Hepatic Pseudolesion due to “Vein of Sappey” in Superior Vena Cava Syndrome
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(01): 62-64
DOI: DOI: 10.4103/ijmpo.ijmpo_125_16
Abstract
One of the common causes of superior vena cava (SVC) syndrome is malignancy of the lung. The invasion of SVC leads to opening of the various venous channels for continuation of the blood flow from upper extremity and proximal trunk and finally draining into right atrium. Vein of Sappey is one of these channels and it causes focal striking enhancement in segment IV of the liver on arterial phase of contrast computed tomography (CT). This enhancement causes diagnostic difficulty and unnecessary biopsy due to misinterpretation of it as a secondary from lung cancer. Awareness and accurate diagnosis can avoid further examination in such patients. It can also provide an idea of a more proximal major thoracic vessel obstruction iffirst detected on CT of the abdomen (contrast).
Publication History
Article published online:
06 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
One of the common causes of superior vena cava (SVC) syndrome is malignancy of the lung. The invasion of SVC leads to opening of the various venous channels for continuation of the blood flow from upper extremity and proximal trunk and finally draining into right atrium. Vein of Sappey is one of these channels and it causes focal striking enhancement in segment IV of the liver on arterial phase of contrast computed tomography (CT). This enhancement causes diagnostic difficulty and unnecessary biopsy due to misinterpretation of it as a secondary from lung cancer. Awareness and accurate diagnosis can avoid further examination in such patients. It can also provide an idea of a more proximal major thoracic vessel obstruction if first detected on CT of the abdomen (contrast).
Introduction
Hepatic pseudolesion forms an important group of hepatic lesions due to altered hemodynamic. We have come across a case of superior vena cava syndrome (SVCS) causing pseudolesion in segment IV of the liver. The superior vena cava (SVC) obstruction in this case was due to bronchogenic carcinoma and the pseudolesion mimicked a secondary. If not diagnose accurately, it may lead to a liver biopsy for confirmation; therefore, recognition of this lesion is essential.
Case Report
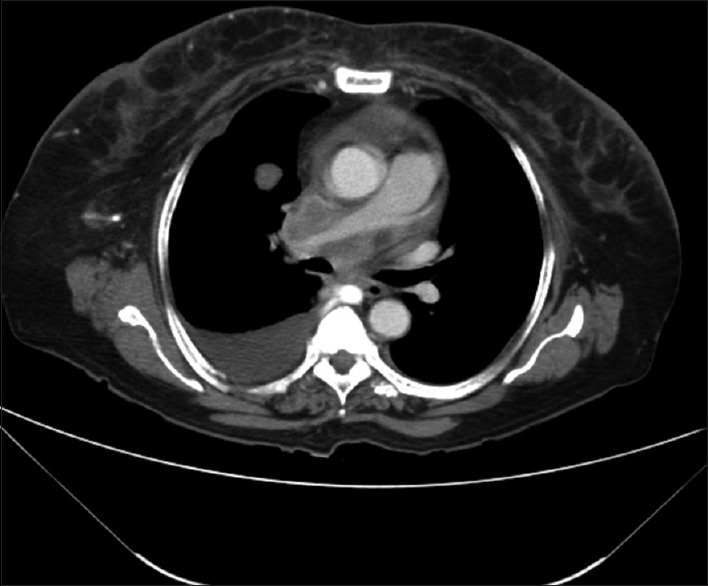
A 50-year-old female patient presented with dyspnea, chest pain for a duration of 8 months and was not responding to antibiotic therapy. A chest X-ray was advised which revealed a rounded nodular opacity in the right lung [Figure 1]. Considering the age of the patient, possibility of malignancy was considered and the patient was further investigated with computed tomography (CT) of the thorax. CT revealed heterogenous enhancing lobulated mass in the superior mediastinum compressing and occluding the SVC [Figure 2]. The SCV was not opacified. Right middle lobe bronchus revealed cutoff sign with a moderately enhancing mass [Figure 3]. There were pleural and pericardial deposits along with right pleural effusion. The metastatic mediastinal lymphadenopathy was encasing the right pulmonary artery [Figure 4]. Multiple chest wall and suprascapular collaterals, vascular collaterals were present. Liver examination on plain CT of the abdomen scan showed no obvious lesion. On arterial phase, a wedge-shaped hyperattenuated area in segment IV A [Figure 5] was seen. This finding was not visualized in venous or delayed phases. In view of SCV obstruction and a wedge-shaped intensly enhancing hepatic lesion, a possibility of a pseudolesion secondary to opening of the collateral channels through vein of Sappey was considered. The patient was further followed up with liver function test and ultrasonography. There was no evidence of any lesion on ultrasonography. Biopsy of the thoracic lesion turned to be bronchogenic carcinoma with mediastinal spread.
