Determinants of Compliance for Breast and Cervical Cancers Screening among Female Police Personnel of Mumbai, India—A Cross-Sectional Study
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2022; 43(01): 060-067
DOI: DOI: 10.1055/s-0042-1742703
Abstract
Introduction : Women working in police force have unique and vital role to play in law enforcement. Although these women have established a secured place for themselves in the police force, they are exposed to several behavioral and health risks apart from job stress. All these can have potentially serious consequences on their well-being.
Objectives : To determine the compliance to breast and uterine cervical cancers screening and identify predictors of participation in breast and cervical cancers screening among women police personnel.
Materials and Methods : This is a cross-sectional study conducted among the Mumbai police personnel during the period 2019 to 2021. All women working for Mumbai police work force in 12 zones were invited to participate in the study. Temporary clinics for screening were set up in different police stations and eligible participants were enrolled after obtaining written informed consent. This was followed by sociodemographic and risk factor assessment, health education program, screening for common cancers conducted by trained primary health workers (breast by clinical breast examination and uterine cervix by visual inspection with 5%- acetic acid). Screen positives were referred according to predefined referral criteria for further investigations and management.
Results : A total of 3,017 police women were contacted, among them, 2,629 (87.14%) were eligible for screening, 2,609 (99.24%) participated in health education, and 1,839 (69.95%) complied for breast or cervical cancer screening. Further, compliance for screening of breast and uterine cervix were 1,837 (91.67%) and 1,297 (64.72%). A total of 256 (13.94%) and 217 (11.81%) police women were screen positives for breast and cervical cancers. According to multivariate logistic regression analysis, women younger than 50 years, those who were not married or were widowed or separated, postmenopausal women, and those who did not have shift duties had higher compliance for breast and cervix cancers screening.
Conclusion : Good participation for breast and cervical cancers screening was seen among the women police personnel. This study has demonstrated that awareness and screening by simple low-cost methods for breast and cervical cancers screening is easily implementable and can be replicated among the women police force in different states of India.
Keywords
screening - breast cancer - uterine cervix cancers - policeNote
This work is attributed to the Department of Preventive Oncology, Centre for Cancer Epidemiology, Tata Memorial Hospital, Homi Bhabha National Institute, E. Borges Marg, Parel, Mumbai 400012, Maharashtra, India.
Presentations at a Meeting
This work has been presented at the OCCUCON 2019 conference held at Rajkot, Gujarat in January 2019 and the OCCUCON 2020 conference held at Mumbai during January 2020, and the abstracts were published as Abstracts 29 & 50: OCCUCON Abstracts. Indian J Occup Environ Med 2020;24(Suppl S1):21–41. It has also been presented in the Public Health Conference 2021.
Supplementary MaterialPublication History
Article published online:
23 February 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Introduction : Women working in police force have unique and vital role to play in law enforcement. Although these women have established a secured place for themselves in the police force, they are exposed to several behavioral and health risks apart from job stress. All these can have potentially serious consequences on their well-being.
Objectives : To determine the compliance to breast and uterine cervical cancers screening and identify predictors of participation in breast and cervical cancers screening among women police personnel.
Materials and Methods : This is a cross-sectional study conducted among the Mumbai police personnel during the period 2019 to 2021. All women working for Mumbai police work force in 12 zones were invited to participate in the study. Temporary clinics for screening were set up in different police stations and eligible participants were enrolled after obtaining written informed consent. This was followed by sociodemographic and risk factor assessment, health education program, screening for common cancers conducted by trained primary health workers (breast by clinical breast examination and uterine cervix by visual inspection with 5%- acetic acid). Screen positives were referred according to predefined referral criteria for further investigations and management.
