Epithelioid Trophoblastic Tumor—A Challenge to Manage due to Its Rare Existence: A Case Report with Review of Literature
CC BY 4.0 · Indian J Med Paediatr Oncol 2024; 45(06): 550-553
DOI: DOI: 10.1055/s-0044-1788777
Epithelioid trophoblastic tumor (ETT) is the rarest type of gestational trophoblastic neoplasia. It has variable presentations and is an aggressive tumor. Because of its rarity, it is difficult to establish an appropriate diagnosis, management, and follow-up. A woman of age 45 years postmenopausal status with an antecedent term pregnancy 13 years back was diagnosed to have ETT in the hysterectomy specimen. She had come with urinary retention as the tumor was infiltrating the bladder. Beta-human chorionic gonadotropin levels were normal. Immunohistochemistry confirmed the diagnosis. Though metastatic workup was normal, adjuvant multiagent chemotherapy was given as the bladder flap margin was not free of tumor cells and antecedent pregnancy was > 4 years. Every new case of ETT needs to be reported to bring about more awareness of the unusual presentations, and it may help come to a consensus for appropriate management.
Keywords
epithelioid trophoblastic tumor - gestational trophoblastic neoplasia - placental site trophoblastic tumorAuthors' Contribution
All authors have agreed to the manuscript description. R.C. contributed to data collection and manuscript preparation. V.S. contributed to concept design and clinical treatment. N.N. contributed to manuscript preparation and editing.
Declaration of the Patient Consent Form
Patient's consent has been obtained for publishing her case report and images.
Publication History
Article published online:
05 August 2024
© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Epithelioid trophoblastic tumor on posterior wall of uterus: a case ReportMSR Freifrau von Welser, Geburtshilfe und Frauenheilkunde, 2016
- Diffuse Leptomeningeal Glioneuronal Tumor: A Rare Case Report with Review of LiteratureAmey P. Patankar, VCOT Open
- Malignant Perivascular Epithelioid Cell Tumor Mimicking Jugular Foramen Schwannoma: A Case Report and Literature ReviewNoritaka Komune, Journal of Neurological Surgery Part B: Skull Base, 2019
- Tumor-Induced Osteomalacia: A Case Report of Rare Disease and Literature reviewShivam Bansal, South Asian Journal of Cancer
- Cervical Hibernoma: A Very Rare Tumor of Childhood – Case Report with Review of LiteratureAdvait Prakash, Indian Journal of Medical and Paediatric Oncology, 2020
- Cervical epithelioid trophoblastic tumor: report of one case and literature review ZHANG Ming-zhu TANG Li-wei SUN Fang GAO Yan-bing, CMA Publishing House, 2022
- A case of accurate diagnosis of rare placental trophoblastic tumor by transvaginal ultrasound CMA Publishing House, 2023
- Perivascular epithelioid cell tumor of uterus: a case report CMA Publishing House, 2023
- A case report of bronchial glomus tumor and literature review Jin Cong Cao Lihua, CMA Publishing House, 2022
- Urachal yolk sac tumor in children: one case report with a literature review Zhang Hong Bai Jianxi Zhang Bing Wu Dianming Fang Yifan, CMA Publishing House, 2024
Epithelioid trophoblastic tumor (ETT) is the rarest type of gestational trophoblastic neoplasia. It has variable presentations and is an aggressive tumor. Because of its rarity, it is difficult to establish an appropriate diagnosis, management, and follow-up. A woman of age 45 years postmenopausal status with an antecedent term pregnancy 13 years back was diagnosed to have ETT in the hysterectomy specimen. She had come with urinary retention as the tumor was infiltrating the bladder. Beta-human chorionic gonadotropin levels were normal. Immunohistochemistry confirmed the diagnosis. Though metastatic workup was normal, adjuvant multiagent chemotherapy was given as the bladder flap margin was not free of tumor cells and antecedent pregnancy was > 4 years. Every new case of ETT needs to be reported to bring about more awareness of the unusual presentations, and it may help come to a consensus for appropriate management.