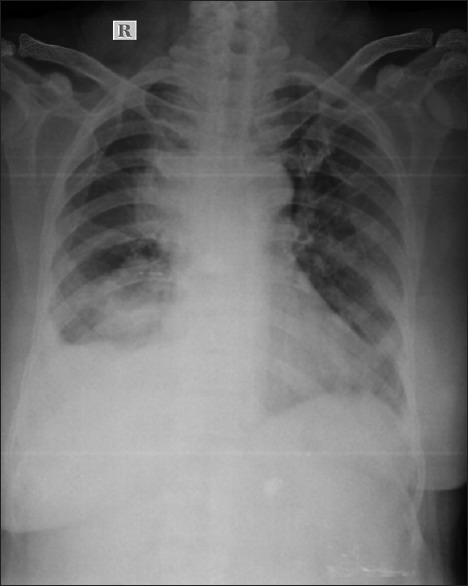
| Figure 1Chest X-ray showing two large nodular opacities along the right heart border
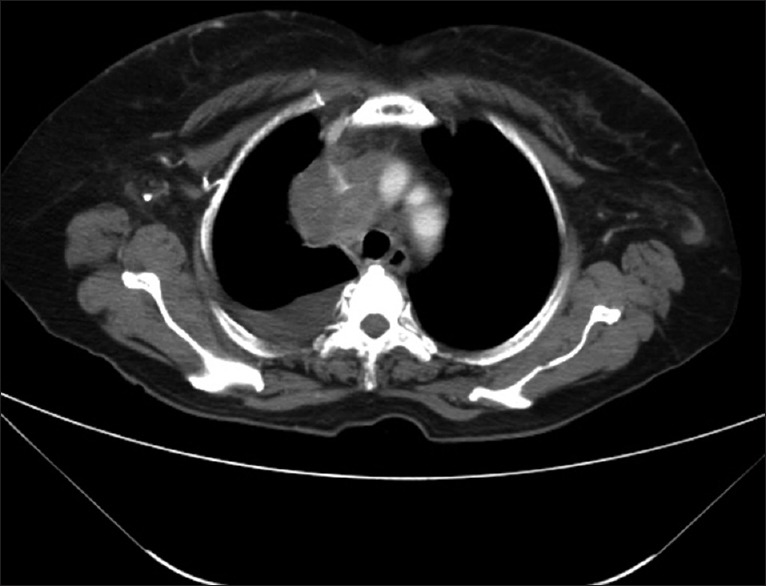
| Figure 2Axial computed tomography of the thorax (mediastinal window) revealed heterogenous enhancing lobulated mass in superior mediastinum compressing and occluding the superior vena cava
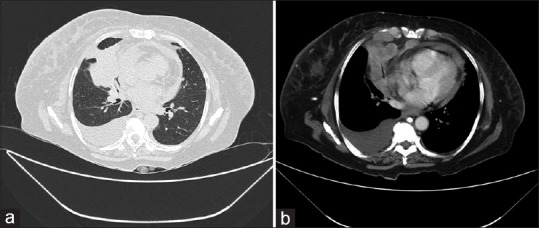
| Figure 3Axial computed tomography of the thorax (a) lung window (b) mediastinal window showing a right middle lobe bronchus cutoff sign due to a moderately enhancing mass. Pleural and pericardial deposits along with right pleural effusion are also seen
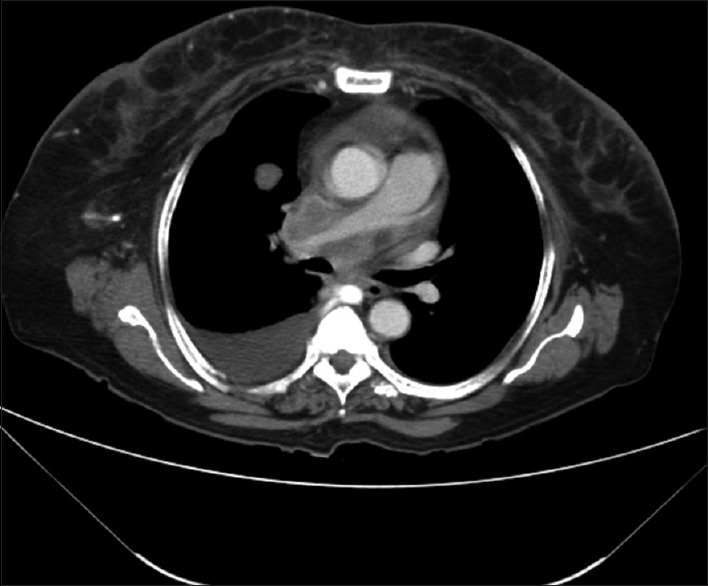
| Figure 4Axial computed tomography of the thorax (mediastinal window) showing metastatic mediastinal lymphadenopathy which is encasing the right pulmonary aorta
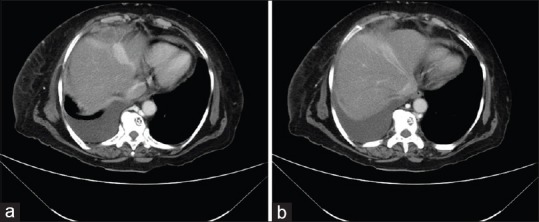
| Figure 5(a and b) Axial computed tomography (arterial phase) showing a wedge-shaped intensly enhancing area in segment IV A
Discussion
SVCS is obstruction of blood flow through the SVC. The important causes of SVCS are malignancy (lung cancer), metastatic spread, inflammation leading to fibrosis and mediastinal masses.[1] In SVCS, different pathway of collaterals has been described in literature.[1] (1) Azygos–hemiazygos–accessory hemiazygos system – If the level of SCV obstruction is above the azygos arch, antegrade flow from the azygos to the right atrium is seen, with abrupt transition between a densely opacified azygos above the arch and a unopacified inferior azygos vein. If the obstruction is below the arch, the entire azygos and hemiazygos veins are brightly opacified as the blood flows in a retrograde fashion toward the inferior vena cava.[2] In our case, we could visualize prominent azygos and hemiazygos veins. (2) Vertebral and subscapular plexuses – Visualization of paravertebral, intervertebral, and epidural veins leading to the azygos system is observed. In our case, a few collaterals in scapular area were present. (3) Mediastinal venous plexus and esophageal venous plexus and diaphragmatic venous plexus – In our case, no esophageal collaterals were seen. (4) Lateral thoracic and superficial thoracoabdominal venous plexuses – The internal thoracic veins and lateral thoracic veins communicate with thoracoepigastric and superficial epigastric veins. Chest wall and breast collateral veins can also brightly opacify as a sign of SCV obstruction. Internal and external mammary pathway includes internal mammary, superficial veins of the thorax, superior and inferior epigastric veins.