Giant velum interpositum meningioma in a child
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2012; 33(03): 173-175
DOI: DOI: 10.4103/0971-5851.103147
Abstract
Intraventricular meningiomas are rare, but are relatively more often seen in children. Large size at presentation often obscures anatomical details. A particular subset of such tumors arising from the velum interpositum pose a significant surgical challenge. Thorough preoperative imaging, especially with respect to the course of the deep venous structures, provides useful evidence as to the origin. Preservation of venous anatomy at surgery is vital. We describe a 3-year-old girl with a giant velum interpositum meningioma that was completely excised with excellent outcome. This is probably the youngest such case reported.
Keywords
Childhood brain tumor - intraventricular meningioma - pineal meningioma - velum interpositumPublication History
Article published online:
02 August 2021
© 2012. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Intraventricular meningiomas are rare, but are relatively more often seen in children. Large size at presentation often obscures anatomical details. A particular subset of such tumors arising from the velum interpositum pose a significant surgical challenge. Thorough preoperative imaging, especially with respect to the course of the deep venous structures, provides useful evidence as to the origin. Preservation of venous anatomy at surgery is vital. We describe a 3-year-old girl with a giant velum interpositum meningioma that was completely excised with excellent outcome. This is probably the youngest such case reported.
INTRODUCTION
Intraventricular meningiomas are rare. However, they are relatively more often seen in children.[1] Most often, these arise from the lateral ventricular walls. Meningiomas of the velum interpositum are extremely unusual and difficult to diagnose.[2] These arise from the arachnoid cap cells within the potential space of the velum interpositum and lack a dural attachment. They usually present as pineal or posterior third ventricular masses. We encountered one such case where the massive size obscured all anatomical information and the site of origin was only established at surgery. We discuss this case and review the relevant literature.
CASE REPORT
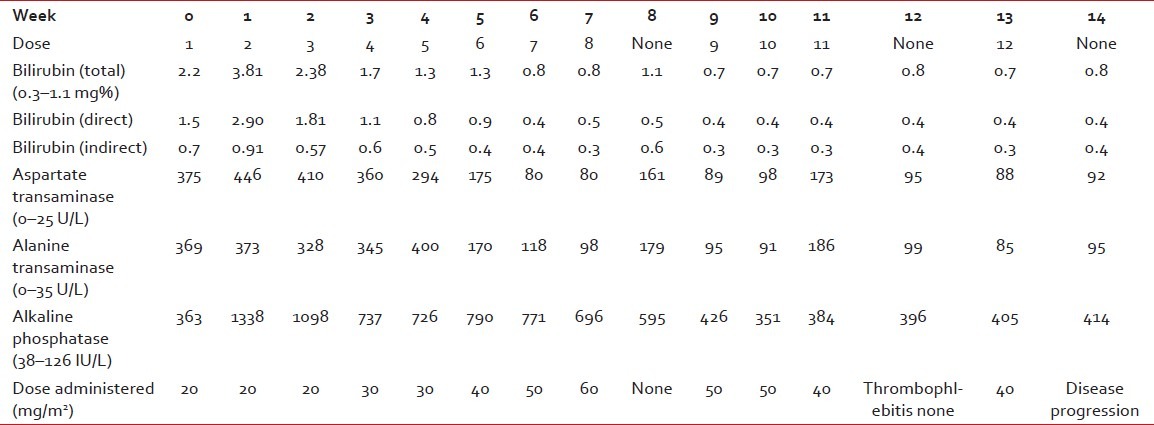
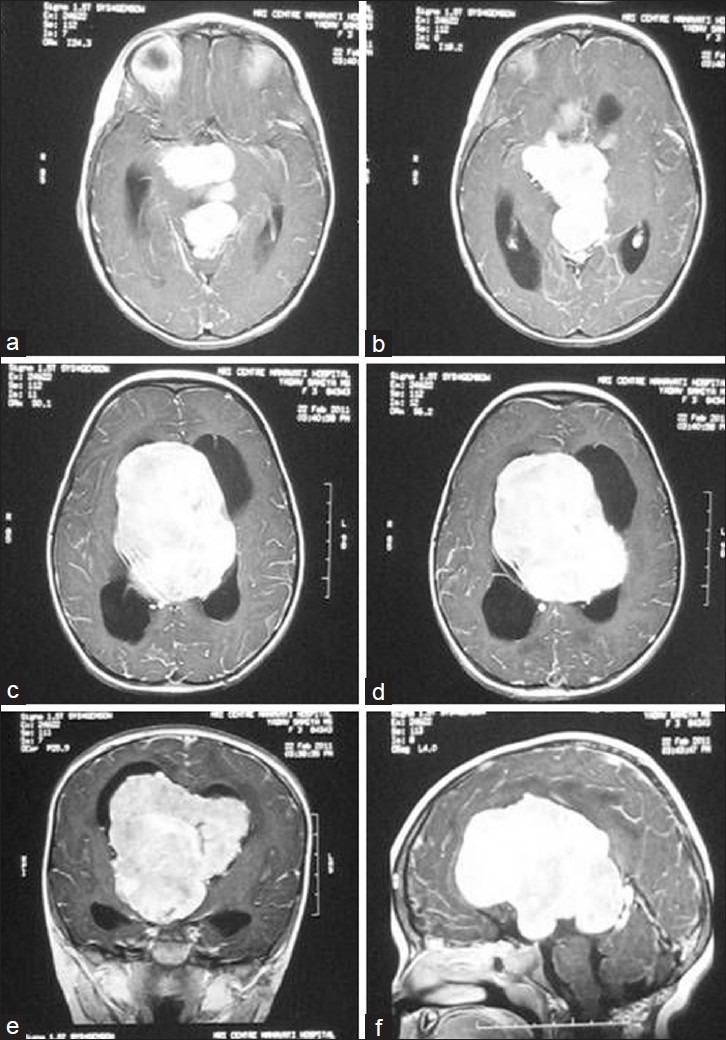
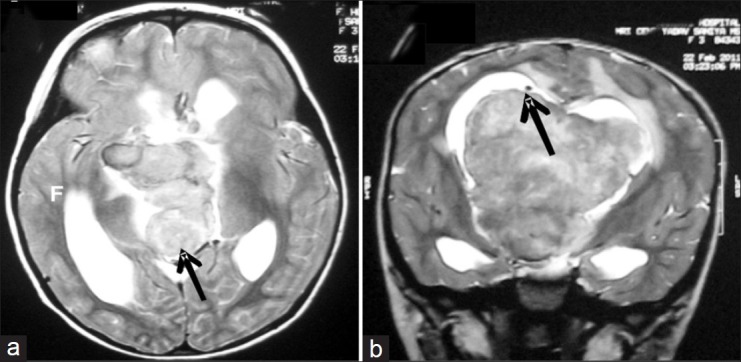