Keywords
epithelioid trophoblastic tumor - gestational trophoblastic neoplasia - placental site trophoblastic tumorIntroduction
Epithelioid trophoblastic tumor (ETT) is the rarest of gestational trophoblastic neoplasia (GTN) with an incidence of 2.2%-of all GTNs.[1] It develops from neoplastic transformation of intermediate trophoblastic cells (ITC). Intermediate trophoblastic tumors exhibit exaggerated placental site, placental site nodule (PSN), placental site trophoblastic tumor (PSTT), and ETT. Implantation type gives rise to PSTT and chorionic type results in ETT. That is the reason both behave similarly and are distinguished mainly by immunohistochemistry (IHC).
Case Report
A woman aged 45 years who had attained menopause 3 years back had presented to an outside hospital with retention of urine. She is para 2 living 2 with her last child birth 13 years back which was a full-term delivery. Prior cycles were regular, and now she did not have postmenopausal bleeding. On evaluation by ultrasound (US) and magnetic resonance imaging ([Fig. 1]), it showed a solid cystic pelvic mass with calcification of 8 × 10 × 7 cm predominantly on the left side involving the uterus with nonvisualized left ovary with an impression of neoplastic etiology of either ovarian or uterine origin. No ascites or pelvic lymphadenopathy was noted. The tumor marker CA-125 level was 14.6 U/mL. She underwent exploratory laparotomy in that hospital where a uterine tumor was noted infiltrating the bladder anteriorly. Total abdominal hysterectomy with bilateral salpingo-oophorectomy with excision of bladder flap was done. The gross specimen of the uterus showed a tumor size of 8 × 7.5 × 5 cm occupying the lower uterine segment breaching the serosa in the left lateral aspect of the uterus infiltrating the bladder. Microscopy showed epithelioid tumor cell nests with necrosis and calcification with atypical features and a 4 mitosis/10 hpf (high power field) was noted ([Fig. 2]). Tumor cells were seen involving the adjacent fallopian tube and ovary. The International Federation of Gynecology and Obstetrics (FIGO) stage II was reported as the tumor extends to other genital organs. IHC was asked for confirmation. The patient came to us with an IHC report for further management. IHC markers of cytokeratin (CK) 8/18, P63, and inhibin were positive. SALL4, desmin, and GATA3 were negative. Ki-67 was 20%-([Fig. 3]). After seeing the histopathological report, β human chorionic gonadotropin (β-hCG) was done and was 4.47 mIU/mL.
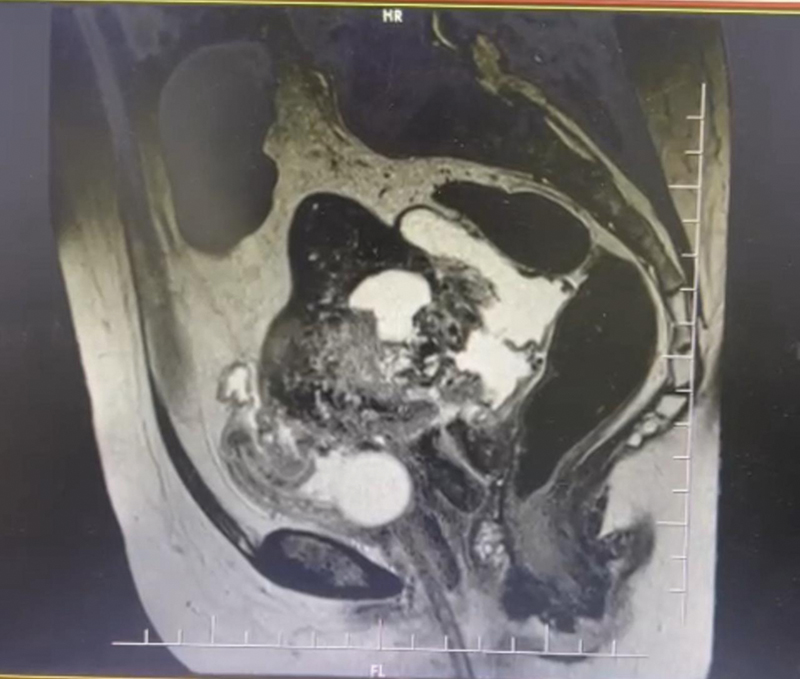
| Fig 1Magnetic resonance imaging showing pelvic mass infiltrating the bladder.