[3] These specific vascular collateral channels cause pseudolesion in the liver in case of SCV obstruction. Small vein in the falciform ligament draining anterior part of the abdominal wall into the liver will get opacified and will cause pseudolesions. These small veins have three subgroups: Superior and inferior vein of Sappey, vein of Burow.[4] The superior vein of Sappey drains upper part of falciform ligament, medial diaphragm and enters peripheral portal branch of the left hepatic lobe. It communicates with the branches of superior epigastric and internal thoracic veins.[1] In SCV obstruction, blood proximal to obstruction reaches liver through the internal thoracic, superior epigastric, and superior vein of Sappey. When this channel opens up, pseudolesion becomes obvious on CT examination.[5,6] In our case, intensly enhancing area in segment IV was seen.
Recognization of the pseudolesions in the liver is important as it can avoid wrong diagnosis of a hepatic metastasis and further unnecessary biopsy. Furthermore, its detection can direct our thinking about a possible obstruction of proximal major thoracic vessels.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Sheth S, Ebert MD, Fishman EK. Superior vena cava obstruction evaluation with MDCT. AJR Am J Roentgenol 2010;194:W336-46.
- Gosselin MV, Rubin GD. Altered intravascular contrast material flow dynamics: Clues for refining thoracic CT diagnosis. AJR Am J Roentgenol 1997;169:1597-603.
- Al Mane KA, Al Maziad GA, Al Wabil AS. Pseudolesion in left lobe of the liver due to superior vena cava obstruction. Saudi Med J 2001;22:74-5.
- Martin BF, Tudor RG. The umbilical and paraumbilical veins of man. J Anat 1980;130 Pt 2:305-22.
- Dahan H, Arrivé L, Monnier-Cholley L, Le Hir P, Zins M, Tubiana JM. Cavoportal collateral pathways in vena cava obstruction: Imaging features. AJR Am J Roentgenol 1998;171:1405-11.
- Tetalman MR, Kusumi R, Gaughran G, Baba N. Radionuclide liver spots: Indicator of liver disease or a blood flow phenomenon. AJR Am J Roentgenol 1978;130:291-6.
