients with family history of cancer, younger than 40 years, male breast cancer or patients with synchronous and metachronous breast cancer, can be referred for genetic counselling and those who are willing may be considered for testing to rule out presence of germline pathogenic variant. ©
Screen detected low-grade DCIS undergoing lumpectomy may not require axillary assessment. ©
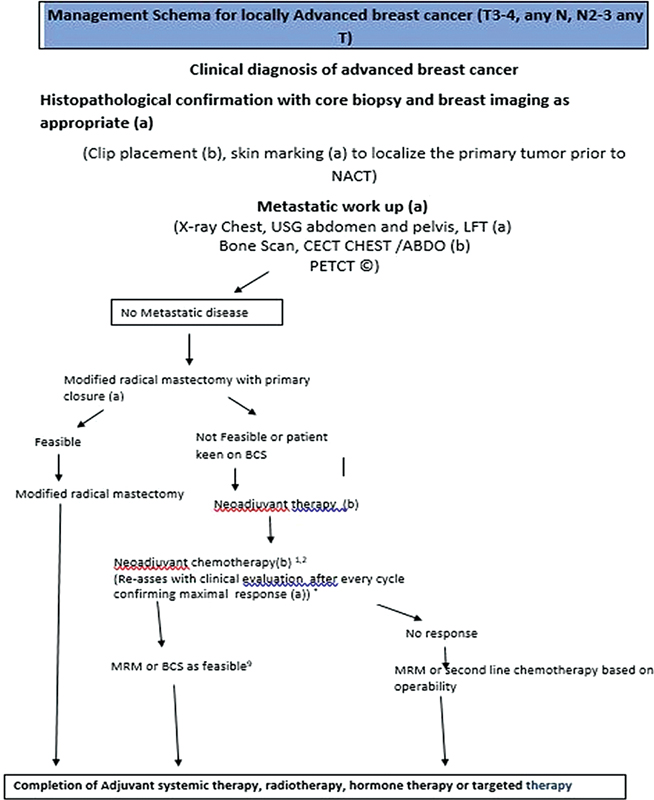
| :
*Source: Adapted from NCG guidelines 2019 (Accessed March 19, 2022).
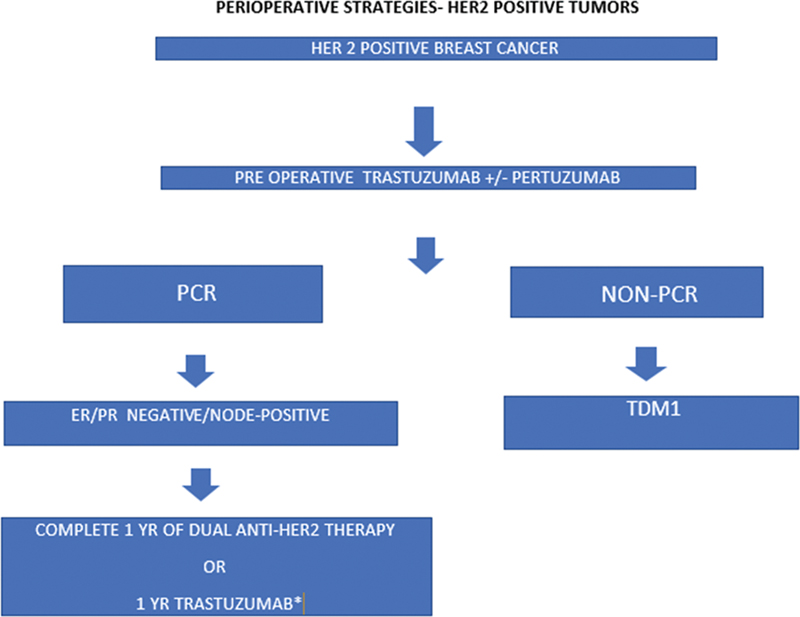
| :
Abbreviations: HER2, human epidermal growth factor receptor; PCR, pathological complete response; TDM1, trastuzumab emtansine.
ANNEXURE 5 METASTATIC BREAST CANCER
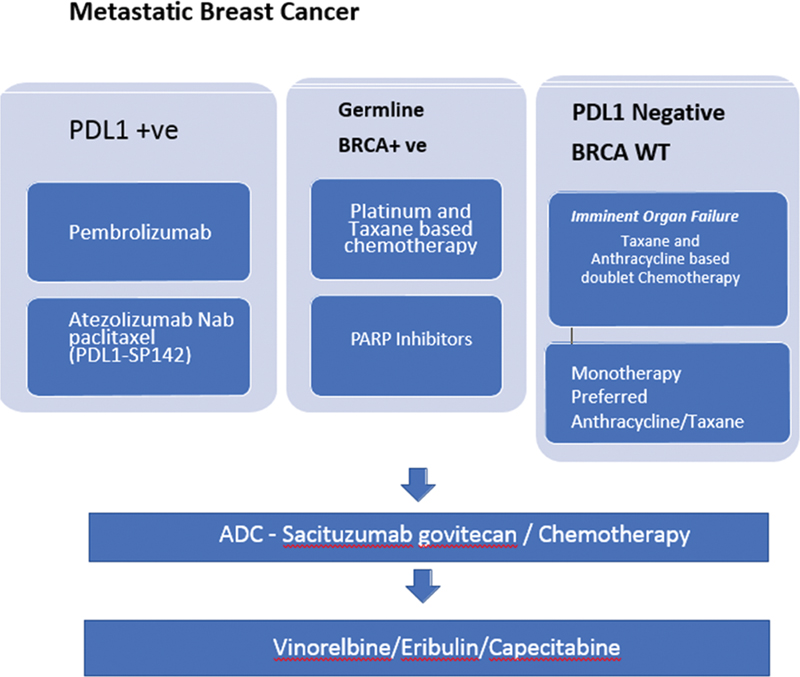
| :
Abbreviations: ADC, antibody drug conjugate; BRCA WT, breast cancer gene wild type; PDL1, programmed death ligand receptor L1.