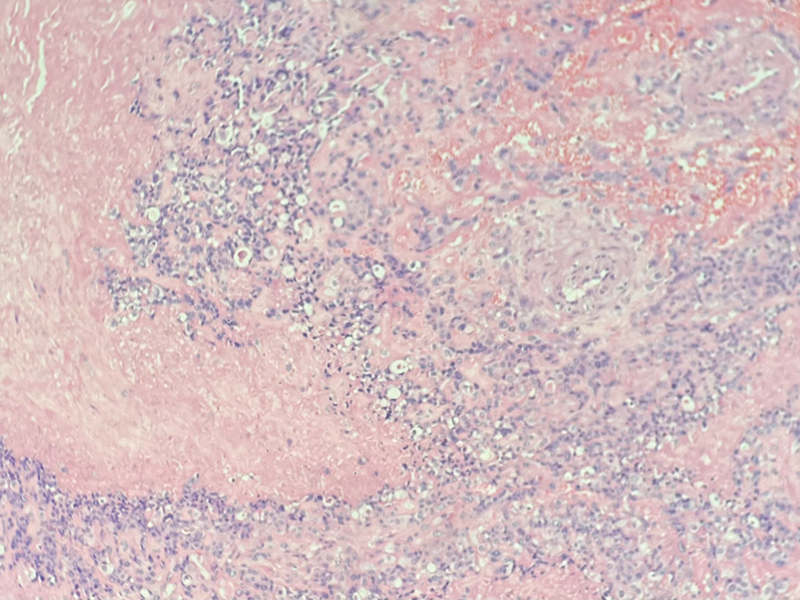
| Fig 2Microscopy (hematoxylin and eosin stain) showing nests of epithelioid cells with atypical features, with hyalinization and necrosis.
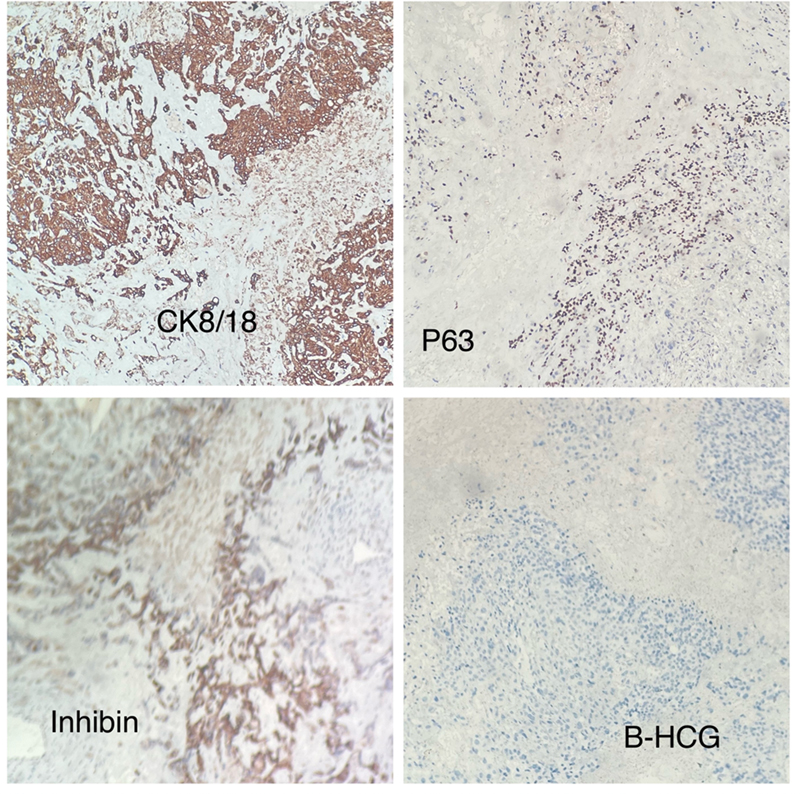
| Fig 3 Immunohistochemistry of tumor cells showing positive expression for cytokeratin (CK8/18), P63, inhibin and negative for β-human chorionic gonadotropin (β-hCG).
