Financial Burden Faced by Families due to Out of pocket Expenses during the Treatment of their Cancer Children: An Indian Perspective
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(01): 4-9
DOI: DOI: 10.4103/0971-5851.203493
Abstract
Context: Life-saving cancer therapy is costly and may result in financial burden for these families. Financial costs for treating childhood cancer care are traditionally assessed based on the amount spent for diagnostic tests, hospitalization, and chemotherapy. The financial costs for travel, accommodation, out-of-pocket expenses for food, phone bills, and loss of income due to reduction or termination of parental employment are hidden nonmedical expenses that are rarely accounted for. Studies on the financial implications of pediatric cancer treatment are based on the Western model of healthcare with good government/state insurance coverage and hence literature on lifestyle implications for families in developing nations with limited resources is still scarce. Aims: The aim of this study is to find out the details of out-of-pocket expenses incurred by the families during their treatment of cancer children and its implications on their quality of life. Settings and Design: This study was conducted in a tertiary care center for pediatric malignancies for over 1-year period. Subjects and Methods: About seventy families whose children were diagnosed with acute leukemia and undergoing treatment at our center were asked to fill a questionnaire detailing their out-of-pocket expenses. Results: Nonmedical expenses accounts for about 46% of their monthly household income of parents from rural areas and 22% of their household income from urban areas. On an average, a family from rural area spends four times the normal amount spent on home for their daily food expenditure. Thirty-eight percent of families have borrowed money from money lenders with an average interest rate of about 12.5% which pushes them to a state of debt for the next few years. Conclusions: Out-of-pocket expenses contribute a significant proportion to the financial burden of the families with childhood malignancies and these invisible expenses should be recognized and provide adequate support to lessen the burden of this economic impact.
Keywords
Childhood cancer treatment - developing country - out-of-pocket expensesPublication History
Article published online:
06 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Introduction
With the major shift in the magnitude of childhood mortality by the decline in the infectious cause of death, a large and growing proportion of global childhood mortality is due to noncommunicable diseases. 6.0% and 18.6% of death among children aged 5–14 years in the lower and upper middle-income countries are due to cancer.[1] Approximately 160,000 children and adolescents are diagnosed with cancer every year worldwide, and 80% of them live in low- and middle-income countries.[2]
Fortunately, the survival rate of children with cancer has increased dramatically since the late 1990s. However, life-saving cancer therapy is costly and may result in financial burden for these families, when there are already disruptions in family dynamics. Although financial constraints remain a major stressor for families of children with cancer, they are yet poorly recognized. Added to the stress of diagnosis and treatment, the economic burden can have long-term effects on the financial security, quality of life, future well-being of the entire family including the siblings of the affected child. Financial costs for treating childhood cancer care are traditionally assessed based on the amount spent for diagnostic tests, hospitalization, and chemotherapy. The financial costs for travel, accommodation, out-of-pocket expenses for food, phone bills, and loss of income due to reduction or termination of parental employment are hidden nonmedical expenses that are rarely accounted for. Out-of-pocket expenses by definition are not covered by insurance or government funding. Understanding the measures by which family absorbs the changes in expenditure and income is important for the psychosocial care of the families. In resource-limited countries, its not unnatural that these families attempt to absorb these costs by increasing their debts, obtaining loans, using credits, borrowing money from friends and relatives, selling their assets, utilizing the long-term savings, and compromising the quality of life of other family members and siblings.
Subjects and Methods
Aims and objectives
This study was done to find out the details of out-of-pocket expenses incurred by the families during their treatment of cancer children and its implications on their quality of life.
Methods
Following the Institutional Research Ethics Board Approval for the students' project proposal, a prospective study over a 1-year period (June 2012–June 2013) was undertaken. A structured questionnaire was developed from the literature review of similar studies and was validated by two more pediatric hemato-oncologists from different institutions. Eligible patients were children aged 0–18 years, diagnosed with malignancy, who were more than 3 months past diagnosis and undergoing treatment at our center. Caregivers of the eligible patients completed an informed consent and the survey. Randomly selected sample of seventy families were interviewed in privacy for about 45 mins to 1 h.
These families were undergoing treatment in a ward setting where the families from poor socioeconomic status had no hospital charges for admission, no doctor fees, and no nursing charges. The investigations were being done at subsidized cost, and some of the chemotherapy drugs were funded by the various cancer support groups. The hospital also provides free food for the patients during their hospital stay.