ANNEXURE 6 HORMONE POSITIVE AND HER2-NEGATIVE METASTATIC TUMOR
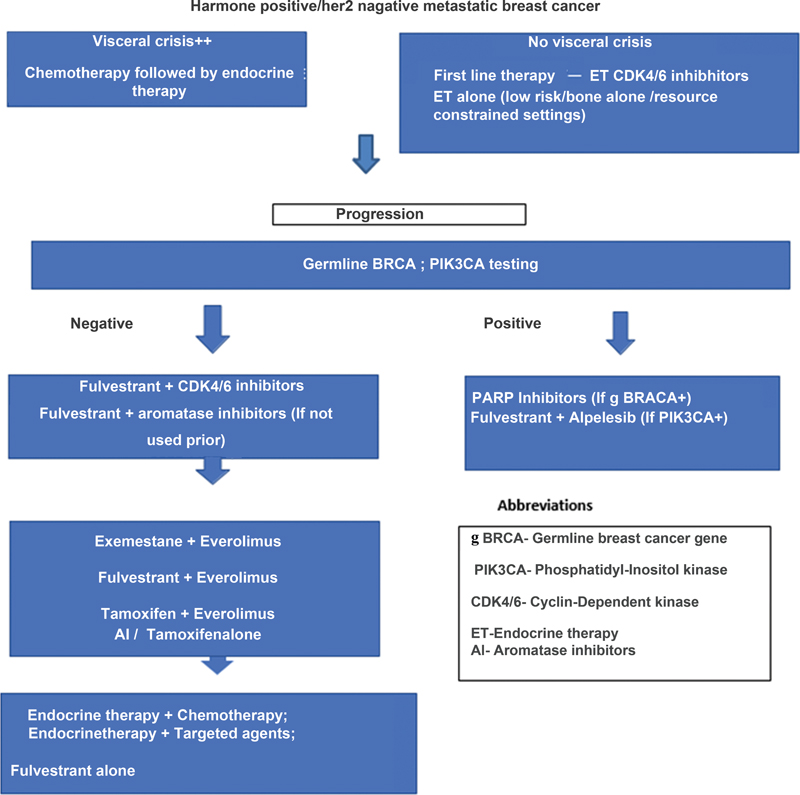
| :
ANNEXURE 7 METASTATIC HER2-POSITIVE TUMOR
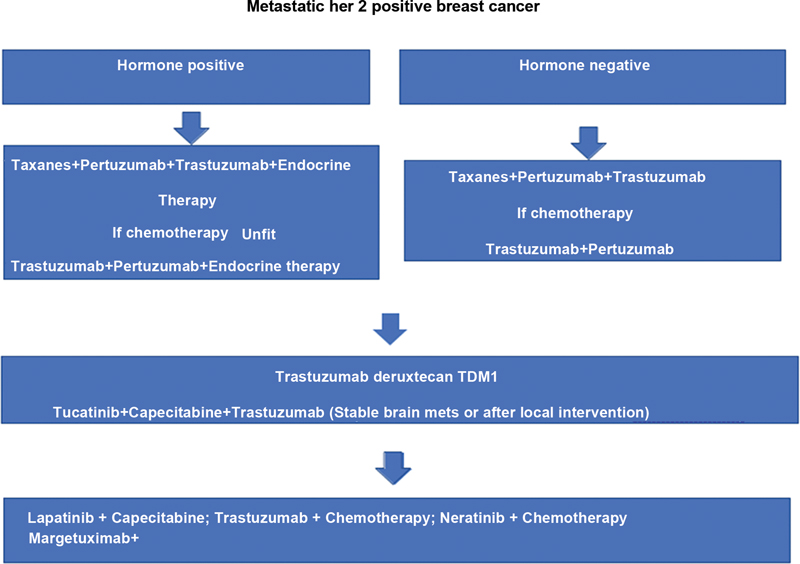
| :
ANNEXURE 8 SYNOPTIC REPORTING FORMATS FOR MAMMOGRAM, USG, MRI BREAST, CT SCAN AND PET CT
Digital mammograms: dated
Bilateral/unilateral
Indication: Screening/diagnostic
Right breast:
Breast composition:
a. The breasts are almost entirely fatty.
b. There are scattered areas of fibroglandular density.
c. The breasts are heterogeneously dense, which may obscure small masses.
d. The breasts are extremely dense, which lowers the sensitivity of mammography.
Normal/Abnormal
If abnormal
A. Mass: Absent/present
If present:
Size:
Location:
| :
Density: iso/high/low/fat containing.
Shape: oval/round/irregular.
Margins: circumscribed/obscured/microlobulated/indistinct/spiculated.
B. Calcifications: absent/present.
If present:
Benign: Vascular/coarse/popcorn/rod-like/round/lucent centered/eggshell/milk of calcium/dystrophic/punctuate/sutural.
Suspicious morphology: Amorphous/coarse heterogeneous/fine pleomorphic/fine linear or fine-linear branching.
Distribution: diffuse/regional/grouped/linear/segmental.
C. Architectural distortion: Absent/present
D. Asymmetry: Absent/present
E. Associated findings:
Skin thickening/skin retraction/nipple retraction/trabecular thickening/abnormal axillary or intramammary nodes.
F. Additional information:
G. Comparison: No change/new lesion/regression/increase in existing lesion.
H. Assessment category:
BIRADS 0/1/2/3/4a/4b/4c/5/6
Left breast:
Breast composition:
a. The breasts are almost entirely fatty.
b. There are scattered areas of fibroglandular density.
c. The breasts are heterogeneously dense, which may obscure small masses.
d. The breasts are extremely dense, which lowers the sensitivity of mammography.
Normal/Abnormal
If abnormal
A. Mass: Absent/present
If present:
Size:
Location:

| :
Density: Iso/high/low/fat containing
Shape: Oval/round/irregular
Margins: Circumscribed/obscured/microlobulated/indistinct/spiculated
B. Calcifications: absent/present If present:
If present:
Benign: Vascular/coarse/popcorn/rod-like/round/lucent centered/eggshell/milk of calcium/dystrophic/punctuate/sutural.
Suspicious morphology: Amorphous/coarse heterogeneous/fine pleomorphic/fine linear or fine-linear branching.
Distribution: Diffuse/regional/grouped/linear/segmental.
C. Architectural distortion: Absent/present.
D. Asymmetry: Absent/present.
E. Associated findings: Skin thickening/skin retraction/nipple retraction/trabecular thickening/abnormal axillary or intramammary nodes.
F. Additional information:
I. Comparison: No change/new lesion/regression/increase in existing lesion.
G. Assessment category:
BIRADS 0/1/2/3/4a/4b/4c/5/6
Breast ultrasound synoptic reporting
Indication
Family history of cancer: Yes/no
Parenchyma
a. Homogeneous background echotexture – fat.
b. Homogeneous background echotexture – fibroglandular.
c. Heterogeneous background echotexture.
Laterality
Right / left / both
Primary lesion evaluation
Single/multiple
Size
Quadrants involved with o'clock position
Shape
Oval/round/irregular
Margin
Circumscribed or
Non-circumscribed (indistinct/angular/microlobulated/spiculated).
Orientation
Parallel /nonparallel
Echopattern
Anechoic/hyperechoic/hypoechoic /isoechoic/complex solid cystic/heterogeneous
Posterior features
No posterior features/enhancement/shadowing/combined pattern
Vascularity
Absent/internal vascularity/vessels in rim
Elasticity assessment
Soft/intermediate/hard
Calcification: yes/no
If yes,
In Mass / Outside Mass / Intraductal
Distance from nipple
Duct
Ductal changes: Yes/No
Satellite lesions
Yes/no
Size
Quadrants
Numbers
Positions in o'clock
Distance from primary lesion and nipple
Axillary nodes
Yes/no
Size
Cortical thickening yes/no (measurement in mm)
Preserved hilum yes/no
Microcalcification in lymph node yes/no
Matted yes/no
Perinodal extension yes/no
Non-hilar blood flow yes/no
Intramammary lymph nodes
Yes/no
Size
Special cases:
Simple cyst
Clustered microcysts
Complicated cyst
Mass in or on skin
Foreign body including implants
Lymph nodes – intramammary
Lymph nodes – axillary
Vascular abnormalities AVMs (arteriovenous malformations/ pseudoaneurysms)
Mondor disease
Postsurgical fluid collection
Fat necrosis
Any other relevant finding
Assessment category
BIRADS 0/1/2/3/4a/4b/4c/5/6
Breast MRI:
Breast MRI performed in a 1.5 T/3T scanner using a dedicated breast coil. Multiplanar Plain T1, T2, STIR, DWI, post contrast dynamic T1 weighted sequence after administration of 0.1 mmol/kg body weight contrast.