A metastatic workup of chest X-ray, β-hCG, and computed tomography (CT) of the lung, abdomen, and pelvis was done and found to be normal. Her FIGO score was 9 (high risk: >40 years old [45 years = 1], index pregnancy [term delivery = 2], time since delivery [13 years = 4], β-hCG (4.47 mIU/mL = 0), size of the tumor (>5 cm = 2), metastasis (none = 0), number of metastasis (none = 0), and previous failed chemotherapy drugs (no = 0). After discussing with the medical oncologist, we came to a decision even though there was no metastasis, we planned to give adjuvant chemotherapy as her antecedent pregnancy was >4 years, and the excised bladder flap margin was not free of tumor cells. Three cycles of etoposide, methotrexate, actinomycin-D, cyclophosphamide, and oncovin (EMA/CO) were planned. The patient received three cycles of the multiagent chemotherapy and has been called for follow-up after 4 weeks. We planned to follow her up regularly with an examination, β-hCG levels, US/contrast-enhanced CT of the abdomen and pelvis for a minimum period of 5 years. The tumor board had decided to only give adjuvant chemotherapy and to follow-up regularly to look for recurrence. Since ETT is radioresistant tumor, radiotherapy was not considered.
Discussion
GTN is a malignant transformation of a gestational event which consists of invasive mole, choriocarcinoma, PSTT, and ETT. Initially, ETT was termed as atypical choriocarcinoma, later Shih and Kurman in 1998 called it as ETT. It is commonly seen in reproductive age group of 15 to 48 years (mean 36 years).[2] Very few cases are reported in postmenopausal age group. Though our patient is 45 years old, she had attained menopause 3 years ago. Most of the patients (67%) present with irregular vaginal bleeding. Other symptoms include abdominal pain, abdominal distension, amenorrhea, or symptoms due to metastasis. Many at times it is incidentally found in a hysterectomy specimen[3] or dilatation and curettage sample. Here, patient had presented with urinary retention probably because the tumor was infiltrating the bladder. Uterus is the primary site (40%) especially the lower uterine segment just like in this case. The next site which is commonly involved is cervix (31%) and can be confused to squamous cell carcinoma (SCC) of the cervix. The commonest extrauterine site is lung (19%) and other sites where tumor can arise include broad ligament, fallopian tube, ovary, pelvis, and vagina. There are few cases of only isolated lung lesions without any uterine involvement. The tumor size usually ranges from 0.5 to 4 cm. The tumor is usually expansive in the endometrial cavity and locally infiltrates the myometrium or can expand toward the cervical canal. The antecedent pregnancy is either a term delivery (43%), molar (39%), abortion in 18%-which may occur 1 to 18 years (mean of 6.2 years) prior to the disease per se.[2] In this case, she had a term delivery nearly 13 years ago which makes us think whether that pregnancy triggered the malignant transformation or is there any other reason or source for development of this tumor. However, antecedent pregnancy > 4 years is a poor prognostic factor triggering us to treat her with multiagent chemotherapy following surgery.
Elevated β-hCG is seen in 69%-of cases and the levels are mostly < 2,500 mIU/mL unlike in choriocarcinoma where it is very high (>10,000 mIU/mL).[3] There have been few cases reported where the β-hCG levels were normal,[4] and it becomes difficult to use it for follow-up unlike in choriocarcinoma. The diagnosis of ETT is based on microscopy and IHC. Microscopically, tumor cells appear uniformly mononucleated chorionic type intermediate trophoblasts with round nuclei and eosinophilic cytoplasm and grow in nests. A distinct hyaline-like material and necrosis can also be noted with no significant vascular invasion. ETT has a diffuse expression for markers such as CK/CK 18, epithelial membrane antigen, and P63. It has focal or patchy expression for hCG, human placental lactogen (hPL), and melanoma cell adhesion molecule (MEL-CAM) (CD146). It is positive for inhibin in 20 to 80%.[5] In this case, it was positive for P63, CK/CK 18, and inhibin. The mitotic index varies from 0 to 9 mitosis/hpf. In this case, it was 4 mitosis/hpf. High mitotic index suggests an aggressive tumor. The mean Ki-67 index in ETT is 17.7 + 4.5.[5]
The differential diagnosis for ETT includes choriocarcinoma, PSTT, PSN, SCC of the cervix, and epithelioid malignant smooth muscle tumor (ESMT). It is easy to differentiate choriocarcinoma as it has both cytotrophoblast and syncytiotrophoblast. PSTT is very infiltrative growth, with prominent vascular invasion, and has larger implantation type ITCs. IHC differentiates PSTT from ETT as PSTT is diffusely positive to hPL, MEL-CAM (CD146) and negative to P63. ETT can be misdiagnosed as SCC of the cervix especially when ETT is located at the cervix and ETT's hyaline-like matrix and necrotic debris can resemble keratin present in the SCC of the cervix. IHC helps in distinguishing as inhibin and CK 18 are positive in ETT but not in the SCC of the cervix. Ki-67 proliferative index is usually 10 to 25%-in ETT, whereas it is high (>50%) in choriocarcinoma and in SCC of the cervix. In our case, it was 20%. In ESMT, smooth muscle markers will be positive. There are cases where ETT was misdiagnosed as stage IIIB cancer of the cervix and treated with radiotherapy[6] with no good response to the treatment and also as choriocarcinoma which was treated with only chemotherapy (without surgery) without any positive response.[7] Hence, one should be very vigilant while diagnosing ETT.
