Cytological study of palpable breast lumps presenting in an Indian rural setup
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2014; 35(02): 159-164
DOI: DOI: 10.4103/0971-5851.138993
Abstract
Introduction: Benign as well as malignant breast lesions are quite common in Indian population. It is the second most common cancer site after cancer cervix. Fine-needle aspiration cytology (FNAC) is safe, reliable, and time saving outdoor procedure with little discomfort to the patient. FNAC is useful in diagnosis and further planning of treatment without need for biopsy. The current study was carried out with aims of studying the frequency of various breast lesions on FNAC in a rural area in India and its histopathological correlation. Materials and Methods: This was 2 years prospective study carried out from May 2010 to April 2012. Physical examination of breast mass by palpation was done. Smears were stained with May-Grunwald Giemsa and Papanicolaou stain. Results: Of the 225 cases, 131 were in the benign category and 65 belonged to the malignant category, while the cytology study of 13 cases was unsatisfactory. Seventy-six cases were available for histological correlation. Of 29 cytological benign cases, 26 were confirmed as benign, but 3 turned out to be malignant. Out of 36 cytological malignant cases, 35 were confirmed as malignant. FNAC was 88.37% sensitive and 96.42% specific in diagnosing malignant lesions. Conclusion: Fine-needle aspiration cytology is a rapid and effective method for the primary categorization of palpable breast lumps into benign, malignant, atypical, suspicious, and unsatisfactory categories. Benign breast lesions are common than malignant lesions. Histological correlation indicated FNAC to be a good diagnostic tool.
Keywords
Benign lesion - breast - fine needle aspiration cytology - histopathology - malignant lesionPublication History
Article published online:
19 July 2021
© 2014. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Introduction:
Benign as well as malignant breast lesions are quite common in Indian population. It is the second most common cancer site after cancer cervix. Fine-needle aspiration cytology (FNAC) is safe, reliable, and time saving outdoor procedure with little discomfort to the patient. FNAC is useful in diagnosis and further planning of treatment without need for biopsy. The current study was carried out with aims of studying the frequency of various breast lesions on FNAC in a rural area in India and its histopathological correlation.
Materials and Methods:
This was 2 years prospective study carried out from May 2010 to April 2012. Physical examination of breast mass by palpation was done. Smears were stained with May-Grunwald Giemsa and Papanicolaou stain.
Results:
Of the 225 cases, 131 were in the benign category and 65 belonged to the malignant category, while the cytology study of 13 cases was unsatisfactory. Seventy-six cases were available for histological correlation. Of 29 cytological benign cases, 26 were confirmed as benign, but 3 turned out to be malignant. Out of 36 cytological malignant cases, 35 were confirmed as malignant. FNAC was 88.37% sensitive and 96.42% specific in diagnosing malignant lesions.
Conclusion:
Fine-needle aspiration cytology is a rapid and effective method for the primary categorization of palpable breast lumps into benign, malignant, atypical, suspicious, and unsatisfactory categories. Benign breast lesions are common than malignant lesions. Histological correlation indicated FNAC to be a good diagnostic tool.
INTRODUCTION
Diseases of breast, with their uncertain causes and confusion of treatments, have intrigued physicians and medical historians throughout the ages. As an appendage of the skin, it usually reveals its disorders to touch or sight.
Evaluating a breast mass can be a difficult task. It may be difficult for the patient because of the anxiety associated with her underlying fear of a breast malignancy, and it may be difficult for the physician to be confident of the fact that what he or she is palpating is truly a mass, rather than a variation of normal breast parenchyma. Majority of breast symptoms or lesions will prove to be of a benign etiology. Physical, psychological and financial costs of investigating benign breast disease, primarily to exclude malignancy are substantial.
Benign as well as malignant breast lesions are quite common in Indian population. It is the second most common cancer site after cancer cervix in Indian females. Currently, 75,000 new cases of breast cancer are detected in India yearly.[1] This figure must be viewed against the backdrop that the National Cancer Registry and the Hospital-based Tumor Registries hardly sample 3% of the total population. Locally advanced breast cancer constitutes >50-70% of the patients presenting for treatment.[1] The information on the epidemiology of breast cancer in India is very limited, except for a few reports on limited samples.
Fine-needle aspiration cytology (FNAC) method was introduced as a primary test in the diagnosis of breast carcinoma. The procedure is safe, reliable and time saving outdoor procedure with little discomfort to the patient. FNAC is not only useful in diagnosis and further planning of treatment without need for biopsy, but also helpful in prognostication of the tumor factors such as nuclear grading, mitotic index, hormone receptor status and DNA contents. The slides can be prepared by cytospin method or thin prep method.[2]
The current study was carried out with aims of studying the frequency of various breast lesions on FNAC in a rural area and its histopathological correlation.