Indication:
Any prior breast imaging available: Yes/no
Last menstrual period:
Amount of fibroglandular Parenchyma: Type a, b, c, d
Background parenchymal enhancement intensity:minimal, mild, moderate, severe
Symmetry: Symmetric/asymmetric
Right breast
Mass:
Location
Size
Shape: Round/oval/irregular
Margins: Circumscribed non-circumscribed: irregular/spiculated
T2 SI
DWI:
Enhancement morphology: Homogeneous/heterogeneous/rim/dark internal septations
Kinetic curve assessment:
Initial phase: Fast/medium/slow
Delayed phase: wash-out/persistent/plateau
Non-mass enhancement:
Distribution: Focal/linear/ segmental/regional/ multiple regions/diffuse
Morphology: Homogeneous/heterogeneous/ clumped/clustered ring
Focus: Number and symmetry
Other findings: Cysts/non enhancing mass/dilated ducts/etc.
Skin thickening
Nipple retraction:
Chest wall invasion:
Axillary nodes
Internal mammary nodes:
Left breast
Mass:
Location
Size
Shape: round oval irregular
Margins: Circumscribed non-circumscribed: irregular/spiculated
T2 SI
DWI:
Enhancement morphology: homogeneous/heterogeneous/rim/dark internal septations
Kinetic curve assessment:
Initial phase: fast/medium/slow
Delayed phase: Washout/persistent/plateau
Non-mass enhancement:
Distribution: Focal/linear/segmental/regional/multiple regions/diffuse
Morphology: Homogeneous/heterogeneous/clumped/clustered ring
Focus: Number and symmetry
Other findings: Cysts/non enhancing mass/dilated ducts/etc.
Skin thickening
Nipple retraction:
Chest wall invasion:
Axillary nodes
Internal mammary nodes:
Visualized Liver: If any abnormality seen
Visualized bones:
Impression:
BIRADS: 1/2/3/4a/4b/4c/5/6
Breast cancer CT scan
CT scan of chest, abdomen, and pelvis
Contrast enhanced CT scan performed.
Indication:
Base line evaluation/post-NACT evaluation. Comparison made with prior CT dated ()/other indication
Primary lesion evaluation
Laterality: Right/left
Tumor size
Skin thickening: present absent
Nipple retraction: present absent
Chest wall invasion: present absent
Axillary nodes: present absent
If present, number and size of largest
Internal mammary nodes: present absent
If present, number and size of largest
Supraclavicular nodes: present absent
If present, number and size of largest
Contralateral breast: unremarkable
Contralateral axilla: unremarkable
Metastatic disease evaluation:
Mediastinal nodes:
Lungs:
Pleura:
Heart and mediastinal great vessels:
Liver:
Adrenals:
Gall bladder:
Pancreas:
Spleen:
Kidneys:
Bowel:
Peritoneum:
Urinary bladder:
Uterus:
Ovaries:
Retroperitoneal and pelvic adenopathy
Free fluid:
Major vessels:
Visualized bones:
Any other finding:
Impression:
Synoptic reports for FDG PETCT:
|
Component of report |
Description |
|
Clinical history |
Age of patient |
|
Type of cancer – histology, receptor status |
|
|
Indication – staging, restaging, treatment response |
|
|
Surgical status – preoperative staging/postoperative staging |
|
|
Histopathology (if operated) – primary, nodal status, receptor status, |
|
|
Treatment received (if restaging, treatment response) |
|
|
Procedure followed |
Dose of 18F FDG injected |
|
Uptake time (post injection waiting before acquisition – anywhere between 45 minute–70 minute) |
|
|
Region imaged – whole body (base skull to mid-thigh, head to mid-thigh, head to toe) Only regional – liver, thorax |
|
|
Acquisition – with contrast CT or non-contrast CT, oral contrast given |
|
|
Any specific change in acquisition – prone, sideways, propped up |
|
|
Need for any medication/interventions – Anesthesia, β blockers |
|
|
Findings |
FDG uptake: Primary: Uptake in the region of breast – affected side • Focal uptakes in nodule (preoperative) or diffuse uptake without obvious mass lesion. • Multiplicity. • Overlying skin thickening – presence or absence. • Extension of lesion into underlying tissue – muscle, chest wall, rib. • Lateral or medial extent. |
|
Contra lateral breast uptake – if abnormal (describe as above) |
|
|
Nodes: Ipsilateral axilla Ipsilateral internal mammary Ipsilateral supraclavicular Cervical nodes Contra lateral internal mammary Contra lateral internal mammary Contra lateral axillary Other nodal site: Mediastinal Abdominal Pelvic |
|
|
Metastases: Lung nodules – side, well defined, multiplicity Liver – segment/lobes Bones – marrow, cortical · Lytic, sclerotic, mixed |
|
|
Comparison |
With previous FDG PETCT/any anatomical imaging. · Mention date · Change in size · Change in FDG uptake · New lesion |
|
Impression |
· Summarize findings to suggest presence of absence of disease if possible. · If not possible to confidentially suggest presence of disease, provide differentials. · Help direct toward additional procedure if needed to arrive at a diagnosis. · Suggestion for timings of follow up if indicated. |
References
- nbsp;Sung H, Ferlay J, Siegel RL. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- nbsp;Global Cancer Observatory. Accessed March 18, 2022, at: https://gco.iarc.fr/
- nbsp;Lima SM, Kehm RD, Terry MB. Global breast cancer incidence and mortality trends by region, age-groups, and fertility patterns. EClinicalMedicine 2021; 38: 100985
- nbsp;Mathur P, Sathishkumar K, Chaturvedi M. et al; ICMR-NCDIR-NCRP Investigator Group. Cancer statistics, 2020: report from National Cancer Registry Programme, India. JCO Glob Oncol 2020; 6 (06) 1063-1075
- nbsp;Wu S, Zhu W, Thompson P, Hannun YA. Evaluating intrinsic and non-intrinsic cancer risk factors. Nat Commun 2018; 9 (01) 3490
- nbsp;Institute of Medicine (US) Committee on Cancer Control in Low- and Middle-Income Countries. Cancer Control Opportunities in Low- and Middle-Income Countries. Cancer Control Opportunity Low-Middle-Income Countries. in: Sloan FA, Gelband H. eds. Washington, DC: National Academies Press; 2007
- nbsp;What Are the Risk Factors for Breast Cancer? | CDC. Accessed March 18, 2022, at: https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm
- nbsp;Morris KT, Pommier RF, Morris A. et al. Usefulness of the triple test score for palpable breast masses; discussion 1012-3. Arch Surg 2001; 136 (09) 1008-1012
- nbsp;Hortobagyi GN, Connolly JL, D'Orsi CJ, Yang WT. Breast. in: Amin MB, Edge S, Greene F. et al., eds; American Joint Committee on Cancer 8th ed.. Springer: AJCC cancer staging manual; 2017: 589-636