Surgery is the preferred treatment as ETT is more chemoresistant than choriocarcinoma. The standard treatment includes total hysterectomy for early-stage disease and resection of metastatic lesions if feasible followed by multiagent chemotherapy in metastatic disease only. Patients with isolated lung lesion had better outcome with excision, although they were classified as stage III. For stage I disease with antecedent pregnancy > 48 months or persistent high β-hCG levels and any stage with metastatic disease postadjuvant platinum-based chemotherapy, either EMA/CO or etoposide, methotrexate, actinomycin-D, etoposide, cisplatin (EMA/EP) is recommended.[8] In this case, she had certain risk factors such as her prior gestational event was 13 years back, age >40 years, and since bladder invasion was noted and margins were not free, we decided to go for multiagent chemotherapy to prevent a recurrence. In a case reported earlier in 2015, a 47-year-old woman with menopausal status and an antecedent pregnancy 16 years back was treated with only surgery and she had a recurrence 4 years later though her β-hCG levels were low following surgery.[5]
Liu et al[1] did a retrospective study on 31 patients and noted stages II to IV, >3 metastatic lesions, and chemotherapy treatment without surgery were associated with adverse recurrence-free survival. FIGO anatomical stage is a significant prognostic factor for ETT. Combined surgery with multiagent chemotherapy is required in metastatic disease or localized disease with persistently positive β-hCG after surgery or if surgery is unfeasible. The preferred chemotherapy is EMA/EP or EMA/CO.
Yang et al revealed univariate analysis showed only stage IV as the only risk factor for poor overall survival rate. In multivariate analysis, an antecedent pregnancy of >120 months, stage IV disease, metastatic disease, and beta-hCG >1,000 IU/L were significantly associated with poor disease-free interval, and it was suggested to keep a close watch for recurrence. In this study, certain immune checkpoints were also looked for such as programmed death (PD)-L1, B7-H3, and CD105, and these were detected 100%-in ETT cases, where PD-L2 and V-domain immunoglobulin suppressor of T-cell activation were detected in 82%, B7-H6 was seen in 18%, and B7-H4 was not detected at all. New therapeutic targets are required to treat nonoperable patients with metastatic chemoresistant diseases. Pembrolizumab (a humanized monoclonal antibody against PD-1) was effective in chemoresistant GTN. The use of immunotherapy and antiangiogenic treatment are upcoming options even in patients with ETT.[9]
Metastatic disease is seen in 25 to 42%-of cases. Metastasis can occur in lung (commonest), liver, brain, small bowel, vagina, and pelvic lymph nodes. Mortality is seen in > 10%. The main cause of early death (which can occur < 4 weeks from diagnosis) may be mainly due to hemorrhage from metastatic lesions or because of tumor destruction following administration of full-dose chemotherapy.[8]
Every ETT case needs to be reported to understand this unusual disease so that we can establish a proper means of diagnosis and management.
Conclusion
ETT is a rare and aggressive tumor that can have diverse presentations. Because of limited knowledge of ETT, diagnosis and management remain challenging and can lead to mismanagement and delay in appropriate treatment. Diagnosis is made on morphological grounds, so the pathologists play an important role to detect the disease. This case highlights that ETT can occur in postmenopausal, with no recent gestational event and with low β-hCG levels.