MATERIALS AND METHODS
This prospective study was carried out from May 2010 to April 2012. Appropriate approval of the institutional ethical committee was obtained for the same. Informed written consent from each patient was also obtained in local language. The subjects concerned included all the female patients which were referred to the Department of Pathology for FNAC of breast mass. Physical examination of breast mass by palpation was done. FNAC was done by using 23 Gauge needle (Becton & Dickinson India Private Limited) attached to 10cc disposable syringe. Air-dried smears were fixed and stained with May-Grunwald Giemsa technique. One smear was fixed with 95% alcohol for Papanicolaou stain.
The patients were followed up for mastectomy or biopsy. Histopathological findings were noted. The statistical analyses were done to find the ability of FNAC to detect the presence of malignancy in the breast in comparison to histopathology. For this sensitivity, specificity, positive and negative predictive value and accuracy/efficiency were calculated.
RESULTS
During the study period May 2010 to April 2012 of this study, a total of 225 FNAC's of breast were done.
The cytological spectrum of various palpable breast lesions in the present study shows that out of the total 225 cases, 131 were in the benign category, 8 were in the atypical category, 8 were in the suspicious category, and 65 belonged to the malignant category while the cytology study of 13 cases was unsatisfactory [Table 1].
Table 1
Cytological spectrum of various palpable breast lesions
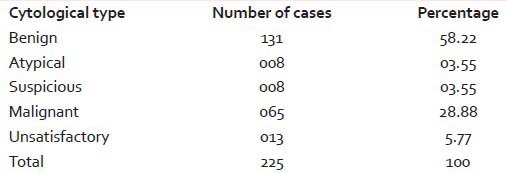
|
The cytological spectrum of various benign breast lesions encountered in the present study shows that out of the total 131 cases that could be satisfactorily labeled as benign in the present study, fibro adenoma accounted for 61 (46.56%) cases, fibrocystic disease for 32 (24.43%) cases, mastitis/breast abscess for 21 (16.03%) cases, galactocele 5 (03.82%) cases, 3 (02.30%) cases showed epithelial hyperplasia, cyst and lipoma 2 (01.52%) cases and fat necrosis, phyllodes tumor, duct papilloma, granular cell tumor, duct ectasia in 1 (00.76%) case each.
On the other hand, the cytological spectrum of various malignant breast lesions encountered in the present study shows that out of the total 65 cases that could be satisfactorily labeled as malignant, infiltrating ductal carcinoma (IDC) accounted for 55 (84.62%) cases, mucinous carcinoma for 4 (6.15%) cases, poorly differentiated carcinoma for 2 (3.07%) cases and medullary carcinoma, lobular carcinoma, metastasis, and lymphoma for 1 (1.53%) case each.
Benign lesions were seen in age group of 19-50 years; whereas suspicious and malignant cases are seen in age group of 31-70 years. Right and left both sides were almost equally involved by the different types of cytological lesions. Upper and outer quadrant is the most commonly involved quadrant by all types of cytological lesions.
The histopathological spectrum in present study showed that out of the total 76 patients (100%) who had a histopathological correlation, 31 (40.78%) were from the benign category and 45 (59.22%) were from the malignant category.
Out of 225 cases of cytopathological study in the in present study, 76 cases were available for histopathological correlation. Out of 29 cytological benign cases, 26 were confirmed as benign on histopathology, but 3 turned out to be malignant. Out of 3 cytological atypical cases, one was benign, and 2 were malignant. All 3 cytological suspicious cases were confirmed as malignant. Out of 36 cytological malignant cases, 35 were confirmed as malignant, but one turned out as benign, while in 5 cytological unsatisfactory cases, 3 were benign and 2 were malignant histopathologically [Table 2].
Table 2
Histopathological correlation with cytopathological spectrum of lesions
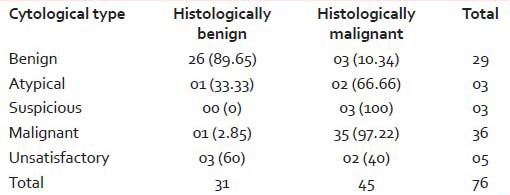
|
The histopathological correlation with benign lesions on cytology as seen in the present study indicated that out of the total 18 (100%) cases of fibro adenoma that had a histopathological correlation, 11 (61.11%) were confirmed as fibro adenoma and 7 (38.88%) were found to be fibrocystic disease. Of the 4 (100%) cases of fibrocystic disease that had a histopathological correlation, 2 (50%) were confirmed fibrocystic disease, while the remaining 2 (50%) were found to be due to IDC. Of the 5 (100%) cases of mastitis/breast abscess that had a histopathological correlation, 4 (80%) were confirmed as mastitis while 1 (20%) was labeled as duct ectasia. The single case of phyllodes tumor on cytology was labeled as angiosarcoma on histopathology. The single case of granular cell tumor on cytology was labeled as fibro adenoma on histopathology.