- AJCC 8th edition staging; 2018, at: Accessed on 12th Jan 2023 http://www.breastsurgeonsweb.com/wp-content/uploads/downloads/2020/10/AJCC-Breast-Cancer-Staging-System.pdf
- Mainiero MB, Moy L, Baron P. et al; Expert Panel on Breast Imaging. ACR Appropriateness Criteria® Breast Cancer Screening. J Am Coll Radiol 2017; 14 (11S): S383-S390
- Chakrabarthi S, Panwar S, Singh T. et al. Best Practice Guidelines for Breast Imaging, Breast Imaging Society, India. Ann Natl Acad Med Sci 2022; 58 (Suppl. 02) 060-068
- Massat NJ, Dibden A, Parmar D, Cuzick J, Sasieni PD, Duffy SW. Impact of screening on breast cancer mortality: the UK program 20 years on. Cancer Epidemiol Biomarkers Prev 2016; 25 (03) 455-462
- Lee CH, Dershaw DD, Kopans D. et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol 2010; 7 (01) 18-27
- Protocols for surveillance of women at very high risk of developing breast cancer - GOV.UK. Accessed March 18, 2022, at: https://www.gov.uk/government/publications/breast-screening-higher-risk-women-surveillance-protocols/protocols-for-surveillance-of-women-at-higher-risk-of-developing-breast-cancer
- Mendelson EB. Problem-solving ultrasound. Radiol Clin North Am 2004; 42 (05) 909-918 , vii
- Guidance on screening and symptomatic breast imaging, Fourth edition | The Royal College of Radiologists. Accessed March 18, 2022, at: https://www.rcr.ac.uk/publication/guidance-screening-and-symptomatic-breast-imaging-fourth-edition
- Sharpe Jr RE, Venkataraman S, Phillips J. et al. Increased cancer detection rate and variations in the recall rate resulting from implementation of 3D digital breast tomosynthesis into a population-based screening program. radiology. Radiology 2016; 278 (03) 698-706
- D'Orsi CJ, Sickles EA, Mendelson EB. et al. ACR BI-RADS Mammography. In: ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. 5th ed.. Reston, VA: American College of Radiology; 2013: 134-136
- Lee S, Jung Y, Bae Y. Synchronous BI-RADS category 3 lesions on preoperative ultrasonography in patients with breast cancer: is short-term follow-up appropriate?. J Breast Cancer 2015; 18 (02) 181-186
- Kim SJ, Ko EY, Shin JH. et al. Application of sonographic BI-RADS to synchronous breast nodules detected in patients with breast cancer. AJR Am J Roentgenol 2008; 191 (03) 653-658
- Indian Council of Medical Research, Government of India. ICMR Subcommittee on Breast Cancer. Consensus document for management of breast cancer, 2016. March 19, 2022, at: http://cancerindia.org.in/wp-content/uploads/2017/11/Breast_Cancer.pdf. - Google Search
- Canadian Association of Radiologists. CAR Practice guidelines and technical standards for breast imaging and intervention. Approved on September 29, 2012; modified on September 17, 2016. Accessed September 2021, at: https://car.ca/wp-content/uploads/Breast-Imaging-and-Intervention-2016.pdf
- American College of Radiology. ACR practice parameter for the performance of ultrasound-guided percutaneous breast interventional procedures, Revised 2021 (Resolution 31). Accessed March 19, 2022, at: https://www.acr.org/-/media/acr/files/practice-parameters/us-guidedbreast.pdf. – Google Search
- ACR practice parameter for the performance of magnetic resonance imaging–guided breast interventional procedures, Revised 2021 (Resolution 29). Accessed March 19, 2022, at: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/MR-Guided-Breast.pdf – Google Search
- Chakrabarthi S. Stereotactic breast biopsy: a review & applicability in the Indian context. Indian J Med Res 2021; 154 (02) 237-247
- Ghaderi KF, Phillips J, Perry H, Lotfi P, Mehta TS. Contrast-enhanced mammography: current applications and future directions. Radiographics 2019; 39 (07) 1907-1920
- Harbeck N, Penault-Llorca F, Cortes J. et al. Breast cancer. Nat Rev Dis Primers 2019; 5 (01) 66
- Taneja S, Evans AJ, Rakha EA, Green AR, Ball G, Ellis IO. The mammographic correlations of a new immunohistochemical classification of invasive breast cancer. Clin Radiol 2008; 63 (11) 1228-1235
- Boisserie-Lacroix M, Hurtevent-Labrot G, Ferron S, Lippa N, Bonnefoi H, Mac Grogan G. Correlation between imaging and molecular classification of breast cancers. Diagn Interv Imaging 2013; 94 (11) 1069-1080
- The American College of Surgeons. Part IX - Breast, AJCC cancer staging manual, 8th edition, updated May 25 2018. Accessed March 19, 2022, at: http://www.breastsurgeonsweb.com/wp-content/uploads/downloads/2020/10/AJCC-Breast-Cancer-Staging-System.pdf - Google Search
- National Comprehensive Cancer Network. Breast Cancer Version 4.2022 — June 21, 2022. Accessed November 10, 2022, at: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
- National Cancer Grid. India. National Cancer Grid Breast Cancer Management Guidelines, September, 2019. Accessed March 19, 2022, at: https://tmc.gov.in/ncg/docs/PDF/DraftGuidelines/Breast/NCG_guidelines_2019_Breast.pdf - Google Search
- Algorithm for Breast Imaging - Breast Imaging Society. India. Accessed March 19, 2022, at: https://www.bisi.co.in/guidelines/algorithm-for-breast-imaging/
- Kalli S, Semine A, Cohen S, Naber SP, Makim SS, Bahl M. American Joint Committee on Cancer's Staging System for breast cancer, eighth edition: what the radiologist needs to know. Radiographics 2018; 38 (07) 1921-1933
- Teichgraeber DC, Guirguis MS, Whitman GJ. Breast cancer staging: Updates in the AJCC cancer staging manual, 8th edition, and current challenges for radiologists, from the AJR special series on cancer staging. Am J Roentgenol 2021; 217 (02) 278-290
- Chang JM, Leung JWT, Moy L, Ha SM, Moon WK. Axillary nodal evaluation in breast cancer: state of the art. Radiology 2020; 295 (03) 500-515
- van Nijnatten TJA, Jochelson MS, Lobbes MBI. Axillary lymph node characteristics in breast cancer patients versus post-COVID-19 vaccination: overview of current evidence per imaging modality. Eur J Radiol 2022; 152: 110334
- Pesapane F, Downey K, Rotili A, Cassano E, Koh D-M. Imaging diagnosis of metastatic breast cancer. Insights Imaging 2020; 11 (01) 79
- Barra FR, Sobrinho AB, Barra RR. et al. Contrast-enhanced mammography (CEM) for detecting residual disease after neoadjuvant chemotherapy: a comparison with breast magnetic resonance imaging (MRI). BioMed Res Int 2018; 2018: 8531916