The background demographics section comprised items including the age, gender of the patient, disease demographics such as diagnosis and treatment status, parental income, educational qualification, residential context, number of earning members in the family, and dependent children. The type of expenses comprised items, such as hospitalization charges, chemotherapy drugs, travel, accommodation, food, and communication. The impact of the financial crisis was assessed by the items such as estimated cost spent since diagnosis, whether they had governmental financial assistance, borrowed money from banks or private money lenders, had to sell their assets and had to utilize the long-term savings or not?
Annual household income was divided into four groups: (1) > Rs. 180,000, (2) Rs. 120,000–1,79,999, (3) Rs. 60,000–119,999, and (4)
Caregiver education was categorized as graduate, high school, primary school, and illiterate.
Medical expenses comprise primarily the expenditure associated with use of healthcare in diagnosis, treatment, hospitalization, professional fee, and food for patient in hospital. Nonmedical expenses include all the out-of-pocket expenses incurred by the families in the course of care (transport, food, accommodation, communication, etc.) and loss of pay. For the convenience of the study, loss of pay, which is essentially an indirect or invisible expense, is assessed under nonmedical expenses. Demographic details of the patients and families are listed in Table 1 and the out-of-pocket expenses details in Table 2.
Table 1
Demographic details of the patients (n=70)
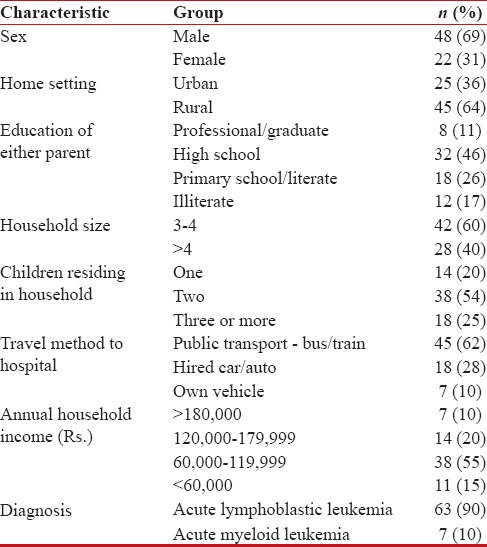
|
Table 2
Out-of-pocket expenses details
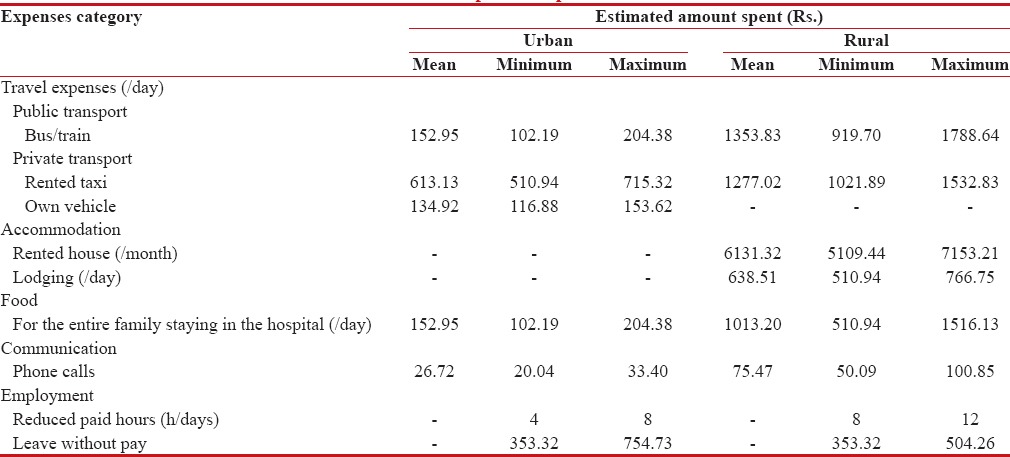
|
Results
Of the seventy patients with malignancies, with 69% boys and 31% girls, the mean age was 7.8 ± 2.2 years. All the patients were undergoing active treatment, and 63% of the patients were from rural areas. Fifty-five percent of the patients household annual income (n = 38) ranged between Rs. 60,261.02 and Rs. 120,522.71. Nonmedical expenses account for about 46% of their monthly household income of parents from rural areas and 22% of their household income from urban areas. Out-of-pocket expenses for food and travel and accommodation have emerged as a major contributing factor for severe economic effect on the family as it accounts for two-thirds of the total expenses incurred during each hospital admissions. On an average, a family from rural area spends four times the normal amount spent on home for their daily food expenditure. The minimal amount spent by a family from rural area towards accommodation charges was Rs. 5089.22/month and Rs. 508.92/day and hence among the 63% of rural families, only 20% of them opted for a change in accommodation, nearby the treatment center. However, they had to spend a minimum amount of Rs. 1781.56 when they had to travel by a public transport and Rs. 1526.77 when they came by rented taxi during each admission.
