Geriatric oncology: The need for a separate subspecialty
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2012; 33(02): 134-136
DOI: DOI: 10.4103/0971-5851.99755
Publication History
Article published online:
13 April 2022
© 2012. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
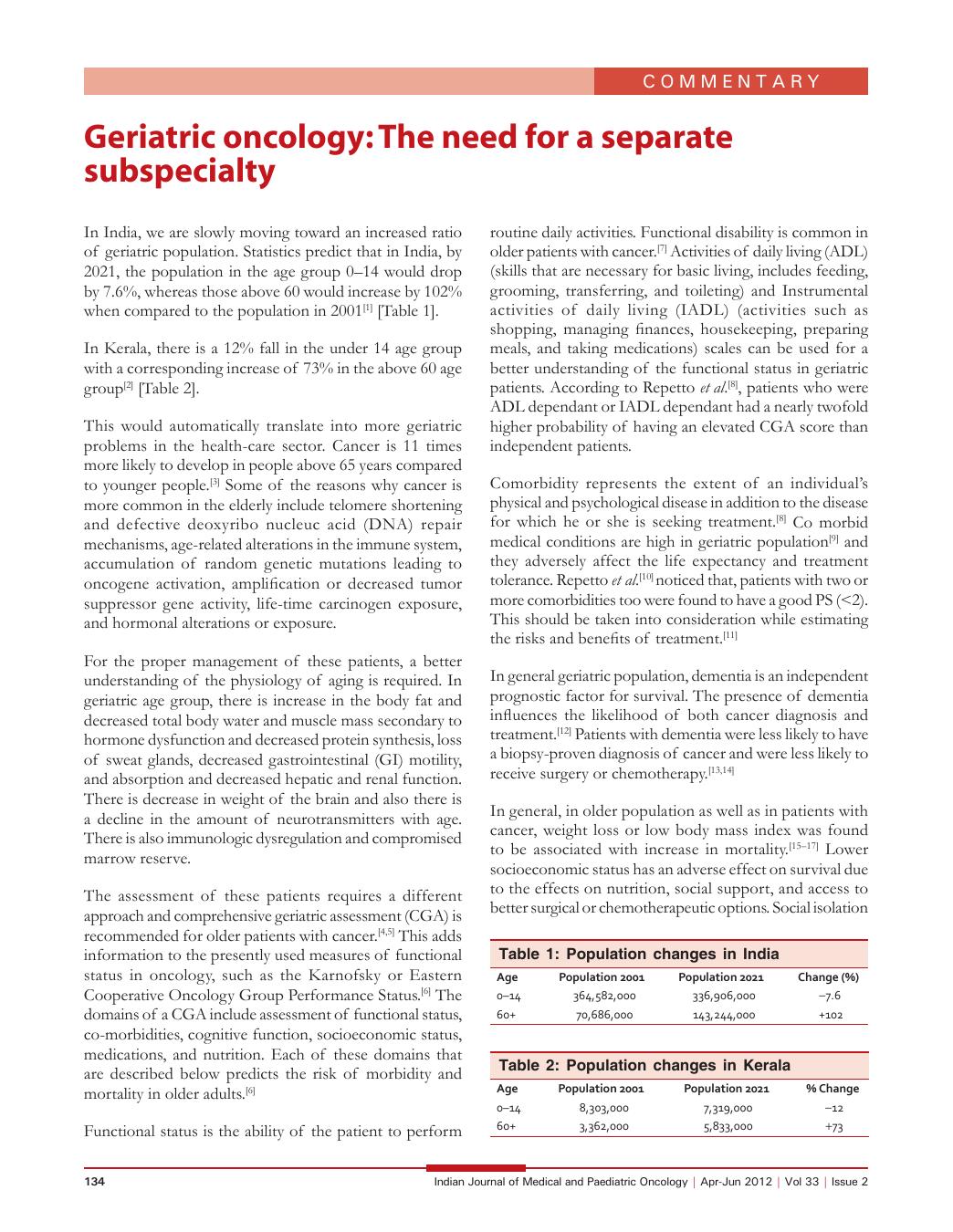
In India, we are slowly moving toward an increased ratio of geriatric population. Statistics predict that in India, by 2021, the population in the age group 0–14 would drop by 7.6%, whereas those above 60 would increase by 102% when compared to the population in 2001[1] [Table 1].
Table 1
Population changes in India
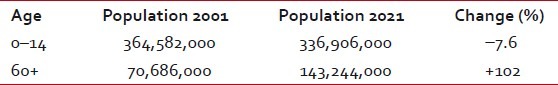
In Kerala, there is a 12% fall in the under 14 age group with a corresponding increase of 73% in the above 60 age group[2] [Table 2].