- Holmes D, Colfry A, Czerniecki B. et al. Performance and practice guideline for the use of neoadjuvant systemic therapy in the management of breast cancer. Ann Surg Oncol 2015; 22 (10) 3184-3190
- Fowler AM, Mankoff DA, Joe BN. Imaging neoadjuvant therapy response in breast cancer. Radiology 2017; 285 (02) 358-375
- Riedl CC, Pinker K, Ulaner GA. et al. Comparison of FDG-PET/CT and contrast-enhanced CT for monitoring therapy response in patients with metastatic breast cancer. Eur J Nucl Med Mol Imaging 2017; 44 (09) 1428-1437
- Dose Schwarz J, Bader M, Jenicke L, Hemminger G, Jänicke F, Avril N. Early prediction of response to chemotherapy in metastatic breast cancer using sequential 18F-FDG PET. J Nucl Med 2005; 46 (07) 1144-1150
- Janssen NNY, Nijkamp J, Alderliesten T. et al. Radioactive seed localization in breast cancer treatment. Br J Surg 2016; 103 (01) 70-80
- Garzotto F, Comoretto RI, Michieletto S. et al. Preoperative non-palpable breast lesion localization, innovative techniques and clinical outcomes in surgical practice: a systematic review and meta-analysis. Breast 2021; 58: 93-105
- Flowers CI, Mooney BP, Drukteinis JS. Clinical and imaging surveillance following breast cancer diagnosis. Am Soc Clin Oncol Educ Book 2012; •••: 59-64
- Brennan S, Liberman L, Dershaw DD, Morris E. Breast MRI screening of women with a personal history of breast cancer. AJR Am J Roentgenol 2010; 195 (02) 510-516
- Kerridge WD, Kryvenko ON, Thompson A, Shah BA. Fat necrosis of the breast: a pictorial review of the mammographic, ultrasound, CT, and MRI findings with histopathologic correlation. Radiol Res Pract 2015; 2015: 613139
- Schrijver WAME, Suijkerbuijk KPM, van Gils CH, van der Wall E, Moelans CB, van Diest PJ. Receptor conversion in distant breast cancer metastases: a systematic review and meta-analysis. J Natl Cancer Inst 2018; 110 (06) 568-580
- Golan O, Amitai Y, Barnea Y, Menes TS. Yield of surveillance magnetic resonance imaging after bilateral mastectomy and reconstruction: a retrospective cohort study. Breast Cancer Res Treat 2019; 174 (02) 463-468
- Osei EK, Faulkner K. Fetal doses from radiological examinations. Br J Radiol 1999; 72 (860) 773-780
- Sechopoulos I, Suryanarayanan S, Vedantham S, D'Orsi CJ, Karellas A. Radiation dose to organs and tissues from mammography: Monte Carlo and phantom study. Radiology 2008; 246 (02) 434-443
- Committee Opinion No. Committee opinion no. 723: guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol 2017; 130 (04) e210-e216
- Özmen V. Paradigm shift from Halstedian radical mastectomy to personalized medicine. J Breast Health 2017; 13 (02) 50-53
- Parmar V, Koppiker CB, Dixit S. Breast conservation surgery & oncoplasty in India – current scenario. Indian J Med Res 2021; 154 (02) 221-228
- Berruti A, Amoroso V, Gallo F. et al. Pathologic complete response as a potential surrogate for the clinical outcome in patients with breast cancer after neoadjuvant therapy: a meta-regression of 29 randomized prospective studies. J Clin Oncol 2014; 32 (34) 3883-3891
- Burstein HJ, Lacchetti C, Anderson H. et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol 2019; 37 (05) 423-438
- Schmid P, Cortes J, Pusztai L. et al; KEYNOTE-522 Investigators. Pembrolizumab for early triple-negative breast cancer. N Engl J Med 2020; 382 (09) 810-821
- Emens LA, Adams S, Barrios CH. et al. First-line atezolizumab plus nab-paclitaxel for unresectable, locally advanced, or metastatic triple-negative breast cancer: IMpassion130 final overall survival analysis. Ann Oncol 2021; 32 (08) 983-993
- Masuda N, Lee S-J, Ohtani S. et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med 2017; 376: 2147-2159
- Abraham G, Noronha V, Rajappa S. et al. The clinical utility and safety of short-course immune checkpoint inhibitors in multiple tumours-A real-world multicentric study from India. Int J Cancer 2022; 150 (06) 1045-1052
- Bajpai J, Ventrapati P, Joshi S. et al. Unique challenges and outcomes of young women with breast cancers from a tertiary care cancer centre in India. Breast 2021; 60: 177-184
- Bajpai J, Simha V, Shylasree TS. et al. Pregnancy associated breast cancer (PABC): Report from a gestational cancer registry from a tertiary cancer care centre, India. Breast 2021; 56: 88-95
- Bajpai J, Kagwade S, Chandrasekharan A. et al. “Randomised controlled trial of scalp cooling for the prevention of chemotherapy induced alopecia”. Breast 2020; 49: 187-193
- Darby S, McGale P, Correa C. et al; Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 2011; 378 (9804): 1707-1716
- Clarke M, Collins R, Darby S. et al; Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005; 366 (9503): 2087-2106
- Bartelink H, Horiot JC, Poortmans PM. et al. Impact of a higher radiation dose on local control and survival in breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost EORTC 22881-10882 trial. J Clin Oncol 2007; 25 (22) 3259-3265
- Polgár C, Major T, Fodor J. et al. Accelerated partial-breast irradiation using high-dose-rate interstitial brachytherapy: 12-year update of a prospective clinical study. Radiother Oncol 2010; 94 (03) 274-279
- Meattini I, Marrazzo L, Saieva C. et al. Accelerated partial-breast irradiation compared with whole-breast irradiation for early breast cancer: long-term results of the randomized phase III APBI-IMRT-Florence trial. J Clin Oncol 2020; 38 (35) 4175-4183
- Bertrand AS, Iannessi A, Natale R. et al. Focused ultrasound for the treatment of bone metastases: effectiveness and feasibility. J Ther Ultrasound 2018; 6 (01) 8
- Tuncali K, Morrison PR, Winalski CS. et al. MRI-guided percutaneous cryotherapy for soft-tissue and bone metastases: initial experience. AJR Am J Roentgenol 2007; 189 (01) 232-239
- Wallace AN, Greenwood TJ, Jennings JW. Use of imaging in the management of metastatic spine disease with percutaneous ablation and vertebral augmentation. AJR AM J Roentgenol 2015; 205 (02) 434-441
Address for correspondence
Meenakshi Thakur, MDDepartment of Radiodiagnosis, Tata Memorial CentreMumbai 400012IndiaEmail: thakurmh@yahoo.co.inPublication History
Article published online:
04 May 2023© 2023. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
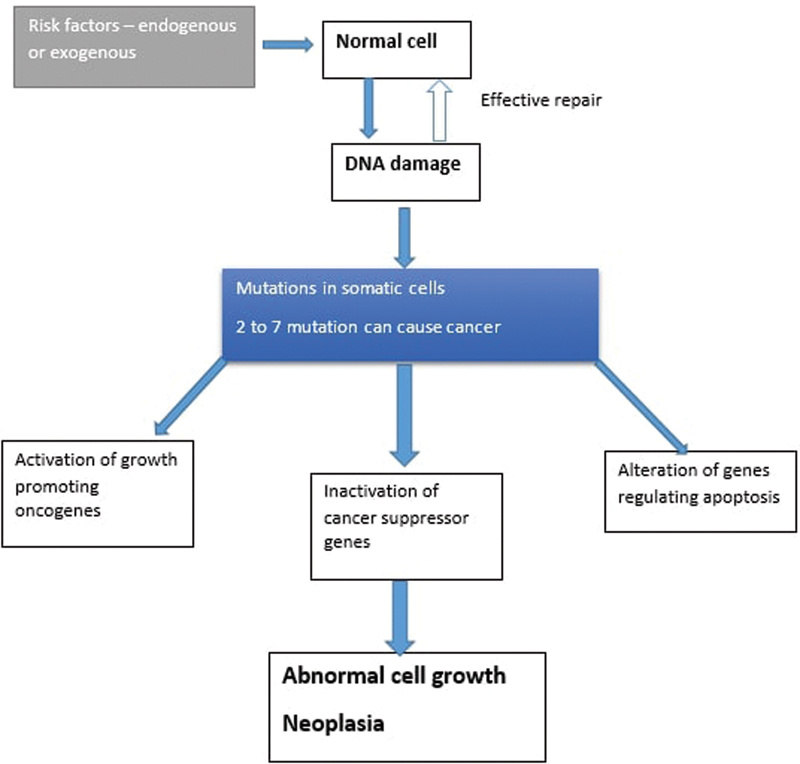
| Fig. 1 :Etiopathogenesis of cancer.