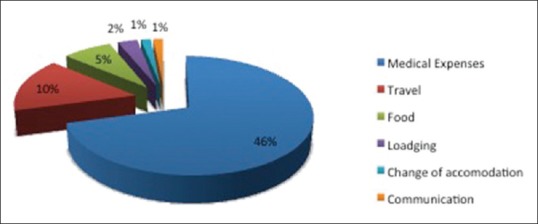
Sixty-three percent of patients used public transport such as trains or buses for travel for treatments and follow-up. Loss of pay is seen more often with working mothers than with fathers. Cancer diagnosis in children has a significant impact on the productivity and duration of work of the parents. None of the patients had private medical insurance. Fifty percent of the households with multiple children have restricted the need for other siblings to provide for the diseased child. Fifty-five percent of them had borrowed money from their friends and relatives. Twenty-two percent of families have borrowed money from money lenders with an average interest rate of about 12.5% which pushes them to a state of debt for the next few years. Thirty-eight percent of them were doing over time and other odd jobs to overcome the financial crisis. Sixty-two percent of them had used up all their savings and 68% of them had gone into debts. Twenty-five percent of them had sold their properties and assets to make the ends meet. Only one family had abandoned treatment due to the financial constraints. The major factor which contributed to higher out-of-pocket expenses was the settlement in rural area and type of malignancy. The family from rural area had to spend more on food, travel and accommodation, and the family of the child with acute myelogenous leukemia had to stay for longer duration than a child with acute lymphocytic leukemia (ALL). Fifty-five percent (78%) of them had gone to various private practitioners and hospitals and had spent an average amount of 15,000–35,000 before they reached the tertiary care center. The impact of the out-of-pocket expenses on their financial economy is shown in Figure 1.
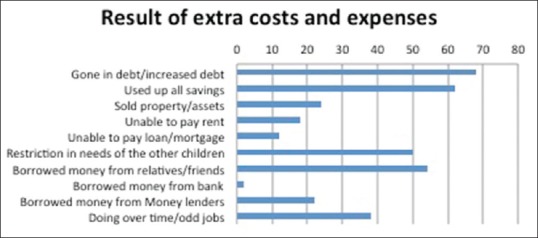
| Figure 1:Impact of the out-of-pocket expenses on the financial status of the families
Discussion
The financial burden of the illness has emerged as a major source of distress, second only to the disease itself. Of the financial concerns, the nonmedical costs pose significant problems, as they must be paid as they are incurred and are never reimbursed. Assessable financial costs generally do not include hidden nonmedical or out-of-pocket expenses for the families. The out-of-pocket expenditures (food, transport, accommodation, and communication), however, it creates drastic blow on the financial status of the family, the magnitude of these on the family's economic burden are still excluded in majority of the studies. In developing countries, there are no adequate programs to support families who care for children with catastrophic illnesses such as cancer.
Dockerty et al. have reported that 37% of the families were forced to borrow money to cover the extra cost of treatment related to their child's treatment.[3] Nonmedical expenses and lost parental wages have been accounted for a minimum 26%-decrease in family income by Lansky.[4]
Health has reported that parents of children with cancer suffered greater financial hardships than did parents with of children with any other serious illness.[5]
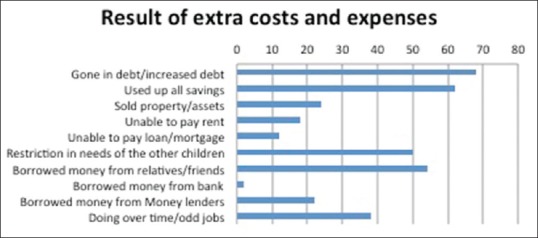
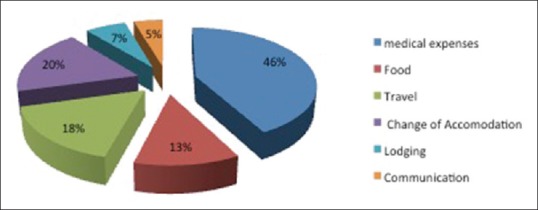
In a comparison made between medical and nonmedical expenses, in our study, mean nonmedical constitutes more than 45% of the total expenditure. A significantly higher proportion of rural families had reported higher costs for travel, accommodation, food, long distance telephone calls as depicted in Figure 2 where the nonmedical expenses constituted 54% of the total expenses per admission. The families from urban area spend around 19% of the total expenses toward out-of-pocket expenses as shown in Figure 3.