Conflict of Interest
None declared.
Acknowledgment
The authors are thankful to the patient for her willingness to publish her case report.
Authors' Contribution
All authors have agreed to the manuscript description. R.C. contributed to data collection and manuscript preparation. V.S. contributed to concept design and clinical treatment. N.N. contributed to manuscript preparation and editing.
Declaration of the Patient Consent Form
Patient's consent has been obtained for publishing her case report and images.
References
- Liu W, Zhou J, Yang J, Huang X. A multicenter retrospective study of Epithelioid trophoblastic tumor to identify the outcomes, prognostic factors and therapeutic strategies. Front Oncol 2022; 12: 907045
- Sung WJ, Shin HC, Kim MK, Kim MJ. Epithelioid trophoblastic tumor: clinicopathologic and immunohistochemical analysis of three cases. Korean J Pathol 2013; 47 (01) 67-73
- Scott EM, Smith AL, Desouki MM, Olawaiye AB. Epithelioid trophoblastic tumor: a case report and review of the literature. Case Rep Obstet Gynecol 2012; 2012: 862472
- Aniţei M-G, Lazăr D-E, Pleşca RA, Terinte C, Iulian R, Viorel S. Uterine epithelioid trophoblastic tumor in a 44-year-old woman: a diagnostic dilemma. Clin Pract 2021; 11 (03) 631-639
- Keser SH, Kokten SC, Cakir C, Sensu S, Buyukbayrak EE, Karadayi N. Epithelioid trophoblastic tumor. Taiwan J Obstet Gynecol 2015; 54 (05) 621-624
- Jordan S, Randall LM, Karamurzin Y. et al. Differentiating squamous cell carcinoma of the cervix and epithelioid trophoblastic tumor. Int J Gynecol Cancer 2011; 21 (05) 918-922
- Shet T, Parage M, Maheshwari A. et al. Epithelioid trophoblastic tumor of uterus presenting as an ovarian mass: a diagnostic and therapeutic dilemma. Indian J Pathol Microbiol 2008; 51 (02) 242-244
- Nakamura B, Cowan M, Griffin BB, Victoria Fischer J, Lurain JR, Strohl AE. Successful management of stage IV epithelioid trophoblastic tumor using multimodality treatment: a case report. Gynecol Oncol Rep 2021; 37: 100802
- Yang J, Zong L, Wang J, Wan X, Feng F, Xiang Y. Epithelioid trophoblastic tumors: treatments, outcomes and potential therapeutic targets. J Cancer 2019; 10 (01) 11-19