A 3-year-old girl presented with history of difficulty in walking since 2 months. She had a normal perinatal history and developmental milestones until the current symptoms. On examination, she had papilledema. There was asymmetric spastic quadriparesis (left worse than right). The computed tomography (CT) head [Figure 1] revealed a large hyperdense uniformly enhancing lesion occupying the intraventricular space (bilateral lateral as well as third ventricles) with a thin rim of calcification. On magnetic resonance (MR) imaging [Figure 2], the lesion appeared isointense on T1, mildly hypointense on T2 and showed uniform enhancement. There was no dural tail or enhancement. The internal cerebral veins (ICV) appeared stretched out and displaced laterally and the cerebral peduncles were splayed [Figure 3]. Because of the asymmetric extension into the right frontal horn, a transcortical, transventricular approach was taken. The tumor was identified in the medial wall of the right lateral ventricle under the septal wall, which was stretched over it. It was firm, fibrous and minimally vascular. Gradual internal debulking revealed the location of the tumor entirely within the third ventricle, displacing the internal cerebral veins around it laterally. These were carefully dissected and preserved. Within the third ventricle (which was grossly dilated), the tumor occupied all the recesses. The tumor lobules could be delivered free from all the recesses except in the region of the pineal recess where there was dense adherence to the confluence of the great veins extending into what would have been the potential space of the velum interpositum. In the absence of any other site of attachment, this was most likely the site of origin of the tumor. The tumor was removed gross, totally shaving it off the great veins. An external ventricular drain was placed before closure. The intraoperative blood loss was 400 mL. Postoperatively, the child recovered well. The external ventricular drain was gradually clamped and removed. On the fourth postoperative day, she became drowsy. The drain cerebrospinal fluid revealed growth of Acinetobacter baumannii and, on commencing antibiotic therapy with meropenem, she improved remarkably. The postoperative MRI [Figure 4] revealed no residual tumor. The deep venous system was intact on the venography [Figure 5]. There was a small area of ischemia in the anterior commissure on the right side. She subsequently had an uneventful course and was discharged on the 14th postoperative day after completing a 10-day course of antibiotics, with minimal residual left hemiparesis. The histopathology revealed a transitional meningioma (WHO grade I) and she was advised a regular clinical follow-up.