Results : A total of 3,017 police women were contacted, among them, 2,629 (87.14%) were eligible for screening, 2,609 (99.24%) participated in health education, and 1,839 (69.95%) complied for breast or cervical cancer screening. Further, compliance for screening of breast and uterine cervix were 1,837 (91.67%) and 1,297 (64.72%). A total of 256 (13.94%) and 217 (11.81%) police women were screen positives for breast and cervical cancers. According to multivariate logistic regression analysis, women younger than 50 years, those who were not married or were widowed or separated, postmenopausal women, and those who did not have shift duties had higher compliance for breast and cervix cancers screening.
Conclusion : Good participation for breast and cervical cancers screening was seen among the women police personnel. This study has demonstrated that awareness and screening by simple low-cost methods for breast and cervical cancers screening is easily implementable and can be replicated among the women police force in different states of India.
Keywords
screening - breast cancer - uterine cervix cancers - policeIntroduction
Globally, breast cancer is the leading cancer among women with estimated 2.3 million new cases, representing 11.7%-of all cancer cases worldwide among both sexes combined. According to the 2020 data, it is also the fifth leading cause of cancer mortality considering both genders and topmost cause of cancer deaths among women. Cervical cancer is the fourth most frequently diagnosed cancer and the fourth leading cause of cancer death in women, with an estimated 604,000 new cases and 342,000 deaths worldwide in 2020. Among Indian women, breast cancer represents the highest incidence and mortality followed by cervical cancer. Indian data on incidence and mortality for breast and cervical cancers are 28.8, 18 and 13.3, 11.4, respectively, per 100,000 women. Every year 178,361 and 123,907 new cases of breast and cervical cancers are diagnosed in India. These two cancers account for 31%-of all cancer cases among women in India.[1] The benefits of screening for breast and cervical cancers are well known (U.S. Preventive Task Force). Screening modalities of breast cancer include clinical breast examination (CBE), self-breast examination, and mammography.[2] Mammography is not feasible as a population-based breast cancer screening method for India because of resource constraints. One of the largest randomized controlled trials (RCTs) on breast cancer screening by CBE conducted in Mumbai has shown significant downstaging of breast cancer at diagnosis. Results show an overall nonsignificant 15%-reduction in breast cancer mortality, while a subset analysis for women older than 49 years shows a significant reduction of 30%-in breast cancer mortality. This 20-year study, that evaluated CBE conducted by trained female health workers in Mumbai, concluded that CBE should be considered for breast cancer screening in low- and middle-income countries (LMICs).[3] Few other trials of CBE in LMICs have also shown that CBE can reduce stage at diagnosis of breast cancer.[4] [5] [6] Screening modalities of cervical cancer include Pap cytology, visual inspection with acetic acid (VIA), and human papillomavirus.[7] Systematic review and meta-analysis conducted by Peirson et al (2013)[8] highlighted effectiveness of screening for reducing incidence and mortality due to cervical cancers and discussed about optimal timing and frequency of screening. Randomized controlled study conducted by Shastri et al demonstrated that VIA performed by primary health workers (PHWs) leads to a statistically significant reduction in cervical cancer mortality.[9] A systematic review on occupational hazards, injuries, and diseases among police officers worldwide has outlined the global impact of occupational hazards, injuries, and diseases in the police force.[10] Some studies have evaluated breast and cervical cancers screening modalities among female armed forces.[11] [12] According to the World Health Organization, noncommunicable diseases (NCDs) are responsible for 71%-of the global mortality each year. More than 85%-of these deaths occur in LMIC settings.[13] With this background, the current study was planned to screen Mumbai police personnel for common cancers and NCDs. Here, we present the data of only women police personnel screened for breast and cervical cancers.