Address for correspondence
Neetha Nandan, MS, FRCOGDepartment of Obstetrics and Gynaecology, K.S. Hegde Medical Academy, NITTE (Deemed to be University)Mangaluru 575018, Dakshina Kannada, KarnatakaIndiaEmail: nvyas@nitte.edu.inPublication History
Article published online:
05 August 2024© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, IndiaWe recommend- Epithelioid trophoblastic tumor on posterior wall of uterus: a case ReportMSR Freifrau von Welser, Geburtshilfe und Frauenheilkunde, 2016
- Diffuse Leptomeningeal Glioneuronal Tumor: A Rare Case Report with Review of LiteratureAmey P. Patankar, VCOT Open
- Malignant Perivascular Epithelioid Cell Tumor Mimicking Jugular Foramen Schwannoma: A Case Report and Literature ReviewNoritaka Komune, Journal of Neurological Surgery Part B: Skull Base, 2019
- Tumor-Induced Osteomalacia: A Case Report of Rare Disease and Literature reviewShivam Bansal, South Asian Journal of Cancer
- Cervical Hibernoma: A Very Rare Tumor of Childhood – Case Report with Review of LiteratureAdvait Prakash, Indian Journal of Medical and Paediatric Oncology, 2020
- Pulmonary infection due to Mycobacterium szulgai, case report and review of the literature. E Tortoli, European Respiratory Journal, 1998
- Acute spontaneous spinal subdural hematoma presenting with Takotsubo cardiomyopathy: a rare case report and literature review Jie Xiang, EFORT Open Rev, 2022
- Eosinophilic granulomatosis with polyangiitis: case report and literature review Vardah Alam, Breathe, 2022
- Endobronchial aspergilloma: A case report and literature review Bing Li, European Respiratory Journal, 2016
- Intravesical explosion during transurethral resection of bladder tumor: a case report and review of the literature PAN Zheng-sheng, Fudan University Journal of Medical Sciences, 2022
- Epithelioid trophoblastic tumor on posterior wall of uterus: a case Report
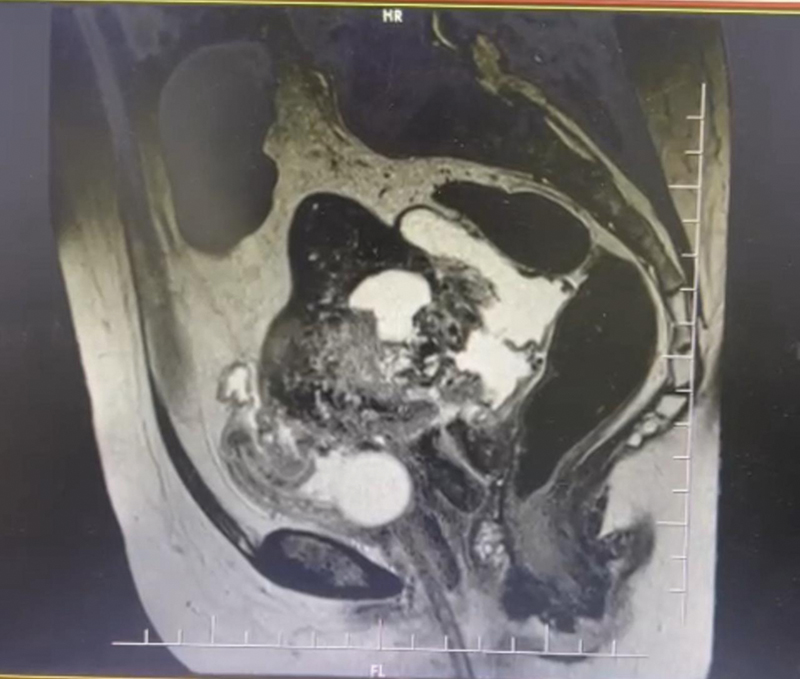
| Fig 1Magnetic resonance imaging showing pelvic mass infiltrating the bladder.
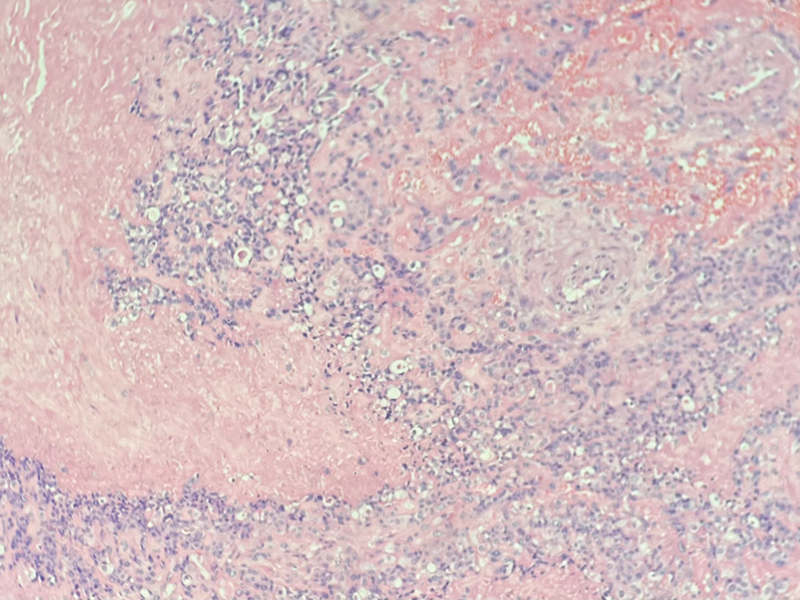
| Fig 2Microscopy (hematoxylin and eosin stain) showing nests of epithelioid cells with atypical features, with hyalinization and necrosis.