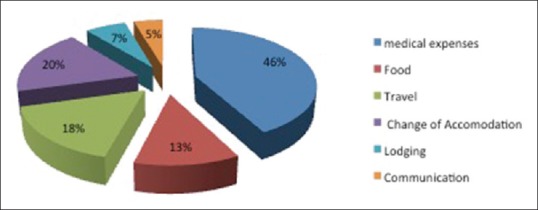
| Figure 2:Percentage of total costs utilized by a rural family
| Figure 3:Percentage of costs utilized by an urban family
During the hospital stays or outpatient visits, families had to buy food for themselves and for the child also, as most of the times, the child preferred outside food to hospital food. If the parents responsible for preparing the meals are accompanying the child every time to the hospital, the other family members might be forced to at out or buy prepared meals, thereby adding to the food costs. The results show that the family spends about 4 times the regular home-made food cost on hospital meals. The average amount spent on food per day by a family from rural area is Rs. 1009.20 and Rs. 152.34 for an family from urban area.
Majority of the tertiary care centers offering cancer treatment are located in urban areas, forcing the rural patients to travel longer distance for care, lodging outside home, thereby potentially contributing to greater financial burden. However, renting an accommodation near the treatment center would be doubling up the expenses as they have to spend for the rent, electricity charges, groceries, household items both at their permanent residence and at the rented accommodation for the treatment purposes, most of the families prefer travelling back and forth constantly from home to hospital for treatment schedule, accumulating considerable travel costs. Of the seventy families interviewed, 63% of the patients had to travel out of their province for treatment. Although the public transit system may be a cheaper alternative, most of the families are worried about the risk of infection while traveling in the crowded vehicles. During the unexpected admissions for fever, the families always prefer travel by a private vehicle as the child is mostly sick, febrile, and unfit to travel in a public mode of transport.
Tsimicalis et al. have reported that three-quarters of the costs incurred by the families were attributed to travel (56%) and food (18%).[6]
Metzger et al. had shown that abandonment of treatment in children with ALL in Honduras was associated with longer duration of travel time to the treatment facility (>5 h) and age group <4 href="https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5398105/#ref7" rid="ref7" class=" bibr popnode tag_hotlink tag_tooltip" id="__tag_603278268" role="button" aria-expanded="false" aria-haspopup="true" xss=removed>7] Cost of transport is also a major concern for parents and have been found to be contributing to abandonment according to Sitaresmi and Yadav et al.[8,9]
Howard et al. have proved that sustained approach involving training of doctors and nurses in remote areas, transfer of diagnostic and therapeutic protocols, improving supportive care at regional centers, financial aid, can result in impressive reductions in abandonment.[10]
Cancer in a child adversely affects the parent's work opportunities due to the increased care burden and altered priorities. Cancer care for the child greatly affected the work dynamics of the parents which indirectly contribute to the invisible expenses of the family. Seventy-three percent of the fathers reported to have decreased productivity and change/decrease in work hours during the child's treatment. All mothers invariably have to stop working to provide care for the sick child. Self-employed families often experienced an immediate loss of income. Families with more than one earning member in the family were able to cope up better with the financial strain. Lansky suggested that costs exceeding 15% of yearly gross income is considered an unfair catastrophic burden.[4] However, in this study, we have demonstrated that the out-of-pocket expenses plus loss of pay average are considerably more than 15% and for 65% of the families, the figures were more than 30%. Despite the cumulative nature of the costs, parents continued to incur them as it was a matter of their child's survival.
