Endobronchial Lesion and Pericardial Extension of Pediatric Hodgkin Lymphoma: A Rare Concomitant Presentation
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(03): 421-422
DOI: DOI: 10.4103/ijmpo.ijmpo_258_18
Abstract
Concomitant endobronchial lesion and pericardial effusion/extension in Hodgkin lymphoma (HL) are extremely rare and can be clinically confused with disseminated tuberculosis or aggressive non-HL changing both management and prognosis. We present a 15-year-old adolescent with complaints of fever, weight loss, and acute onset of cough, chest pain, and breathing difficulty. Computed tomography of the thorax showed moderate-to-significant pericardial effusion/extension with significant mediastinal adenopathy. A bronchoscopy demonstrated a well-defined polypoidal mass lesion in the right upper lobe bronchus. Endobronchial biopsy of the lesion with endobronchial ultrasound/transbronchial needle aspiration of mediastinal lymphadenopathy categorically diagnosed with classic HL.
Keywords
Endobronchial biopsy - endobronchial lesion - endobronchial ultrasound/transbronchial needle aspiration - Hodgkin lymphoma - mediastinal lymphadenopathyPublication History
Received: 04 December 2018
Accepted: 28 February 2019
Article published online:
28 June 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Concomitant endobronchial lesion and pericardial effusion/extension in Hodgkin lymphoma (HL) are extremely rare and can be clinically confused with disseminated tuberculosis or aggressive non-HL changing both management and prognosis. We present a 15-year-old adolescent with complaints of fever, weight loss, and acute onset of cough, chest pain, and breathing difficulty. Computed tomography of the thorax showed moderate-to-significant pericardial effusion/extension with significant mediastinal adenopathy. A bronchoscopy demonstrated a well-defined polypoidal mass lesion in the right upper lobe bronchus. Endobronchial biopsy of the lesion with endobronchial ultrasound/transbronchial needle aspiration of mediastinal lymphadenopathy categorically diagnosed with classic HL.
Keywords
Endobronchial biopsy - endobronchial lesion - endobronchial ultrasound/transbronchial needle aspiration - Hodgkin lymphoma - mediastinal lymphadenopathyIntroduction
Mediastinal and hilar lymphadenopathy is one of the most common presentation of patients with newly diagnosed intrathoracic Hodgkin lymphoma (HL), accounting for approximately 40%-of cases.[1],[2] Parenchymal and tracheobronchial presentation of HL are rare[1],[2] and seldom associated with symptomatic pericardial effusion.[3],[4] We report a 15-year-old adolescent presenting with symptomatic pericardial effusion also having endobronchial polypoidal lesion diagnosed with classical HL.
Case Report
A 15-year-old adolescent with no significant history presented with complaints of fever, weight loss for 3 weeks, acute onset of cough, chest pain, and breathing difficulty for 2 days. On admission, he was tachypneic (respiratory rate −30/min) and tachycardic (130/min) with normal blood pressure and saturations. General physical examination showed mild pallor with no significant peripheral lymphadenopathy. Systemic examination showed muffled heart sounds with other systems normal.
He was admitted to the pediatric intensive care unit for monitoring and possible further intervention. His initial investigations were normal (complete blood count, renal function test, liver function test, Widal test, malarial parasite by peripheral smear, leptospirosis IgM, blood culture/sensitivity, Mantoux test negative). Two-dimensional echocardiography showed a significant pericardial effusion and contrast-enhanced computed tomography of the thorax showed the right upper lobe (RUL) cut of the sign [Figure 1]a, significant mediastinal adenopathy [Figure 1]a and [Figure 1]b with moderate pericardial effusion/pericardial extension [Figure 1]b. Due to worsening distress and tachycardia, pericardiocentesis done, ~500 mL of straw-colored fluid drained. A differential of tuberculosis versus aggressive non-HL disease versus HL was considered.{Figure 1}
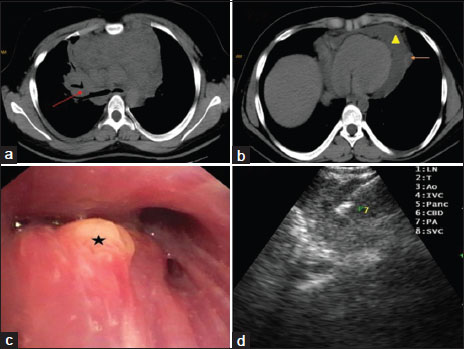
| Figure 1:(a) Computed tomography of the chest shows significant mediastinal adenopathy with bronchial cut off sign (red arrow), (b) Computed tomography of the chest shows significant mediastinal adenopathy (yellow triangle)/pericardial extension (orange arrow), (c) polypoidal growth seen entrance of the right upper lobe bronchus (black star), (d) transbronchial needle in the target lymphnode (Station 7)
Pleural fluid analysis showed lymphocytic transudate, adenosine deaminase –30 IU/L, geneexpert negative, and negative for malignant cells.