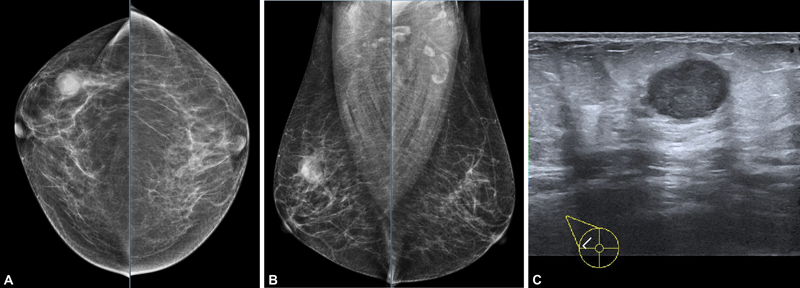
| Figure 2:A 50-year-old female with right breast lump since 1 month. No other complains. On mammogram (A and B) and USG: a well-defined high-density mass with partly obscured margins is seen in the upper outer quadrant of right breast, measuring approximately 1.9 × 2.2 × 2.3 cm. No suspicious microcalcifications are seen. No other associated features are seen. On USG (C) irregular mass with microlobulated margin is seen at 10 o'clock position in right breast. The lesion is predominantly hypoechoic with posterior acoustic enhancement. The lesion is parallel in orientation. No suspicious axillary lymph nodes are seen on imaging. Histopathology of lesion is TNBC. As this lesion is early stage breast cancer without nodal involvement (stage IIA), further metastatic work-up is not needed. (TNBC, triple-negative breast cancer; USG, ultrasonography).
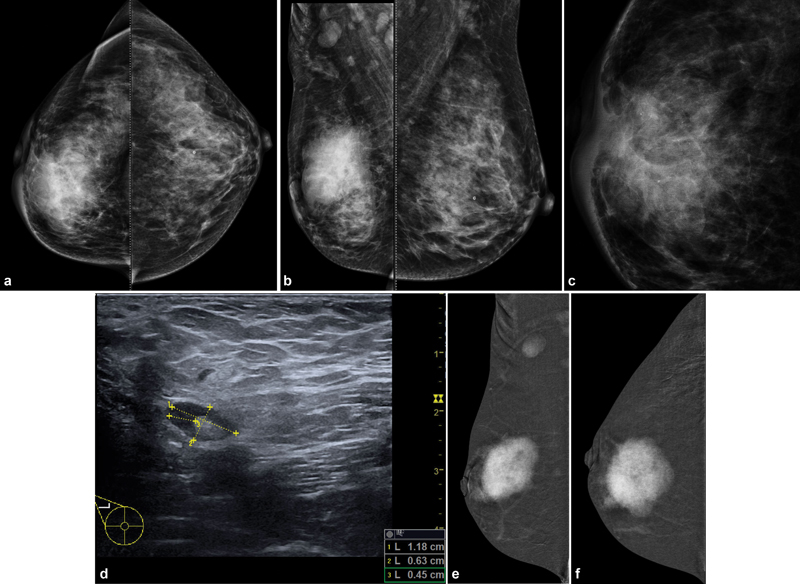
| Figure 3:A 38-year-old female with increasing right breast lump since 15 months. Mammogram (A, B): An irregular high-density mass with indistinct margins is seen in predominantly upper inner quadrant also extending in the outer quadrant measuring approximately 4.4 × 4.4 × 5.5 cm. Pleomorphic microcalcifications (C) are seen within the mass, better seen on magnification view. Diffuse trabecular thickening with nipple areolar complex thickening and retraction is seen. Few suspicious right axillary nodes are seen, largest measuring 1.2 × 0.7 cm with 4.5-mm cortical thickness (D). In view of dense breast parenchyma, further evaluation with CEM was performed to rule out any other lesion in breast, CEM (E, F) is suggestive of large unifocal lesion. This is the case of locally advanced breast cancer (stage IIIA), further metastatic work-up was performed. On CT scan, (G, H) heterogeneously enhancing mass is seen involving right breast with involvement of overlying skin. Enlarged right axillary, right internal mammary, and right supraclavicular lymph nodes are seen. (CEM, contrast-enhanced mammogram.)
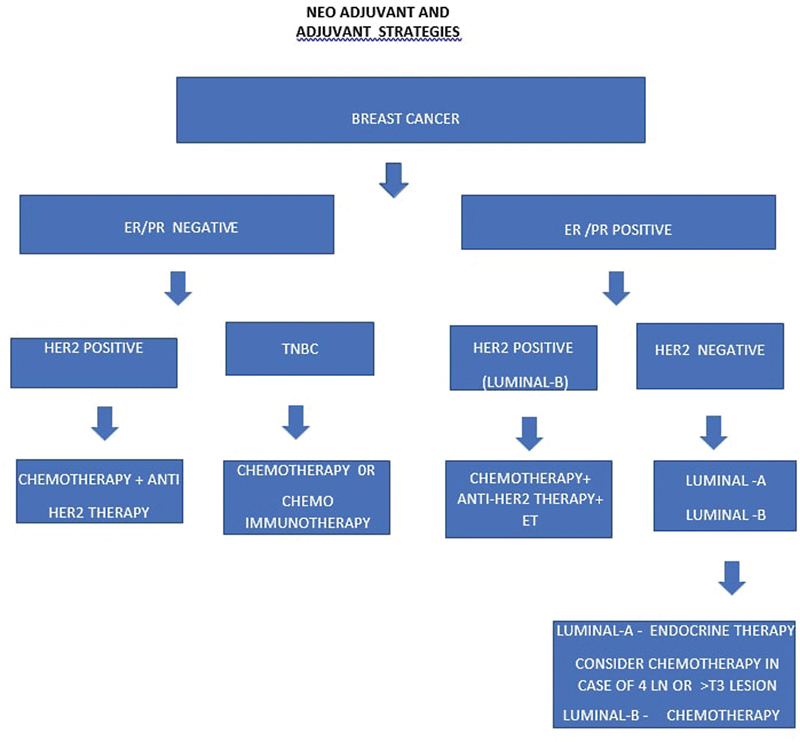
| Figure 4:Neo-adjuvant and adjuvant therapy.