The solution suggested by Mathews et al. is that families who must travel outside their region to access health services should be given medical travel subsidies and costs spent for meals, accommodation, and gas should be reimbursed as per Lightfoot et al.[11,12]
Effective pediatric cancer treatment requires adequate financial support for families who are without adequate resources or private health insurance. Policymakers should begin covering specific malignancies depending on prevalence and available finance resources. Given the severely constrained resources, limited infrastructure, and significant competing health concerns, low-income countries face additional challenges to provide financial assistance for childhood cancer treatment.
The single most factor that contributes to abandonment of childhood cancer treatment is financial burden faced by the family. In developing countries, social and economic support from the state is either nonexistent or mostly inadequate and medical insurance are mostly absent. Hence, the burden of the cost of treatment falls mostly on the family. Monthly income of the family has been shown to be significantly related to the abandonment rates.[13]
Cost of therapy is not simply the sum of cost of investigations and treatment. The true cost of treatment is complex interplay of multiple factors including the direct costs, indirect costs – food, transport, accommodation, communication, income lost, unemployment, lack of medical insurance, and additional costs incurred to take care of the other siblings at home. And, hence, providing free chemotherapy alone would not work, unless all these factors are taken into account.
When a child is diagnosed with cancer, family member in the household, other than parents, also incur costs which are known as the spillover effect. Families have invariably gone in debt or have pawned gold or property to meet the financial needs. In some of the families, the other sibling's education was compromised to meet the demands of the diseased child. Some of them reported that financially, it has set the family back by 5 years due to the debt and its interests. Low socioeconomic families have even reported skipping of meals when they were in the hospital to cut down the expenditure.
Our study focuses on the severity of the negative financial effects on families when they care for a child with cancer. Although none of the families have withdrawn the care due to financial constraints, the families have struggled with financial hardship, imposing additional stress on them. The debts accrued over the course of treatment had long-term effects on the financial stability of the family, making them pay the debts, years after the treatment.
Our study reiterates that the lack of assistance for the primary income loss and personal expenses such as accommodation, transport, food, and communication which account to almost two-thirds % of their total expenses during each admission for cancer treatment is a major problem to be looked into.
Limitations of the study
The limitations are (i) a small sample size (n = 70) and (ii) a single hospital-based study. It is a retrospective study which makes it difficult to ascertain the accuracy and reliability of the information collected and to obtain information on potential confounding variables. Although prescription, bills, and referral slips at hand were used, there may be a recall bias for certain measures. Children with nonhematological malignancies were not included in the study and hence the results could not be generalized with all oncological conditions. There were methodical challenges and lack of interpretative standards.
Conclusions
Families of children with cancer experience a wide range of costs. Investigations of families' costs will yield a better understanding of cancer costs, and lend insight into practice and policy changes aimed at lessening the burden of this economic impact. Health-care providers, patient advocates, agencies, and insurers should take the lead and responsibility to change the nonexistent or inconsistent methods of cancer treatment support in developing country like India to support not only the medical expenses but also the out-of-pocket expenses.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Magrath I, Steliarova-Foucher E, Epelman S, Ribeiro RC, Harif M, Li CK, et al. Paediatric cancer in low-income and middle-income countries. Lancet Oncol 2013;14:e104-16.
- Rodriguez-Galindo C, Friedrich P, Alcasabas P, Antillon F, Banavali S, Castillo L, et al. Toward the cure of all children with cancer through collaborative efforts: Pediatric oncology as a global challenge. J Clin Oncol 2015;33:3065-73.
- Dockerty JD, Skegg DC, Williams SM. Economic effects of childhood cancer on families. J Paediatr Child Health 2003;39:254-8.
- Lansky SB. The high cost of cancer. Am J Pediatr Hematol Oncol 1987;9:89-91.
- Heath JA, Lintuuran RM, Rigguto G, Tokatlian N, McCarthy M. Childhood cancer: Its impact and financial costs for Australian families. Pediatr Hematol Oncol 2006;23:439-48.
- Tsimicalis A, Stevens B, Ungar WJ, McKeever P, Greenberg M, Agha M, et al. Amixed method approach to describe the out-of-pocket expenses incurred by families of children with cancer. Pediatr Blood Cancer 2013;60:438-45.
- Metzger ML, Howard SC, Fu LC, Peña A, Stefan R, Hancock ML, et al. Outcome of childhood acute lymphoblastic leukaemia in resource-poor countries. Lancet 2003;362:706-8.