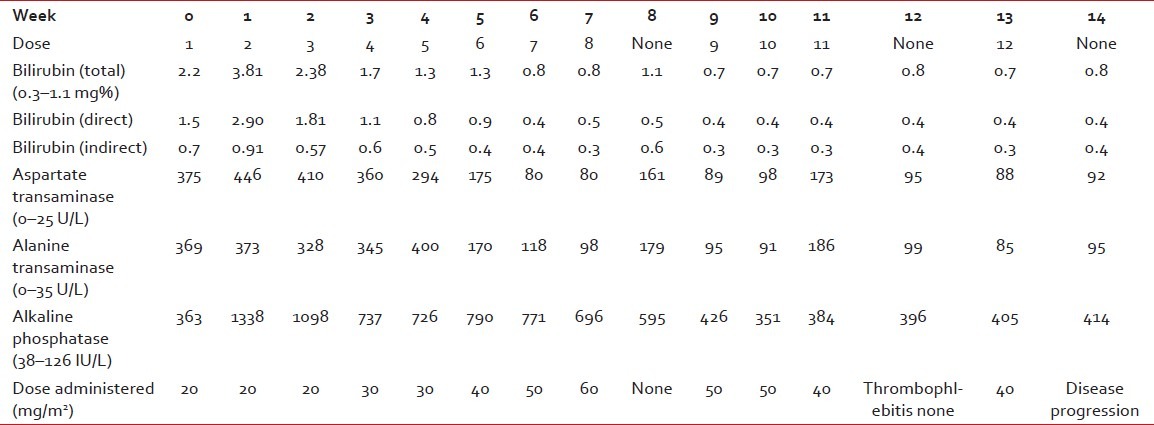
| Fig. 1 Preoperative computed tomography (plain – a and b; contrast enhanced – c and f) showing a hyperdense intraventricular tumor with uniform and brilliant contrast enhancement
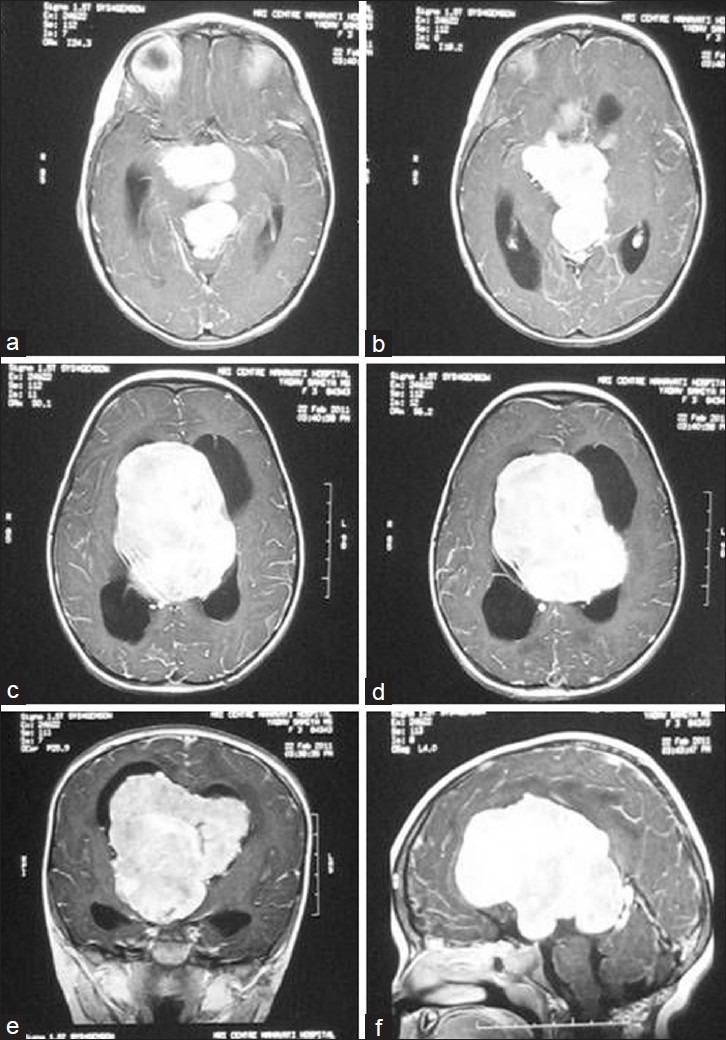
| Fig. 2 Preoperative gadolinium-enhanced T1-weighted magnetic resonance images (axial – a–d; coronal – e; sagittal – f) showing the enhancing tumor occupying the third ventricle with lobules extending into its various recesses
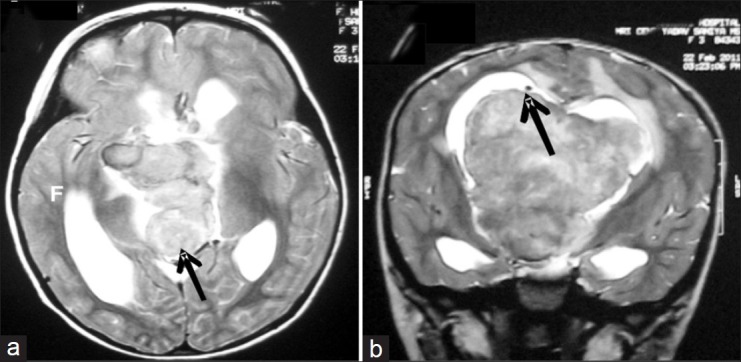
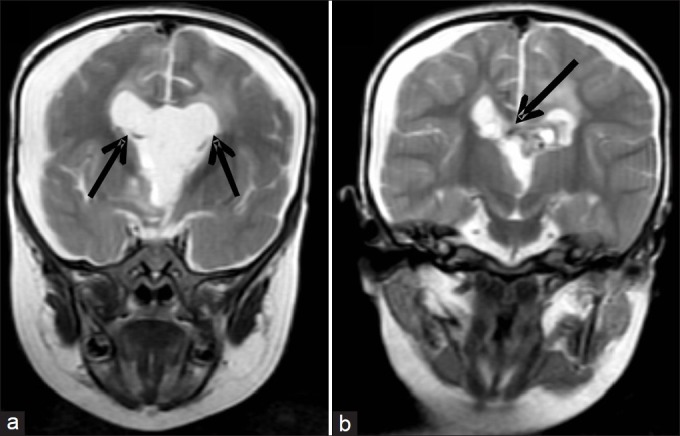
| Fig. 3 Preoperative T2-weighted (axial – a; coronal – b) images showing the tumor in the pineal recess splaying the internal cerebral veins and their confluence (black arrows)
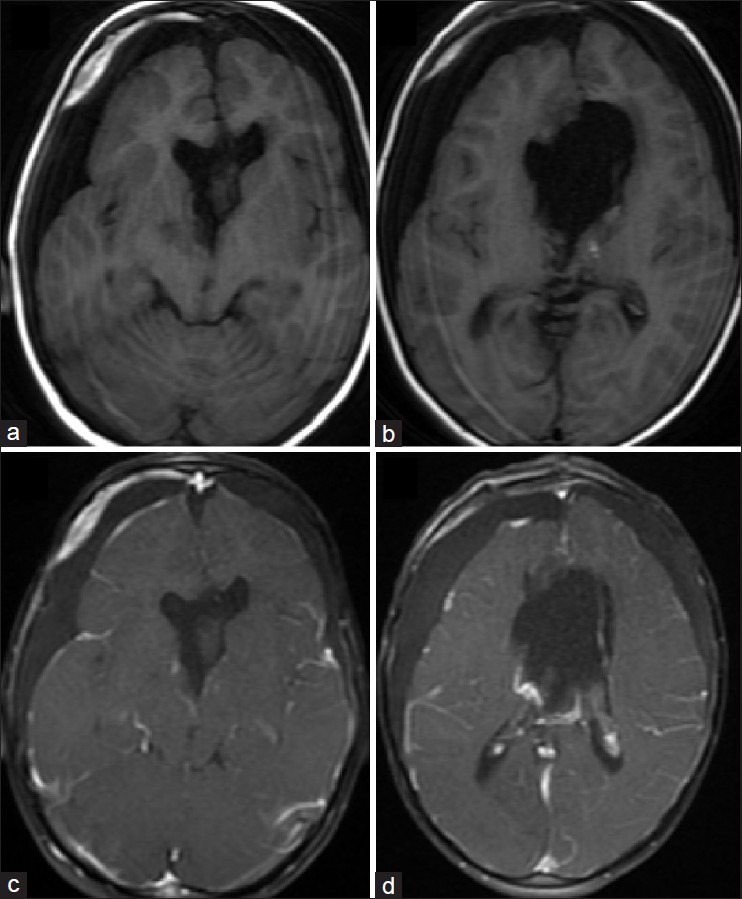
| Fig. 4 Postoperative magnetic resonance (T1 weighted – a and b; postgadolinium T1 weighted – c and d) showing complete excision