Methodology: Materials and Methods
This is a cross-sectional study, and methodology is shown in [Fig. 1]. Mumbai metropolitan region (MMR) police work force is divided into five regions, namely, south, central, east, west, and north. These regions are further divided into 12 zones. Each zone has 5 to 10 police stations. Prior to the proposed study, the permissions were obtained from all respective police authorities belonging to different police stations for implementing the screening camps in different police stations. A pilot study was conducted in one of the police stations to understand the feasibility of screening Mumbai police. The questionnaire for the same was validated in the pilot study. The main study was planned for a duration of 36 months. The primary objective of the current article is to determine the compliance to screening of breast and uterine cervix cancers among women Mumbai police personnel using low cost and effective technologies. The overall objective of the main study is to formulate a demonstrable and sustainable model on prevention, control, and early detection of breast and cervical cancers among the female police personnel in Mumbai. The PHWs received standardized intensive training in the Department of Preventive Oncology Clinic for 3 weeks before they initiated screening police women. All the eligible women participated in breast and cervical cancers screening, and no sample size was calculated. A total of 3,071 police women working in these police stations were invited for breast and cervical cancers screening. After obtaining informed consent for participating in the study, all the participants were interviewed with a well-structured questionnaire to collect information about their sociodemographic, medical, reproductive, and risk factor history. Detailed health education sessions regarding prevention and early detection for cancers of uterine cervix and breast were conducted for all female police personnel by trained medical social workers. All female police personnel in age group 30 to 65 years were eligible to participate. Any acute or chronic health conditions that may limit the ability of the potential participant to participate in the study were excluded from the study. All female police personnel were offered CBE for breast cancer screening and VIA for cervical cancer screening by trained PHWs. The primary outcome measure was to determine the prevalence of common cancers in this group by conducting screening: breast and uterine cervix for women police personnel. The secondary outcome measure was to formulate a demonstrable and sustainable model on prevention, control, and early detection of breast and cervical cancers among the female police personnel in Mumbai. Compliance in this study refers to adherence to health education or screening. All screen-positive participants were referred to the nodal hospital for further diagnostic investigations and follow-up. Necessary diagnostic confirmatory tests were conducted at the hospital. Predefined referral criteria for breast cancer screening were lump in the breast or under arm, single or multiple duct blood stained nipple discharge, single duct serous nipple discharge, skin changes (peau d'orange appearance/dimpling of skin), recent changes in the nipple or areola (inversion/retraction), nipple eczema, localized thickening/asymmetrical nodularity in postmenopausal women, and palpable supraclavicular or axillary lymph nodes.[14] Referral criteria for uterine cervical cancer screening were VIA positive, postmenopausal bleeding, postmenopausal polyp, postcoital bleeding, intermenstrual bleeding, obvious growth on cervix, and excessive foul smelling white discharge per vagina.[15] All confirmed positive were treated and all confirmed negative cases were advised to follow-up regularly at nodal hospital.
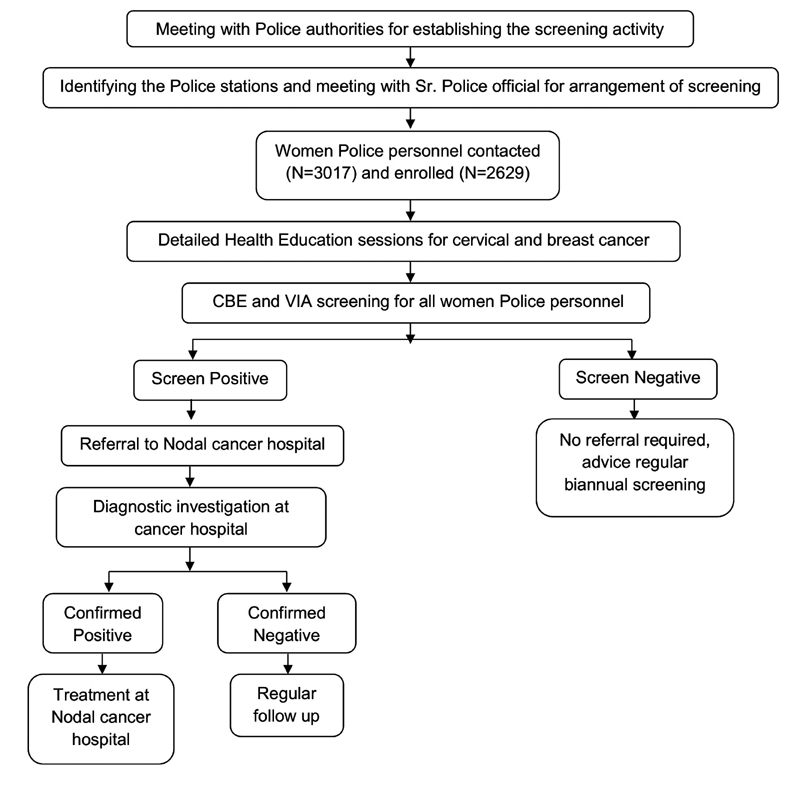
| Fig. 1Study methodology. (CBE) clinical breast examination; (VIA) visual inspection with acetic acid.