Table 2
Population changes in Kerala
This would automatically translate into more geriatric problems in the health-care sector. Cancer is 11 times more likely to develop in people above 65 years compared to younger people.[3] Some of the reasons why cancer is more common in the elderly include telomere shortening and defective deoxyribo nucleuc acid (DNA) repair mechanisms, age-related alterations in the immune system, accumulation of random genetic mutations leading to oncogene activation, amplification or decreased tumor suppressor gene activity, life-time carcinogen exposure, and hormonal alterations or exposure.
For the proper management of these patients, a better understanding of the physiology of aging is required. In geriatric age group, there is increase in the body fat and decreased total body water and muscle mass secondary to hormone dysfunction and decreased protein synthesis, loss of sweat glands, decreased gastrointestinal (GI) motility, and absorption and decreased hepatic and renal function. There is decrease in weight of the brain and also there is a decline in the amount of neurotransmitters with age. There is also immunologic dysregulation and compromised marrow reserve.
The assessment of these patients requires a different approach and comprehensive geriatric assessment (CGA) is recommended for older patients with cancer.[4,5] This adds information to the presently used measures of functional status in oncology, such as the Karnofsky or Eastern Cooperative Oncology Group Performance Status.[6] The domains of a CGA include assessment of functional status, co-morbidities, cognitive function, socioeconomic status, medications, and nutrition. Each of these domains that are described below predicts the risk of morbidity and mortality in older adults.[6]
Functional status is the ability of the patient to perform routine daily activities. Functional disability is common in older patients with cancer.[7] Activities of daily living (ADL) (skills that are necessary for basic living, includes feeding, grooming, transferring, and toileting) and Instrumental activities of daily living (IADL) (activities such as shopping, managing finances, housekeeping, preparing meals, and taking medications) scales can be used for a better understanding of the functional status in geriatric patients. According to Repetto et al.[8] , patients who were ADL dependant or IADL dependant had a nearly twofold higher probability of having an elevated CGA score than independent patients.
Comorbidity represents the extent of an individual's physical and psychological disease in addition to the disease for which he or she is seeking treatment.[8] Co morbid medical conditions are high in geriatric population[9] and they adversely affect the life expectancy and treatment tolerance. Repetto et al.[10] noticed that, patients with two or more comorbidities too were found to have a good PS ( < 2). This should be taken into consideration while estimating the risks and benefits of treatment.[11]
In general geriatric population, dementia is an independent prognostic factor for survival. The presence of dementia influences the likelihood of both cancer diagnosis and treatment.[12] Patients with dementia were less likely to have a biopsy-proven diagnosis of cancer and were less likely to receive surgery or chemotherapy.[13,14]
In general, in older population as well as in patients with cancer, weight loss or low body mass index was found to be associated with increase in mortality.[15–17] Lower socioeconomic status has an adverse effect on survival due to the effects on nutrition, social support, and access to better surgical or chemotherapeutic options. Social isolation is also an independent predictor of mortality in the geriatric population.[18] A careful assessment of the medications taken by the patient is necessary to remove any unnecessary medicines and also to look for potential drug interactions.[19–21]
Even though the majority of cancer patients are in the older age group, participation of older patients in cancer treatment trials had been very low. In Canada, it was found that patients who were 65 years or older accounted only for 22% of patients in the National Cancer Institute of Canada Clinical Trials Group compared with 58% of the Canadian population with cancer in 1993–1996.[22] Also in India, the number of older cancer patients enrolled in trials will be much less compared to the other age groups. The enrolment of older people in adjuvant trials was lower than their enrolment in advanced clinical trials. This may be because many older patients present in advanced stage[23–25] and have poor physical condition. It may also be due to reluctance on the part of the physicians or patients to enroll in adjuvant trials.[22] But now there are a few randomized controlled trials specifically for the geriatric population, like the Intergroupe Francophone de Cancérologie Thoracique 0501 for advanced nonsmall cell carcinoma of the Lung.[26]
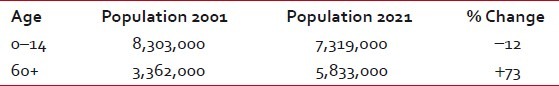
In India, according to registry data about 45–50% of all the cancers in males and 35–41% of all cancer in females occur above the age of 60.[27] The age specific rate of all cancers affecting males and females in India is represented in Figures Figures11 and and22.