Postpericardiocentesis, distress, and tachycardia settled but continued to have persistent fever spikes. As a need for diagnosis was of paramount importance, a bronchoscopy with endobronchial ultrasound/transbronchial needle biopsy (EBUS/TBNA) of lymph nodes was planned. Bronchoscopy showed RUL mass lesion obstructing anterior segment of RUL bronchus [Figure 1]c. EBUS/TBNA [Figure 1]d and endobronchial biopsy of the mass lesion showed classical HL histopathologically confirmed on immunohistochemistry. Positron-emission tomography/computed tomography for staging showed Stage IV according to the Lugano classification [Figure 2].[5] He has currently completed two cycles of chemotherapy with no significant adverse effects.{Figure 2}
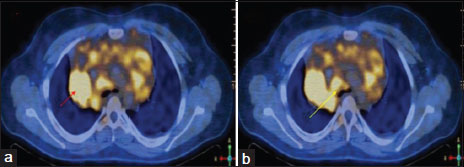
| Figure.2:(a) Positron‑emission tomography–computed tomography of the chest shows significant mediastinal adenopathy with increased radiotracer uptake with a standardized uptake value‑max of 8 (red arrow), (b) positron‑emission tomography‑computed tomography of the chest shows bronchial cut off sign with increased radiotracer uptake with a standardized
Discussion
Mediastinal lymphadenopathy (MLN) is one of the most common manifestations of intrathoracic HL, accounting to approximately 40%-of all cases.[1],[2] Isolated endobronchial,[1],[2],[6],[7] as well as pericardial extension of HL,[3],[4],[8] has been reported in different patients, respectively, but the simultaneous presentation of both in the same patient, has seldom been. The patient presented with both symptomatic pericardial effusion and endobronchial mass lesion with significant MLN. Pericardial involvement, specifically effusion, occurs in approximately 5%-of patients with HL, spread via lymphatic or hematogenous route and is a result of blockage of lymphatic and venous drainage of pericardial fluid,[8] whereas endobronchial involvement in HL is unclear. Trédaniel et al.[6] and Gallagher etal.[7] reported 3 and 9 patients in there series, respectively, presenting as endobronchial HL, confirmed by bronchial biopsy.
The patient underwent both endobronchial biopsy of the polypoidal growth and EBUS/TBNA of paratracheal (4R), right hilar (10R and 11R) lymph nodes with core biopsy for both histopathological and immunophonotypical diagnosis.
Endobronchial biopsy and EBUS/TBNA showed plenty of binucleated cells seen suggestive of Reed–Sternberg cells among the lymphocytes and histiocytes. Immunohistochemistry of the same was positive for both CD15 and CD30, thus making a categorical diagnosis of classical HL. He has currently completed two cycles of chemotherapy with no significant adverse effects.