Statistical Analysis
The data were entered and analyzed using SPSS version 25.0 (IBM SPSS Statistics, Version 25.0, Armonk, New York, United States: IBM Corp.). Qualitative data were expressed in percentages. The determinants of compliance were analyzed by univariate and multivariate logistic regression analyses to evaluate the effects of various sociodemographic and reproductive characteristics of women on compliance, by estimating odds ratios and their 95%-confidence intervals (CIs). A p-value of <0>
Ethics
The cross-sectional study audit were conducted in accordance with Declaration of Helsinki and Good Clinical Practice as defined by the International Conference on Harmonization. The study was conducted in compliance to the protocol. The cross-sectional study protocol received Tata Memorial Centre Institutional Review Board/Independent Ethics Committee approval prior to initiation of the study dated 26, February 2019. Subject confidentiality was maintained at all times. Ethics committee approval was received, and the trial was registered under ClinicalTrials.gov. CTRI/2019/04/018748
Results
A total of 3,017 police personnel from 12 zones under MMR, headquarters, and special branch were eligible for screening. Distribution of sociodemographic and reproductive characteristics among participant women is shown in [Table 1]. The mean age of participant police women was 34.92 ± 7.64 years and median duration of service in police was 10 (interquartile range [IQR] = 7) years. Total 2,194 (83.45%) were married, 2,251 (85.62%) were premenopausal women, 239 (9.09%) were postmenopausal women, and 138 (5.25%) were perimenopausal women. The mean age at menarche and menopause were 14.53 ± 1.39 and 45.51 ± 4.81 years, respectively. Mean age at marriage was 24.68 ± 3.72, and mean age at first child birth was 26.17 ± 3.71. Median number of children was one (IQR = 1.00). Total 1,933 (73.53%) had history of breastfeeding with 24 (IQR = 24) months as median duration of breastfeeding, 462 (17.57%) women had history of gynecological problems, and 122 (4.64%) had history of breast abnormalities.
|
Variables |
N = 2,629 N (%) |
|---|---|
|
Age groups (y) |
|
|
20–25 |
66 (2.51) |
|
26–30 |
825 (31.38) |
|
31–35 |
871 (33.13) |
|
36–40 |
314 (11.94) |
|
41–45 |
196 (7.46) |
|
46–50 |
205 (7.80) |
|
> 50 |
152 (5.78) |
|
Mean age (y) (SD) |
34.92 (7.64) |
|
Duration of service in police (y) |
|
|
< 5 |
239 (9.09) |
|
6–15 |
1,746 (66.41) |
|
16–25 |
437 (16.62) |
|
> 25 |
207 (7.88) |
|
Median age in duration of service (IQR) |
10 (7.00) |
|
Marital status |
|
|
Married |
2,194 (83.45) |
|
Other |
435 (16.55) |
|
Mean age at marriage (SD)[a] |
24.68 (3.72) |
|
Menstrual status[a] |
|
|
Premenopausal |
2,251 (85.62) |
|
Perimenopausal |
138 (5.25) |
|
Postmenopausal |
239 (9.09) |
|
Mean age at menarche (SD)[a] |
14.53 (1.39) |
|
Mean age at menopause (SD)[a] |
45.51 (4.81) |
|
Language |
|
|
Marathi |
2,568 (97.68) |
|
Other |
61 (2.32) |
|
Education |
|
|