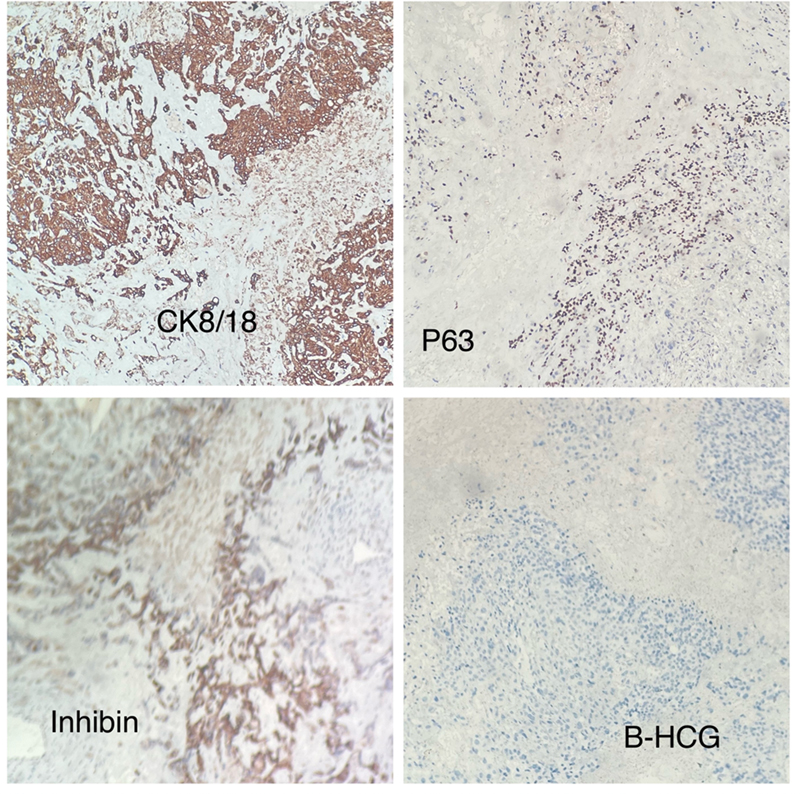
| Fig 3 Immunohistochemistry of tumor cells showing positive expression for cytokeratin (CK8/18), P63, inhibin and negative for β-human chorionic gonadotropin (β-hCG).
References
- Liu W, Zhou J, Yang J, Huang X. A multicenter retrospective study of Epithelioid trophoblastic tumor to identify the outcomes, prognostic factors and therapeutic strategies. Front Oncol 2022; 12: 907045
- Sung WJ, Shin HC, Kim MK, Kim MJ. Epithelioid trophoblastic tumor: clinicopathologic and immunohistochemical analysis of three cases. Korean J Pathol 2013; 47 (01) 67-73
- Scott EM, Smith AL, Desouki MM, Olawaiye AB. Epithelioid trophoblastic tumor: a case report and review of the literature. Case Rep Obstet Gynecol 2012; 2012: 862472
- Aniţei M-G, Lazăr D-E, Pleşca RA, Terinte C, Iulian R, Viorel S. Uterine epithelioid trophoblastic tumor in a 44-year-old woman: a diagnostic dilemma. Clin Pract 2021; 11 (03) 631-639
- Keser SH, Kokten SC, Cakir C, Sensu S, Buyukbayrak EE, Karadayi N. Epithelioid trophoblastic tumor. Taiwan J Obstet Gynecol 2015; 54 (05) 621-624
- Jordan S, Randall LM, Karamurzin Y. et al. Differentiating squamous cell carcinoma of the cervix and epithelioid trophoblastic tumor. Int J Gynecol Cancer 2011; 21 (05) 918-922
- Shet T, Parage M, Maheshwari A. et al. Epithelioid trophoblastic tumor of uterus presenting as an ovarian mass: a diagnostic and therapeutic dilemma. Indian J Pathol Microbiol 2008; 51 (02) 242-244
- Nakamura B, Cowan M, Griffin BB, Victoria Fischer J, Lurain JR, Strohl AE. Successful management of stage IV epithelioid trophoblastic tumor using multimodality treatment: a case report. Gynecol Oncol Rep 2021; 37: 100802
- Yang J, Zong L, Wang J, Wan X, Feng F, Xiang Y. Epithelioid trophoblastic tumors: treatments, outcomes and potential therapeutic targets. J Cancer 2019; 10 (01) 11-19


 PDF
PDF  Views
Views  Share
Share