The histopathological correlation with malignant lesions on cytology as seen in present study indicated that out of the total 32 (100%) cases of IDC that had a histopathological correlation, 30 (93.75%) were confirmed as IDC and one each (3.12%) was found to be due to mastitis and medullary carcinoma respectively. The solitary cases of medullary carcinoma, lobular carcinoma and lymphoma on cytology were confirmed to be true on histopathology, but the single case of poorly differentiated carcinoma on cytology was confirmed as lobular carcinoma on histopathology.
The statistical analyses of FNAC as a diagnostic test to detect the presence of malignancy in the breast were done. FNAC was 88.37% sensitive and 96.42% specific in diagnosing malignant lesions. Furthermore, FNAC had positive predictive value of 97.43% and a negative predictive value of 84.37% in diagnosing malignant lesion. In the present study, it had an accuracy/efficiency of 91.54%.
Imaging spectrum of the lesions is demonstrated in [Figures [Figures11--55].
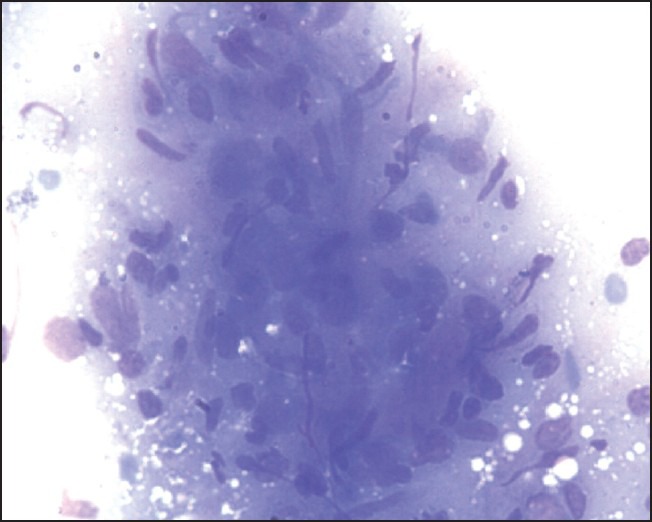
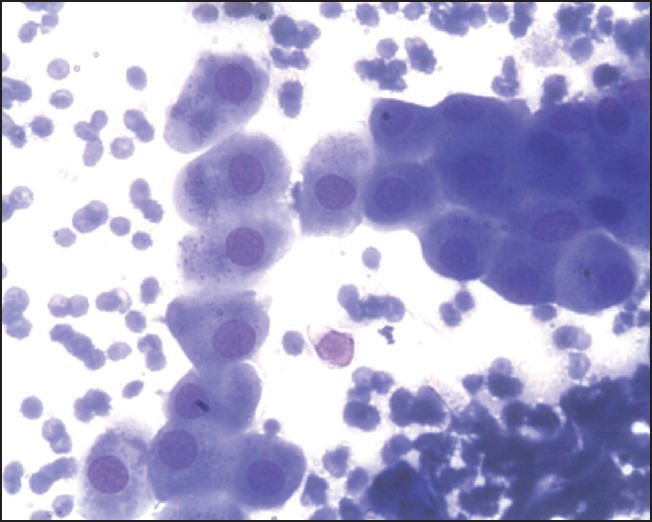
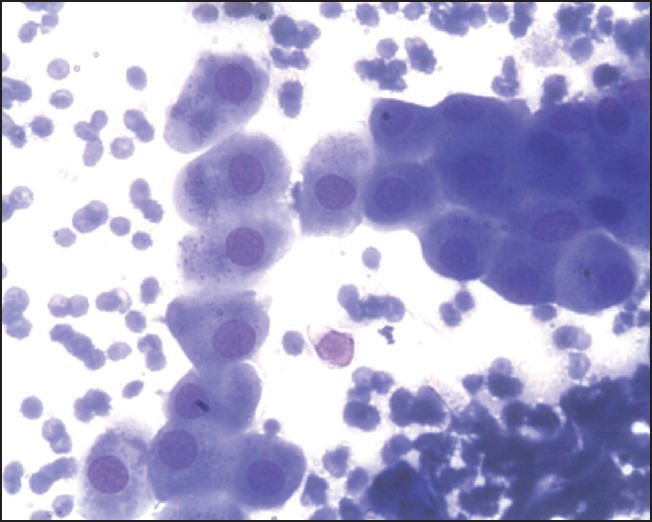
| Figure 1:Granulomatous mastitis May-Grunwald Giemsa, HP
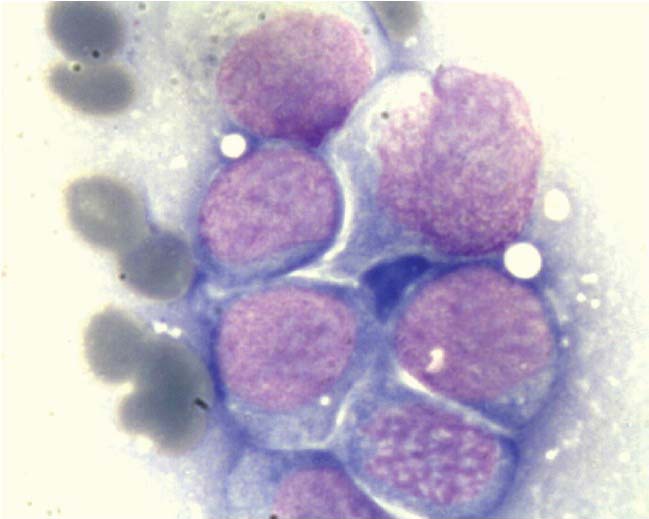
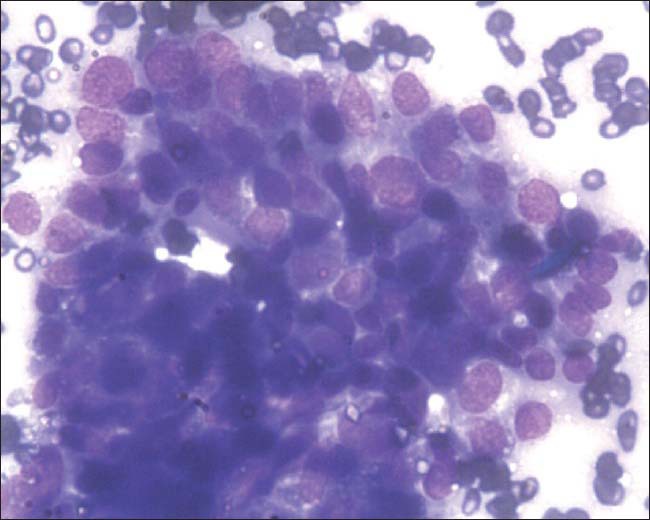
| Figure 5:Primary breast lymphoma, May-Grunwald Giemsa, oil immersion
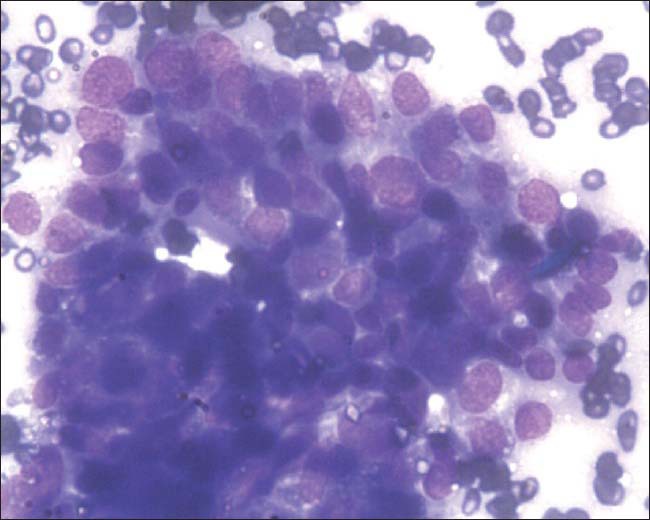
| Figure 2:Granular cell tumor May-Grunwald Giemsa, HP
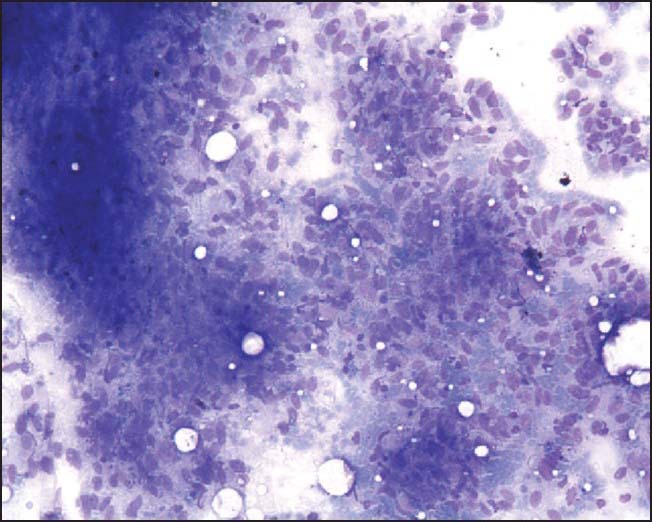
| Figure 3:Phylloides tumor, May-Grunwald Giemsa, HP