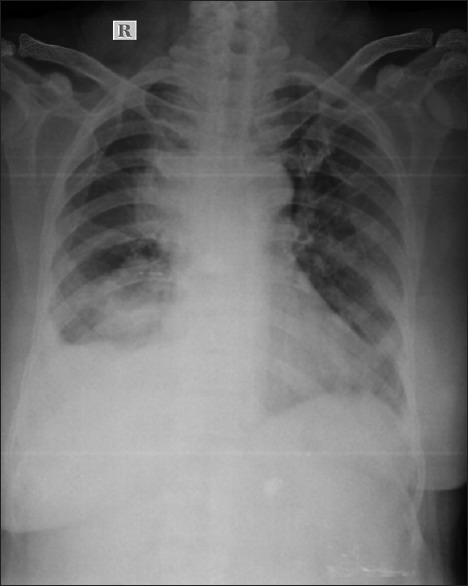
| Figure 1Chest X-ray showing two large nodular opacities along the right heart border
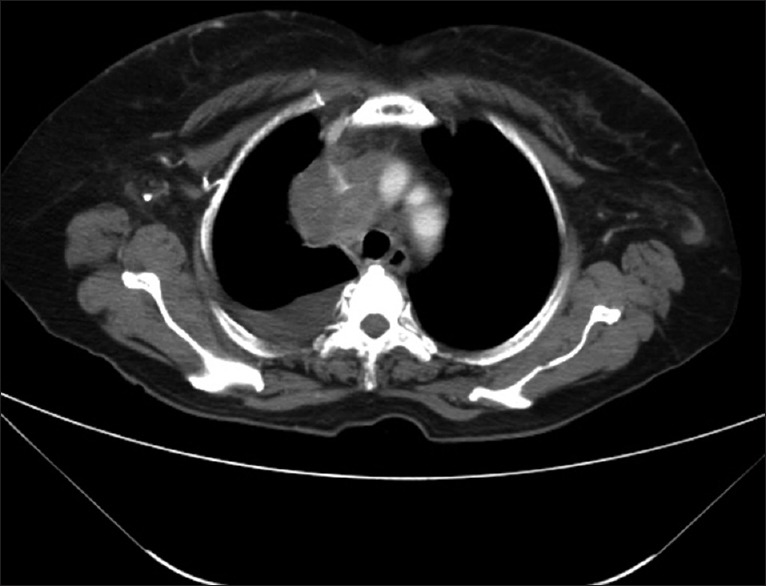
| Figure 2Axial computed tomography of the thorax (mediastinal window) revealed heterogenous enhancing lobulated mass in superior mediastinum compressing and occluding the superior vena cava
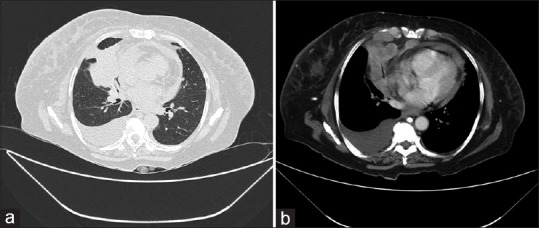
| Figure 3Axial computed tomography of the thorax (a) lung window (b) mediastinal window showing a right middle lobe bronchus cutoff sign due to a moderately enhancing mass. Pleural and pericardial deposits along with right pleural effusion are also seen
| Figure 4Axial computed tomography of the thorax (mediastinal window) showing metastatic mediastinal lymphadenopathy which is encasing the right pulmonary aorta
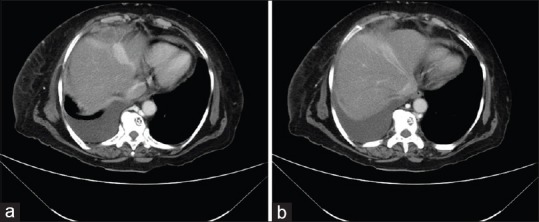
| Figure 5(a and b) Axial computed tomography (arterial phase) showing a wedge-shaped intensly enhancing area in segment IV A
References
- Sheth S, Ebert MD, Fishman EK. Superior vena cava obstruction evaluation with MDCT. AJR Am J Roentgenol 2010;194:W336-46.
- Gosselin MV, Rubin GD. Altered intravascular contrast material flow dynamics: Clues for refining thoracic CT diagnosis. AJR Am J Roentgenol 1997;169:1597-603.
- Al Mane KA, Al Maziad GA, Al Wabil AS. Pseudolesion in left lobe of the liver due to superior vena cava obstruction. Saudi Med J 2001;22:74-5.
- Martin BF, Tudor RG. The umbilical and paraumbilical veins of man. J Anat 1980;130 Pt 2:305-22.
- Dahan H, Arrivé L, Monnier-Cholley L, Le Hir P, Zins M, Tubiana JM. Cavoportal collateral pathways in vena cava obstruction: Imaging features. AJR Am J Roentgenol 1998;171:1405-11.
- Tetalman MR, Kusumi R, Gaughran G, Baba N. Radionuclide liver spots: Indicator of liver disease or a blood flow phenomenon. AJR Am J Roentgenol 1978;130:291-6.


 PDF
PDF  Views
Views  Share
Share