- Sitaresmi MN, Mostert S, Schook RM, Sutaryo, Veerman AJ. Treatment refusal and abandonment in childhood acute lymphoblastic leukemia in Indonesia: An analysis of causes and consequences. Psychooncology 2010;19:361-7.
- Yadav S, Anjan M, Sachdeva A. Outcome of children with haematological malignancies who are lost to follow up. Pediatr Blood Cancer 2007;49:527.
- Howard SC, Pedrosa M, Lins M, Pedrosa A, Pui CH, Ribeiro RC, et al. Establishment of a pediatric oncology program and outcomes of childhood acute lymphoblastic leukemia in a resource-poor area. JAMA 2004;291:2471-5.
- Mathews M, West R, Buehler S. How important are out-of-pocket costs to rural patients' cancer care decisions? Can J Rural Med 2009;14:54-60.
- Lightfoot N, Steggles S, Gauthier-Frohlick D, Arbour-Gagnon R, Conlon M, Innes C, et al. Psychological, physical, social and economic impact of travelling great distances for cancer treatment. Curr Oncol 2005;12:1-7.
- Bonilla M, Rossell N, Salaverria C, Gupta S, Barr R, Sala A, et al. Prevalence and predictors of abandonment of therapy among children with cancer in El Salvador. Int J Cancer 2009;125:2144-6.
| Figure 1:Impact of the out-of-pocket expenses on the financial status of the families
| Figure 2:Percentage of total costs utilized by a rural family
| Figure 3:Percentage of costs utilized by an urban family
References
- Magrath I, Steliarova-Foucher E, Epelman S, Ribeiro RC, Harif M, Li CK, et al. Paediatric cancer in low-income and middle-income countries. Lancet Oncol 2013;14:e104-16.
- Rodriguez-Galindo C, Friedrich P, Alcasabas P, Antillon F, Banavali S, Castillo L, et al. Toward the cure of all children with cancer through collaborative efforts: Pediatric oncology as a global challenge. J Clin Oncol 2015;33:3065-73.
- Dockerty JD, Skegg DC, Williams SM. Economic effects of childhood cancer on families. J Paediatr Child Health 2003;39:254-8.
- Lansky SB. The high cost of cancer. Am J Pediatr Hematol Oncol 1987;9:89-91.
- Heath JA, Lintuuran RM, Rigguto G, Tokatlian N, McCarthy M. Childhood cancer: Its impact and financial costs for Australian families. Pediatr Hematol Oncol 2006;23:439-48.
- Tsimicalis A, Stevens B, Ungar WJ, McKeever P, Greenberg M, Agha M, et al. Amixed method approach to describe the out-of-pocket expenses incurred by families of children with cancer. Pediatr Blood Cancer 2013;60:438-45.
- Metzger ML, Howard SC, Fu LC, Peña A, Stefan R, Hancock ML, et al. Outcome of childhood acute lymphoblastic leukaemia in resource-poor countries. Lancet 2003;362:706-8.
- Sitaresmi MN, Mostert S, Schook RM, Sutaryo, Veerman AJ. Treatment refusal and abandonment in childhood acute lymphoblastic leukemia in Indonesia: An analysis of causes and consequences. Psychooncology 2010;19:361-7.
- Yadav S, Anjan M, Sachdeva A. Outcome of children with haematological malignancies who are lost to follow up. Pediatr Blood Cancer 2007;49:527.
- Howard SC, Pedrosa M, Lins M, Pedrosa A, Pui CH, Ribeiro RC, et al. Establishment of a pediatric oncology program and outcomes of childhood acute lymphoblastic leukemia in a resource-poor area. JAMA 2004;291:2471-5.
- Mathews M, West R, Buehler S. How important are out-of-pocket costs to rural patients' cancer care decisions? Can J Rural Med 2009;14:54-60.
- Lightfoot N, Steggles S, Gauthier-Frohlick D, Arbour-Gagnon R, Conlon M, Innes C, et al. Psychological, physical, social and economic impact of travelling great distances for cancer treatment. Curr Oncol 2005;12:1-7.
- Bonilla M, Rossell N, Salaverria C, Gupta S, Barr R, Sala A, et al. Prevalence and predictors of abandonment of therapy among children with cancer in El Salvador. Int J Cancer 2009;125:2144-6.


 PDF
PDF  Views
Views  Share
Share