| :
| :
| :
| :
| :
| :

| :
References
- nbsp;Sung H, Ferlay J, Siegel RL. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- nbsp;Global Cancer Observatory. Accessed March 18, 2022, at: https://gco.iarc.fr/
- nbsp;Lima SM, Kehm RD, Terry MB. Global breast cancer incidence and mortality trends by region, age-groups, and fertility patterns. EClinicalMedicine 2021; 38: 100985
- nbsp;Mathur P, Sathishkumar K, Chaturvedi M. et al; ICMR-NCDIR-NCRP Investigator Group. Cancer statistics, 2020: report from National Cancer Registry Programme, India. JCO Glob Oncol 2020; 6 (06) 1063-1075
- nbsp;Wu S, Zhu W, Thompson P, Hannun YA. Evaluating intrinsic and non-intrinsic cancer risk factors. Nat Commun 2018; 9 (01) 3490
- nbsp;Institute of Medicine (US) Committee on Cancer Control in Low- and Middle-Income Countries. Cancer Control Opportunities in Low- and Middle-Income Countries. Cancer Control Opportunity Low-Middle-Income Countries. in: Sloan FA, Gelband H. eds. Washington, DC: National Academies Press; 2007
- nbsp;What Are the Risk Factors for Breast Cancer? | CDC. Accessed March 18, 2022, at: https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm
- nbsp;Morris KT, Pommier RF, Morris A. et al. Usefulness of the triple test score for palpable breast masses; discussion 1012-3. Arch Surg 2001; 136 (09) 1008-1012
- nbsp;Hortobagyi GN, Connolly JL, D'Orsi CJ, Yang WT. Breast. in: Amin MB, Edge S, Greene F. et al., eds; American Joint Committee on Cancer 8th ed.. Springer: AJCC cancer staging manual; 2017: 589-636
- AJCC 8th edition staging; 2018, at: Accessed on 12th Jan 2023 http://www.breastsurgeonsweb.com/wp-content/uploads/downloads/2020/10/AJCC-Breast-Cancer-Staging-System.pdf
- Mainiero MB, Moy L, Baron P. et al; Expert Panel on Breast Imaging. ACR Appropriateness Criteria® Breast Cancer Screening. J Am Coll Radiol 2017; 14 (11S): S383-S390
- Chakrabarthi S, Panwar S, Singh T. et al. Best Practice Guidelines for Breast Imaging, Breast Imaging Society, India. Ann Natl Acad Med Sci 2022; 58 (Suppl. 02) 060-068
- Massat NJ, Dibden A, Parmar D, Cuzick J, Sasieni PD, Duffy SW. Impact of screening on breast cancer mortality: the UK program 20 years on. Cancer Epidemiol Biomarkers Prev 2016; 25 (03) 455-462
- Lee CH, Dershaw DD, Kopans D. et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol 2010; 7 (01) 18-27
- Protocols for surveillance of women at very high risk of developing breast cancer - GOV.UK. Accessed March 18, 2022, at: https://www.gov.uk/government/publications/breast-screening-higher-risk-women-surveillance-protocols/protocols-for-surveillance-of-women-at-higher-risk-of-developing-breast-cancer
- Mendelson EB. Problem-solving ultrasound. Radiol Clin North Am 2004; 42 (05) 909-918 , vii
- Guidance on screening and symptomatic breast imaging, Fourth edition | The Royal College of Radiologists. Accessed March 18, 2022, at: https://www.rcr.ac.uk/publication/guidance-screening-and-symptomatic-breast-imaging-fourth-edition
- Sharpe Jr RE, Venkataraman S, Phillips J. et al. Increased cancer detection rate and variations in the recall rate resulting from implementation of 3D digital breast tomosynthesis into a population-based screening program. radiology. Radiology 2016; 278 (03) 698-706
- D'Orsi CJ, Sickles EA, Mendelson EB. et al. ACR BI-RADS Mammography. In: ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. 5th ed.. Reston, VA: American College of Radiology; 2013: 134-136
- Lee S, Jung Y, Bae Y. Synchronous BI-RADS category 3 lesions on preoperative ultrasonography in patients with breast cancer: is short-term follow-up appropriate?. J Breast Cancer 2015; 18 (02) 181-186
- Kim SJ, Ko EY, Shin JH. et al. Application of sonographic BI-RADS to synchronous breast nodules detected in patients with breast cancer. AJR Am J Roentgenol 2008; 191 (03) 653-658
- Indian Council of Medical Research, Government of India. ICMR Subcommittee on Breast Cancer. Consensus document for management of breast cancer, 2016. March 19, 2022, at: http://cancerindia.org.in/wp-content/uploads/2017/11/Breast_Cancer.pdf. - Google Search
- Canadian Association of Radiologists. CAR Practice guidelines and technical standards for breast imaging and intervention. Approved on September 29, 2012; modified on September 17, 2016. Accessed September 2021, at: https://car.ca/wp-content/uploads/Breast-Imaging-and-Intervention-2016.pdf
- American College of Radiology. ACR practice parameter for the performance of ultrasound-guided percutaneous breast interventional procedures, Revised 2021 (Resolution 31). Accessed March 19, 2022, at: https://www.acr.org/-/media/acr/files/practice-parameters/us-guidedbreast.pdf. – Google Search
- ACR practice parameter for the performance of magnetic resonance imaging–guided breast interventional procedures, Revised 2021 (Resolution 29). Accessed March 19, 2022, at: https://www.acr.org/-/media/ACR/Files/Practice-Parameters/MR-Guided-Breast.pdf – Google Search
- Chakrabarthi S. Stereotactic breast biopsy: a review & applicability in the Indian context. Indian J Med Res 2021; 154 (02) 237-247
- Ghaderi KF, Phillips J, Perry H, Lotfi P, Mehta TS. Contrast-enhanced mammography: current applications and future directions. Radiographics 2019; 39 (07) 1907-1920
- Harbeck N, Penault-Llorca F, Cortes J. et al. Breast cancer. Nat Rev Dis Primers 2019; 5 (01) 66
- Taneja S, Evans AJ, Rakha EA, Green AR, Ball G, Ellis IO. The mammographic correlations of a new immunohistochemical classification of invasive breast cancer. Clin Radiol 2008; 63 (11) 1228-1235
- Boisserie-Lacroix M, Hurtevent-Labrot G, Ferron S, Lippa N, Bonnefoi H, Mac Grogan G. Correlation between imaging and molecular classification of breast cancers. Diagn Interv Imaging 2013; 94 (11) 1069-1080
- The American College of Surgeons. Part IX - Breast, AJCC cancer staging manual, 8th edition, updated May 25 2018. Accessed March 19, 2022, at: http://www.breastsurgeonsweb.com/wp-content/uploads/downloads/2020/10/AJCC-Breast-Cancer-Staging-System.pdf - Google Search
- National Comprehensive Cancer Network. Breast Cancer Version 4.2022 — June 21, 2022. Accessed November 10, 2022, at: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
- National Cancer Grid. India. National Cancer Grid Breast Cancer Management Guidelines, September, 2019. Accessed March 19, 2022, at: https://tmc.gov.in/ncg/docs/PDF/DraftGuidelines/Breast/NCG_guidelines_2019_Breast.pdf - Google Search
- Algorithm for Breast Imaging - Breast Imaging Society. India. Accessed March 19, 2022, at: https://www.bisi.co.in/guidelines/algorithm-for-breast-imaging/
- Kalli S, Semine A, Cohen S, Naber SP, Makim SS, Bahl M. American Joint Committee on Cancer's Staging System for breast cancer, eighth edition: what the radiologist needs to know. Radiographics 2018; 38 (07) 1921-1933