Illiterate or primary (1–4) |
14 (0.53) |
|
Secondary or higher secondary (5–12) |
759 (28.87) |
|
Sr. college (13–15) |
1,068 (40.63) |
|
Graduates and higher |
788 (29.97) |
|
Monthly family income in Rs. (per mo) |
|
|
< 20,000 |
14 (0.53) |
|
20,001–50,000 |
1,630 (62.00) |
|
50,001–75,000 |
775 (29.48) |
|
75,001–100,000 |
137 (5.21) |
|
> 100,000 |
73 (2.78) |
|
Shift duty |
|
|
Yes |
1,496 (56.90) |
|
No |
1,133 (43.10) |
|
Median number of shift duties (IQR) |
120 (40.00) |
|
Family history of cancer |
|
|
Yes |
268 (10.19) |
|
No |
2,361 (89.81) |
|
Cancer screening history |
|
|
Yes |
373 (14.19) |
|
No |
2,256 (85.81) |
|
History of breastfeeding[a] |
|
|
Yes |
1,933 (73.53) |
|
No |
695 (26.44) |
|
Mean age at first child birth (SD)[a] |
26.17 (3.71) |
|
Median number of children (IQR)[a] |
1 (1.00) |
|
Median duration of breastfeeding (IQR)[a] |
24(24) |
|
Previous history of breast abnormalities[a] |
|
|
Yes |
122 (4.64) |
|
No |
2,506 (95.32) |
|
Previous history of gynecological problems[a] |
|
|
Yes |
462 (17.57) |
|
No |
2,166 (82.39) |
|
Eligible women |
Women contacted (% of eligible) |
Participation in health education (% of eligible) |
Site |
Eligible women |
Compliance to screening (%) |
Screening +ve (% of screened) |
Screening +ve (% of contacted) |
|---|---|---|---|---|---|---|---|
|
3,017 |
2,629 (87.14) |
2,609 (99.24) |
Breast |
2,004 (76.23) |
1,837 (91.67) |
256 (13.94) |
256 (9.74) |
|
Cervix |
1,297 (64.72) |
217 (11.81) |
217 (8.25) |
|
Variables |
Multivariate analysis |
||
|---|---|---|---|
|
OR |
95% CI |
p-Value |
|
|
Age groups (y) |
|||
|
30–35 |
4.829 |
1.067–21.848 |
0.041 |
|
36–40 |
5.333 |
1.176–24.181 |
0.030 |
|
41–45 |
3.565 |
0.844–15.058 |
0.084 |
|
46–50 |
7.231 |
1.916–27.288 |
0.004 |
|
> 50 |
1 |
||
|
Duration of service in police (y) |
|||
|
< 5 |
0.454 |
0.130–1.594 |
0.218 |
|
6–15 |
0.625 |
0.200–1.950 |
0.418 |
|
16–25 |
1.630 |
0.558–4.766 |
0.372 |
|
> 25 |
1 |
||
|
Marital status |
|||
|
Married |
1 |
||
|
Other |
1.882 |
1.133–3.125 |
0.015 |
|
Menstrual status |
|||
|
Premenopausal |
1 |
||
|
Perimenopausal |
1.269 |
0.532–3.026 |
0.591 |
|
Postmenopausal |
3.447 |
1.045–11.370 |
0.042 |
|
Shift duty |
|||
|
Yes |
1 |
||
|
No |
1.865 |
1.306–2.663 |
0.001 |
|
Breastfeed history |
|||
|
No |
1 |
||
|
Yes |
1.318 |
0.836–2.076 |
0.234 |
References
- Sung H, Ferlay J, Siegel RL. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- US Preventive Task Force recommendation. Accessed September 5, 2021 at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-screening
- Mittra I, Mishra GA, Dikshit RP. et al. Effect of screening by clinical breast examination on breast cancer incidence and mortality after 20 years: prospective, cluster randomised controlled trial in Mumbai. BMJ 2021; 372: n256
- Sankaranarayanan R. Screening for cancer in low- and middle-income countries. Ann Glob Health 2014; 80 (05) 412-417