| Figure 4:Atypical ductal hyperplasia, May-Grunwald Giemsa, HP
DISCUSSION
The present study accounted for less number of benign cases and more number of malignant cases than Mohammed et al.,[3] Yeoh and Chan,[4] Park and Ham,[5] Rocha et al.[6] and Domínguez et al.[7] One possible cause is, present study is carried out in tertiary cancer hospital in rural area and has higher referrals of patients with diagnosed or likely to be diagnosed breast cancers. In rural area, patient may not be coming with small lesions. Simultaneously, it is also possible that this might be an incidental finding in the period of the present study. Incidence of suspicious lesions was more in this study when compared to others. The rates of atypical lesions in present study are almost same as that in other studies. Although the finding of unsatisfactory lesions in the present study is more than in the study by Mohammed et al.,[3] it still is much less than the majority of other studies [Table 3].
Table 3
Cytological cases
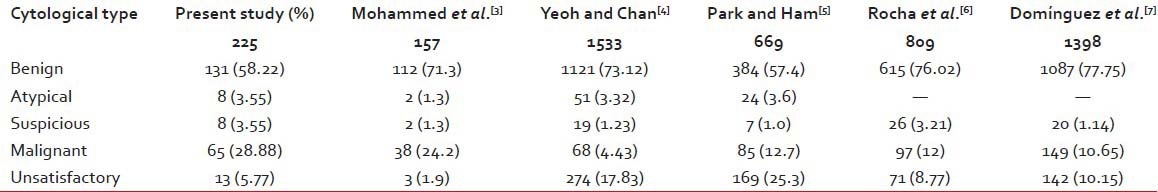
|
In the present study, fibroadenoma (46.56%) followed by fibrocystic disease (24.43%) and mastitis/breast abscess (16.03%) were the most common breast lesions on cytology, which is in agreement with Domínguez et al.[7] (34.49%, 32.17% and 1.55% respectively). Whereas in study by Tiwari[8] and Qasim et al.,[9] fibroadenoma (56.25% and 82.14%) followed by mastitis/breast abscess (20.31% and 10.71%) and fibrocystic disease (7.81% and 3.57%) were the most common breast lesion.