| Fig. 1 Age specific rates of cancer in males
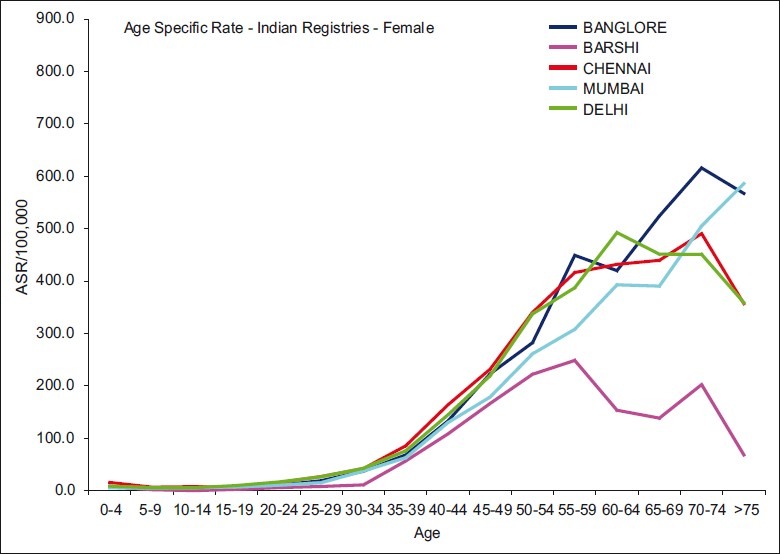
| Fig. 2 Age specific rates of cancer in females
Based on the incidence rates published in the Indian Council of Medical Research population-based cancer registry report[27] and Dindigul Ambilikkai Cancer registry,[28] there will be more than 200,000 males and nearly 150,000 females newly diagnosed as cancer every year in India by 2021. The prevalence of cancer patients in India above the age of 60 is estimated to reach more than 1 million by 2021.
Kerala though a small state, has three population-based cancer registries; two in the rural area and one in the urban area (Trivandrum rural and Karunagapally vs Trivandrum urban).
Based on the incidence rates of Karunagapally and Trivandrum[29,30] it can be estimated that there will be around 20,171 people above 65 years newly diagnosed as cancer every year in Kerala by 2021. In addition, in Kerala the prevalence of cancer patients above the age of 60 is estimated to be more than 60,000 by 2021.
As these patients have special needs and a different approach to treatment, there is a strong case for the emergence of geriatric oncology as a sub specialty in oncology.:
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
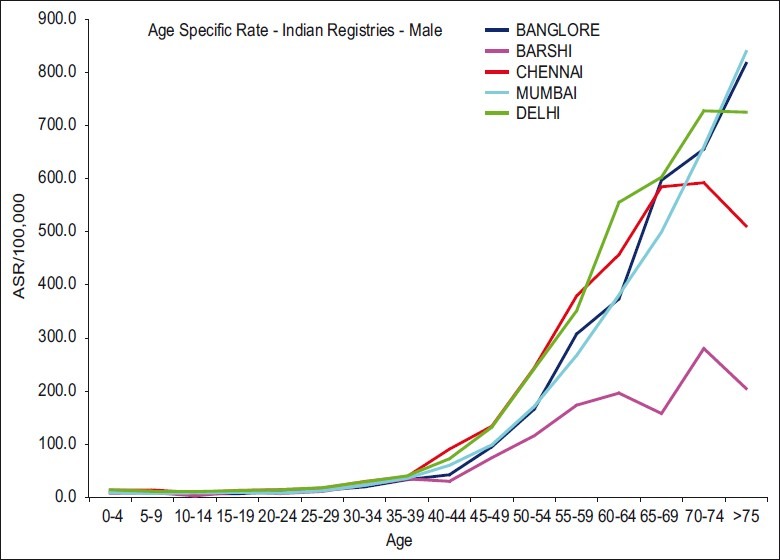
| Fig. 1 Age specific rates of cancer in males
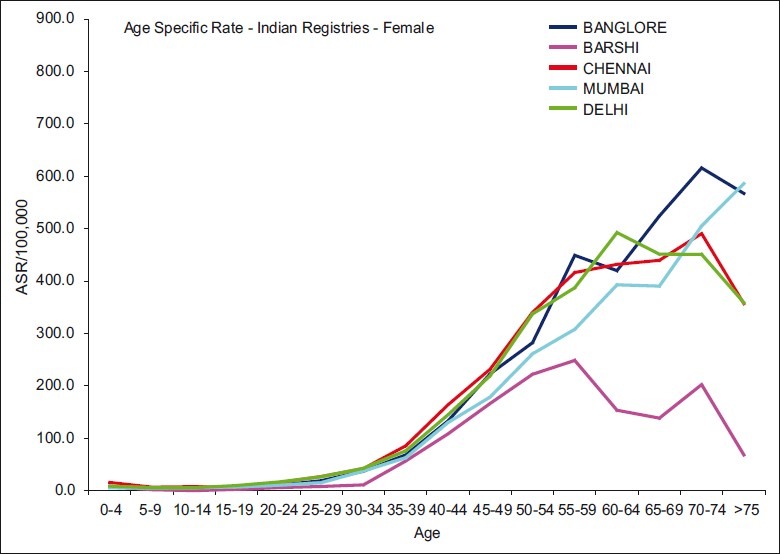
| Fig. 2 Age specific rates of cancer in females


 PDF
PDF  Views
Views  Share
Share