| Fig. 5 Postoperative T2-weighted images (coronal) showing the preserved internal cerebral veins (black arrows)
DISCUSSION
ALthough meningiomas are common in adults, they constitute less than 5% of childhood central nervous system tumors.[1] Among the intracranial meningiomas, the intraventricular location is exceedingly rare (less than 1%).[3,4] However, intraventricular meningiomas are relatively more common in children.[5] The most common site for intraventricular tumors is the lateral ventricle. The third ventricle is rarely the primary site of origin. Often, due to the large size of these tumors, it becomes very difficult to ascertain the exact site of origin. These tumors are divided into anterior third ventricular meningiomas without dural attachment, which may arise from the tela choroidea in the roof or rarely from the floor of the third ventricle, and posterior third ventricular tumors arising from the posterior tela choroidea and the tenia fornicis in the velum interpositum.[2] This latter group is rare and has been called velum interpositum meningiomas.[2] This category also falls into the group of pineal region meningiomas. Meningiomas of the pineal region are again rare[6] and often include tumors having a dural base along the falcotentorial junction.
True meningiomas of the velum interpositum (without any dural involvement) are indeed exceedingly uncommon. Radiologically, they may mimic any third ventricular or pineal region tumor depending on the exact site of origin and direction of growth. Giant intraventricular meningiomas are often seen in childhood, just as in our case, and this may obscure all anatomical imaging clues as to the site of origin. Lozier et al.[2] described 17 cases of meningiomas of the velum interpositum. Of these, only three were in children, all more than 5 years of age.[7–9] Our case is probably the youngest such case reported.