Conclusion
Concomitant endobronchial lesion and pericardial effusion, even though rare can be the initial presentation of HL and has to be considered a possible differential to tuberculosis and non-HL.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
References
- Harper PG, Fisher C, McLennan K, Souhami RL. Presentation of Hodgkin's disease as an endobronchial lesion. Cancer 1984; 53: 147-50
- Kern WH, Crepeau AG, Jones JC. Primary Hodgkin's disease of the lung. Report of 4 cases and review of the literature. Cancer 1961; 14: 1151-65
- Pilcher J, Zubair M. Hodgkin's disease and pericardial effusion. Thorax 1970; 25: 631-3
- Retter A, Ardeshna KM, O'Driscoll A. Cardiac tamponade in Hodgkin lymphoma. Br J Haematol 2007; 138: 2
- Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E. et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano classification. J Clin Oncol 2014; 32: 3059-68
- Trédaniel J, Peillon I, Fermé C, Brice P, Gisselbrecht C, Hirsch A. et al. Endobronchial presentation of Hodgkin's disease: A report of nine cases and review of the literature. Eur Respir J 1994; 7: 1852-5
- Gallagher CJ, Knowles GK, Habeshaw JA, Green M, Malpas JS, Lister TA. et al. Early involvement of the bronchi in patients with malignant lymphoma. Br J Cancer 1983; 48: 777-81
- Bashir H, Hudson MM, Kaste SC, Howard SC, Krasin M, Metzger ML. et al. Pericardial involvement at diagnosis in pediatric Hodgkin lymphoma patients. Pediatr Blood Cancer 2007; 49: 666-71
Address for correspondence
Publication History
Received: 04 December 2018
Accepted: 28 February 2019
Article published
online:
28 June 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301
UP, India
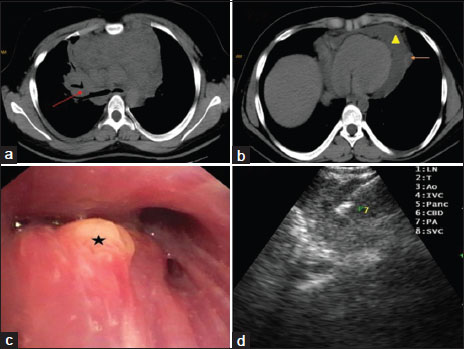
| Figure 1:(a) Computed tomography of the chest shows significant mediastinal adenopathy with bronchial cut off sign (red arrow), (b) Computed tomography of the chest shows significant mediastinal adenopathy (yellow triangle)/pericardial extension (orange arrow), (c) polypoidal growth seen entrance of the right upper lobe bronchus (black star), (d) transbronchial needle in the target lymphnode (Station 7)
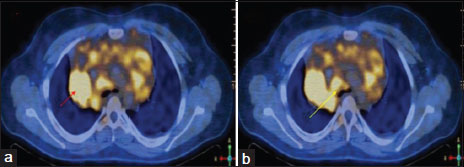
| Figure.2:(a) Positron‑emission tomography–computed tomography of the chest shows significant mediastinal adenopathy with increased radiotracer uptake with a standardized uptake value‑max of 8 (red arrow), (b) positron‑emission tomography‑computed tomography of the chest shows bronchial cut off sign with increased radiotracer uptake with a standardized
References
- Harper PG, Fisher C, McLennan K, Souhami RL. Presentation of Hodgkin's disease as an endobronchial lesion. Cancer 1984; 53: 147-50
- Kern WH, Crepeau AG, Jones JC. Primary Hodgkin's disease of the lung. Report of 4 cases and review of the literature. Cancer 1961; 14: 1151-65
- Pilcher J, Zubair M. Hodgkin's disease and pericardial effusion. Thorax 1970; 25: 631-3
- Retter A, Ardeshna KM, O'Driscoll A. Cardiac tamponade in Hodgkin lymphoma. Br J Haematol 2007; 138: 2
- Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E. et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano classification. J Clin Oncol 2014; 32: 3059-68
- Trédaniel J, Peillon I, Fermé C, Brice P, Gisselbrecht C, Hirsch A. et al. Endobronchial presentation of Hodgkin's disease: A report of nine cases and review of the literature. Eur Respir J 1994; 7: 1852-5
- Gallagher CJ, Knowles GK, Habeshaw JA, Green M, Malpas JS, Lister TA. et al. Early involvement of the bronchi in patients with malignant lymphoma. Br J Cancer 1983; 48: 777-81
- Bashir H, Hudson MM, Kaste SC, Howard SC, Krasin M, Metzger ML. et al. Pericardial involvement at diagnosis in pediatric Hodgkin lymphoma patients. Pediatr Blood Cancer 2007; 49: 666-71


 PDF
PDF  Views
Views  Share
Share