- Devi BC, Tang TS, Corbex M. Reducing by half the percentage of late-stage presentation for breast and cervix cancer over 4 years: a pilot study of clinical downstaging in Sarawak, Malaysia. Ann Oncol 2007; 18 (07) 1172-1176
- Sankaranarayanan R, Ramadas K, Thara S. et al. Clinical breast examination: preliminary results from a cluster randomized controlled trial in India. J Natl Cancer Inst 2011; 103 (19) 1476-1480
- US Preventive Task Force recommendation. Accessed September 5, 2021 at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cervical-cancer-screenings
- Peirson L, Fitzpatrick-Lewis D, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev 2013; 2 (01) 35
- Shastri SS, Mittra I, Mishra GA. et al. Effect of VIA screening by primary health workers: randomized controlled study in Mumbai, India. J Natl Cancer Inst 2014; 106 (03) dju009
- Mona GG, Chimbari MJ, Hongoro C. A systematic review on occupational hazards, injuries and diseases among police officers worldwide: policy implications for the South African Police Service. J Occup Med Toxicol 2019; 14 (01) 2
- Merdiemah GE. Breast Cancer Screening among Female Personnel of the Ghana Armed Forces, Accra (PHD dissertation, University of Ghana).
- Naicker K, Hawes R. Cervical cancer screening in the Canadian armed forces: an estimation of screening participation rates using the CF-HERO surveillance system. Cancer Epidemiol 2020; 65: 101670
- WHO factsheet on NCDs [Internet]. [Cited September 18, 2018]. Accessed August 6, 2021 at: http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- Basset AA. Physical examination of the breast and breast self-examination. In: Miller AB. ed. Screening for Cancer. Orlando: Academic Press; 1985
- Sankaranarayan R, Wesley R. A Practical Manual on Visual Screening for Cervical Neoplasia. IARC Technical Publication No. 41. Lyon: IARC Press; 2003
- Braun LA, Kennedy HP, Sadler LS, Dixon J, Womack J, Wilson C. US Navy women's experience of an abnormal cervical cancer screening. J Midwifery Womens Health 2016; 61 (02) 249-256
- Frommelt RA, Peterson MR, O'Leary TJ. A comparison of cervical pathology between United States Air Force women who did and did not serve in the Persian Gulf War. Ann Epidemiol 2000; 10 (05) 285-292
- Dinshaw K, Mishra G, Shastri S. et al. Determinants of compliance in a cluster randomised controlled trial on screening of breast and cervix cancer in Mumbai, India. Oncology 2007; 73 (3–4): 145-153
- Allen JD, Stoddard AM, Mays J, Sorensen G. Promoting breast and cervical cancer screening at the workplace: results from the Woman to Woman Study. Am J Public Health 2001; 91 (04) 584-590
- Amin A, Shriver CD, Henry LR, Lenington S, Peoples GE, Stojadinovic A. Breast cancer screening compliance among young women in a free access healthcare system. J Surg Oncol 2008; 97 (01) 20-24
- Kulkarni SV, Mishra GA, Dusane RR. Determinants of compliance to breast cancer screening and referral in low socio-economic regions of urban India. Int J Prev Med 2019; 10: 84