ALthough Lozier et al.[2] describe radiological imaging features (especially the course of the internal cerebral veins) in preoperatively differentiating these tumors, the information may not always be forthcoming and, even when available, may not always help differentiate them from other intraventricular meningiomas. What is however critical is to appreciate the venous anatomy (which may be grossly distorted) and preserve the veins during surgery. The surgical approach is dictated by the location and extent of the lesion. We selected the transcortical transventricular transchoroidal approach to the tumor as has been described for safe entry into velum interpositum,[10] because the tumor had extended significantly into the lateral ventricles. Although we were not sure of the site of origin a priori, following the anatomy and gradually debulking the tumor led us to the site. We were able to identify and preserve the internal cerebral veins as was apparent in the postoperative MRI as well as trace the origin of the tumor to the dense fibrous tissue at the confluence of the great veins. Preservation of the deep venous system is crucial and complications can often be fatal. Although challenging, complete surgical excision is curative for the grade I lesions, and should be attempted. Recovery is often uneventful (and satisfying) if the deep venous structures are preserved.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
REFERENCES
| Fig. 1 Preoperative computed tomography (plain – a and b; contrast enhanced – c and f) showing a hyperdense intraventricular tumor with uniform and brilliant contrast enhancement
| Fig. 2 Preoperative gadolinium-enhanced T1-weighted magnetic resonance images (axial – a–d; coronal – e; sagittal – f) showing the enhancing tumor occupying the third ventricle with lobules extending into its various recesses
| Fig. 3 Preoperative T2-weighted (axial – a; coronal – b) images showing the tumor in the pineal recess splaying the internal cerebral veins and their confluence (black arrows)
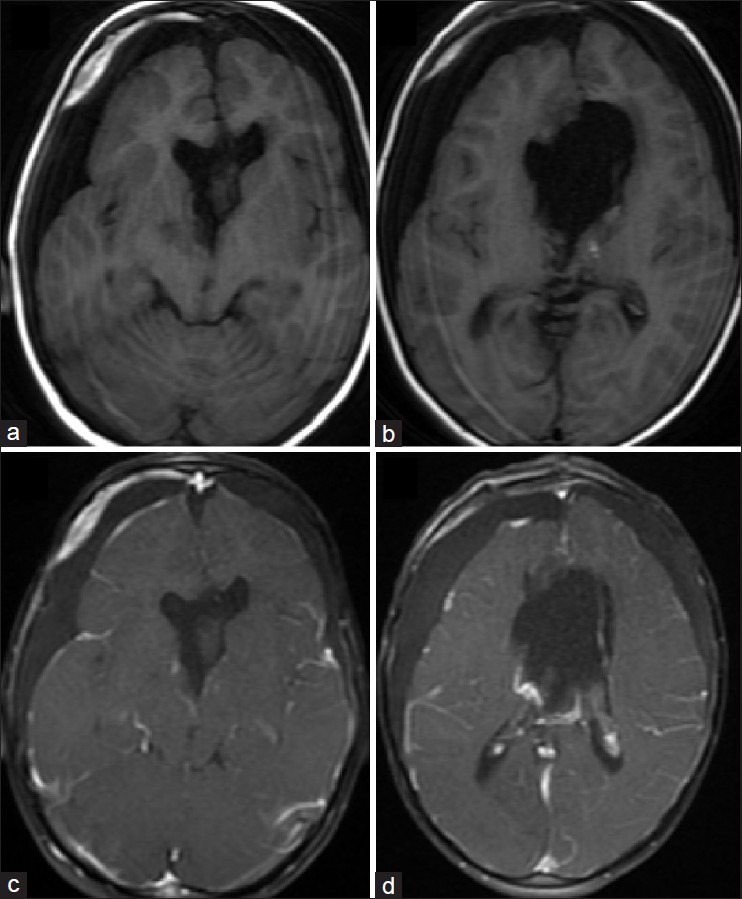
| Fig. 4 Postoperative magnetic resonance (T1 weighted – a and b; postgadolinium T1 weighted – c and d) showing complete excision
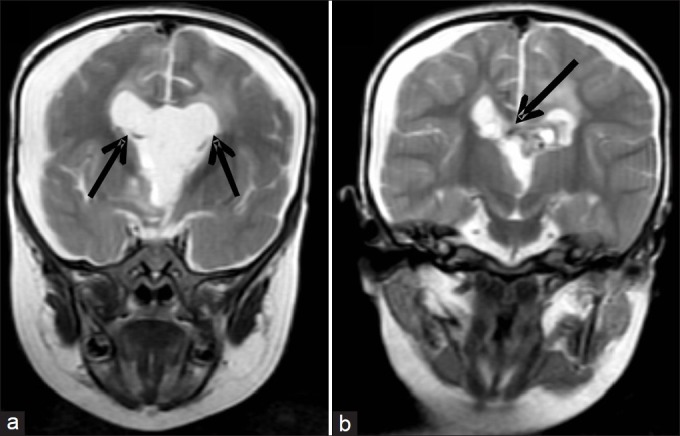
| Fig. 5 Postoperative T2-weighted images (coronal) showing the preserved internal cerebral veins (black arrows)


 PDF
PDF  Views
Views  Share
Share