- Teichgraeber DC, Guirguis MS, Whitman GJ. Breast cancer staging: Updates in the AJCC cancer staging manual, 8th edition, and current challenges for radiologists, from the AJR special series on cancer staging. Am J Roentgenol 2021; 217 (02) 278-290
- Chang JM, Leung JWT, Moy L, Ha SM, Moon WK. Axillary nodal evaluation in breast cancer: state of the art. Radiology 2020; 295 (03) 500-515
- van Nijnatten TJA, Jochelson MS, Lobbes MBI. Axillary lymph node characteristics in breast cancer patients versus post-COVID-19 vaccination: overview of current evidence per imaging modality. Eur J Radiol 2022; 152: 110334
- Pesapane F, Downey K, Rotili A, Cassano E, Koh D-M. Imaging diagnosis of metastatic breast cancer. Insights Imaging 2020; 11 (01) 79
- Barra FR, Sobrinho AB, Barra RR. et al. Contrast-enhanced mammography (CEM) for detecting residual disease after neoadjuvant chemotherapy: a comparison with breast magnetic resonance imaging (MRI). BioMed Res Int 2018; 2018: 8531916
- Holmes D, Colfry A, Czerniecki B. et al. Performance and practice guideline for the use of neoadjuvant systemic therapy in the management of breast cancer. Ann Surg Oncol 2015; 22 (10) 3184-3190
- Fowler AM, Mankoff DA, Joe BN. Imaging neoadjuvant therapy response in breast cancer. Radiology 2017; 285 (02) 358-375
- Riedl CC, Pinker K, Ulaner GA. et al. Comparison of FDG-PET/CT and contrast-enhanced CT for monitoring therapy response in patients with metastatic breast cancer. Eur J Nucl Med Mol Imaging 2017; 44 (09) 1428-1437
- Dose Schwarz J, Bader M, Jenicke L, Hemminger G, Jänicke F, Avril N. Early prediction of response to chemotherapy in metastatic breast cancer using sequential 18F-FDG PET. J Nucl Med 2005; 46 (07) 1144-1150
- Janssen NNY, Nijkamp J, Alderliesten T. et al. Radioactive seed localization in breast cancer treatment. Br J Surg 2016; 103 (01) 70-80
- Garzotto F, Comoretto RI, Michieletto S. et al. Preoperative non-palpable breast lesion localization, innovative techniques and clinical outcomes in surgical practice: a systematic review and meta-analysis. Breast 2021; 58: 93-105
- Flowers CI, Mooney BP, Drukteinis JS. Clinical and imaging surveillance following breast cancer diagnosis. Am Soc Clin Oncol Educ Book 2012; •••: 59-64
- Brennan S, Liberman L, Dershaw DD, Morris E. Breast MRI screening of women with a personal history of breast cancer. AJR Am J Roentgenol 2010; 195 (02) 510-516
- Kerridge WD, Kryvenko ON, Thompson A, Shah BA. Fat necrosis of the breast: a pictorial review of the mammographic, ultrasound, CT, and MRI findings with histopathologic correlation. Radiol Res Pract 2015; 2015: 613139
- Schrijver WAME, Suijkerbuijk KPM, van Gils CH, van der Wall E, Moelans CB, van Diest PJ. Receptor conversion in distant breast cancer metastases: a systematic review and meta-analysis. J Natl Cancer Inst 2018; 110 (06) 568-580
- Golan O, Amitai Y, Barnea Y, Menes TS. Yield of surveillance magnetic resonance imaging after bilateral mastectomy and reconstruction: a retrospective cohort study. Breast Cancer Res Treat 2019; 174 (02) 463-468
- Osei EK, Faulkner K. Fetal doses from radiological examinations. Br J Radiol 1999; 72 (860) 773-780
- Sechopoulos I, Suryanarayanan S, Vedantham S, D'Orsi CJ, Karellas A. Radiation dose to organs and tissues from mammography: Monte Carlo and phantom study. Radiology 2008; 246 (02) 434-443
- Committee Opinion No. Committee opinion no. 723: guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol 2017; 130 (04) e210-e216
- Özmen V. Paradigm shift from Halstedian radical mastectomy to personalized medicine. J Breast Health 2017; 13 (02) 50-53
- Parmar V, Koppiker CB, Dixit S. Breast conservation surgery & oncoplasty in India – current scenario. Indian J Med Res 2021; 154 (02) 221-228
- Berruti A, Amoroso V, Gallo F. et al. Pathologic complete response as a potential surrogate for the clinical outcome in patients with breast cancer after neoadjuvant therapy: a meta-regression of 29 randomized prospective studies. J Clin Oncol 2014; 32 (34) 3883-3891
- Burstein HJ, Lacchetti C, Anderson H. et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol 2019; 37 (05) 423-438
- Schmid P, Cortes J, Pusztai L. et al; KEYNOTE-522 Investigators. Pembrolizumab for early triple-negative breast cancer. N Engl J Med 2020; 382 (09) 810-821
- Emens LA, Adams S, Barrios CH. et al. First-line atezolizumab plus nab-paclitaxel for unresectable, locally advanced, or metastatic triple-negative breast cancer: IMpassion130 final overall survival analysis. Ann Oncol 2021; 32 (08) 983-993
- Masuda N, Lee S-J, Ohtani S. et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med 2017; 376: 2147-2159
- Abraham G, Noronha V, Rajappa S. et al. The clinical utility and safety of short-course immune checkpoint inhibitors in multiple tumours-A real-world multicentric study from India. Int J Cancer 2022; 150 (06) 1045-1052
- Bajpai J, Ventrapati P, Joshi S. et al. Unique challenges and outcomes of young women with breast cancers from a tertiary care cancer centre in India. Breast 2021; 60: 177-184
- Bajpai J, Simha V, Shylasree TS. et al. Pregnancy associated breast cancer (PABC): Report from a gestational cancer registry from a tertiary cancer care centre, India. Breast 2021; 56: 88-95
- Bajpai J, Kagwade S, Chandrasekharan A. et al. “Randomised controlled trial of scalp cooling for the prevention of chemotherapy induced alopecia”. Breast 2020; 49: 187-193
- Darby S, McGale P, Correa C. et al; Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 2011; 378 (9804): 1707-1716
- Clarke M, Collins R, Darby S. et al; Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005; 366 (9503): 2087-2106
- Bartelink H, Horiot JC, Poortmans PM. et al. Impact of a higher radiation dose on local control and survival in breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost EORTC 22881-10882 trial. J Clin Oncol 2007; 25 (22) 3259-3265
- Polgár C, Major T, Fodor J. et al. Accelerated partial-breast irradiation using high-dose-rate interstitial brachytherapy: 12-year update of a prospective clinical study. Radiother Oncol 2010; 94 (03) 274-279
- Meattini I, Marrazzo L, Saieva C. et al. Accelerated partial-breast irradiation compared with whole-breast irradiation for early breast cancer: long-term results of the randomized phase III APBI-IMRT-Florence trial. J Clin Oncol 2020; 38 (35) 4175-4183
- Bertrand AS, Iannessi A, Natale R. et al. Focused ultrasound for the treatment of bone metastases: effectiveness and feasibility. J Ther Ultrasound 2018; 6 (01) 8
- Tuncali K, Morrison PR, Winalski CS. et al. MRI-guided percutaneous cryotherapy for soft-tissue and bone metastases: initial experience. AJR Am J Roentgenol 2007; 189 (01) 232-239
- Wallace AN, Greenwood TJ, Jennings JW. Use of imaging in the management of metastatic spine disease with percutaneous ablation and vertebral augmentation. AJR AM J Roentgenol 2015; 205 (02) 434-441


 PDF
PDF  Views
Views  Share
Share