- Shui Y, Xu D, Liu Y, Liu S. Work-family balance and the subjective well-being of rural women in Sichuan, China. BMC women's health 2020; 20 (01) 1
- Lairson DR, Chan W, Newmark GR. Determinants of the demand for breast cancer screening among women veterans in the United States. Soc Sci Med 2005; 61 (07) 1608-1617
- Natale K, Howard RS, Crothers BA. To Screen or Not to Screen: Presence of High-Grade Squamous Intraepithelial Lesions or Worse in a Regional Military/Beneficiary Population Under 21 Years of Age. J Am Soc Cytopathol 2013; 1 (02) S39-40
- Braun LA, Kostas-Polston EA, Miedema J, Hoffecker L, Wilson C. A scoping review of cervical cancer risk factors, prevention, diagnosis, and treatment in U.S. Active Duty Military Women. Womens Health Issues 2021; 31 (Suppl. 01) S53-S65
- Thomson BA, Nielsen PE. Women's health care in Operation Iraqi Freedom: a survey of camps with echelon I or II facilities. Mil Med 2006; 171 (03) 216-219
Address for correspondence
Publication History
Article published online:
23 February 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2,
Noida-201301 UP, India
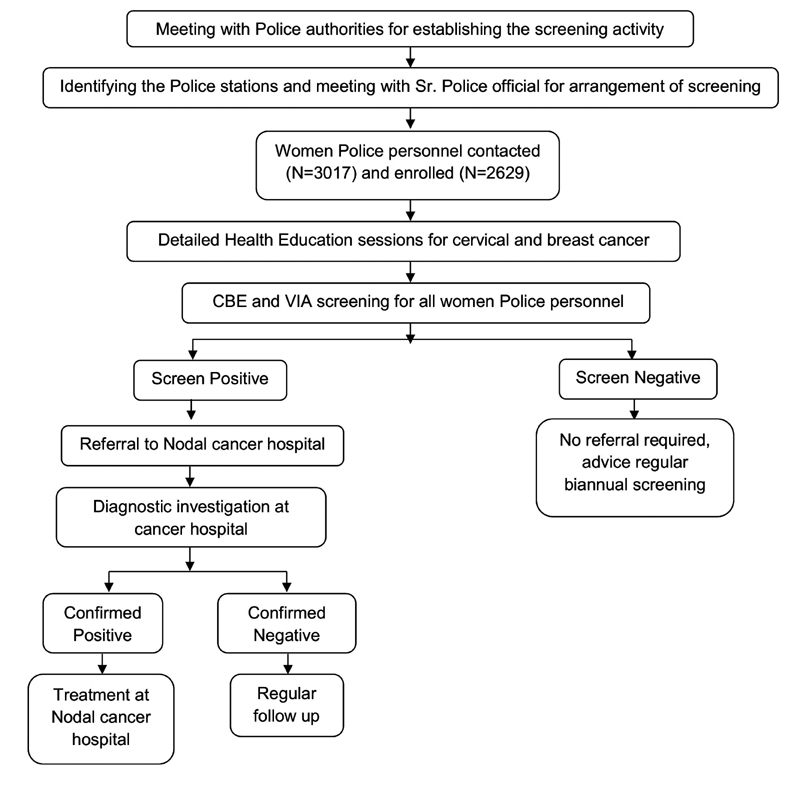
| Fig. 1Study methodology. (CBE) clinical breast examination; (VIA) visual inspection with acetic acid.
References
- Sung H, Ferlay J, Siegel RL. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- US Preventive Task Force recommendation. Accessed September 5, 2021 at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-screening
- Mittra I, Mishra GA, Dikshit RP. et al. Effect of screening by clinical breast examination on breast cancer incidence and mortality after 20 years: prospective, cluster randomised controlled trial in Mumbai. BMJ 2021; 372: n256
- Sankaranarayanan R. Screening for cancer in low- and middle-income countries. Ann Glob Health 2014; 80 (05) 412-417
- Devi BC, Tang TS, Corbex M. Reducing by half the percentage of late-stage presentation for breast and cervix cancer over 4 years: a pilot study of clinical downstaging in Sarawak, Malaysia. Ann Oncol 2007; 18 (07) 1172-1176
- Sankaranarayanan R, Ramadas K, Thara S. et al. Clinical breast examination: preliminary results from a cluster randomized controlled trial in India. J Natl Cancer Inst 2011; 103 (19) 1476-1480
- US Preventive Task Force recommendation. Accessed September 5, 2021 at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cervical-cancer-screenings
- Peirson L, Fitzpatrick-Lewis D, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev 2013; 2 (01) 35
- Shastri SS, Mittra I, Mishra GA. et al. Effect of VIA screening by primary health workers: randomized controlled study in Mumbai, India. J Natl Cancer Inst 2014; 106 (03) dju009
- Mona GG, Chimbari MJ, Hongoro C. A systematic review on occupational hazards, injuries and diseases among police officers worldwide: policy implications for the South African Police Service. J Occup Med Toxicol 2019; 14 (01) 2
- Merdiemah GE. Breast Cancer Screening among Female Personnel of the Ghana Armed Forces, Accra (PHD dissertation, University of Ghana).
- Naicker K, Hawes R. Cervical cancer screening in the Canadian armed forces: an estimation of screening participation rates using the CF-HERO surveillance system. Cancer Epidemiol 2020; 65: 101670
- WHO factsheet on NCDs [Internet]. [Cited September 18, 2018]. Accessed August 6, 2021 at: http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- Basset AA. Physical examination of the breast and breast self-examination. In: Miller AB. ed. Screening for Cancer. Orlando: Academic Press; 1985
- Sankaranarayan R, Wesley R. A Practical Manual on Visual Screening for Cervical Neoplasia. IARC Technical Publication No. 41. Lyon: IARC Press; 2003
- Braun LA, Kennedy HP, Sadler LS, Dixon J, Womack J, Wilson C. US Navy women's experience of an abnormal cervical cancer screening. J Midwifery Womens Health 2016; 61 (02) 249-256
- Frommelt RA, Peterson MR, O'Leary TJ. A comparison of cervical pathology between United States Air Force women who did and did not serve in the Persian Gulf War. Ann Epidemiol 2000; 10 (05) 285-292
- Dinshaw K, Mishra G, Shastri S. et al. Determinants of compliance in a cluster randomised controlled trial on screening of breast and cervix cancer in Mumbai, India. Oncology 2007; 73 (3–4): 145-153
- Allen JD, Stoddard AM, Mays J, Sorensen G. Promoting breast and cervical cancer screening at the workplace: results from the Woman to Woman Study. Am J Public Health 2001; 91 (04) 584-590
- Amin A, Shriver CD, Henry LR, Lenington S, Peoples GE, Stojadinovic A. Breast cancer screening compliance among young women in a free access healthcare system. J Surg Oncol 2008; 97 (01) 20-24
- Kulkarni SV, Mishra GA, Dusane RR. Determinants of compliance to breast cancer screening and referral in low socio-economic regions of urban India. Int J Prev Med 2019; 10: 84
- Shui Y, Xu D, Liu Y, Liu S. Work-family balance and the subjective well-being of rural women in Sichuan, China. BMC women's health 2020; 20 (01) 1
- Lairson DR, Chan W, Newmark GR. Determinants of the demand for breast cancer screening among women veterans in the United States. Soc Sci Med 2005; 61 (07) 1608-1617
- Natale K, Howard RS, Crothers BA. To Screen or Not to Screen: Presence of High-Grade Squamous Intraepithelial Lesions or Worse in a Regional Military/Beneficiary Population Under 21 Years of Age. J Am Soc Cytopathol 2013; 1 (02) S39-40
- Braun LA, Kostas-Polston EA, Miedema J, Hoffecker L, Wilson C. A scoping review of cervical cancer risk factors, prevention, diagnosis, and treatment in U.S. Active Duty Military Women. Womens Health Issues 2021; 31 (Suppl. 01) S53-S65
- Thomson BA, Nielsen PE. Women's health care in Operation Iraqi Freedom: a survey of camps with echelon I or II facilities. Mil Med 2006; 171 (03) 216-219


 PDF
PDF  Views
Views  Share
Share