In the present study, 65 malignant lesions were seen, while in study by Domínguez et al.,[7] 147 cases were seen. IDC was most common in the present study with 55 (88.60%) cases in present study and 141 (95.91%) in study by Domínguez et al.[7] Mucinous carcinoma was second most common tumor in this study with 4 (6.15%) cases while in study by Domínguez et al.,[7] it was seen in 1 (0.68%) case. Lobular carcinoma was seen in only 1 (1.53%) case in this study, while it was second common tumor in study by Domíngue et al. with 4 (2.72%) cases.[7]
As overall pattern of type of malignancy with IDC accounting for >85%-cases in both studies, generally there is a tendency not to sub classify malignant tumors on FNAC. Zuk et al. in 1989[10] classified all aspirates into the following groups: Inadequate: Either extremely hypocellular with regard to epithelial cells or bloodstained to an extent that all other elements are obscured. Benign: Characterized by sheets of regular ductal cells with nuclear features of benign cells, often admixed with a large number of “stripped” nuclei. Suspicious: Hyper cellular specimen, which had an admixture of regular cells and others with abnormal nuclear and cytoplasm features falling short of a firm diagnosis of malignancy. Malignant: Hyper cellular specimen comprising cells with unequivocal cytological features of malignancy. In 2000, Tabbara et al.[11] recommended in the national comfort institute conference the use of a standardized approach for the reporting of breast FNAs. The classification system proposed at the conference places breast FNAs into one of five categories:
- Benign
- Atypical/indeterminate
- Suspicious/probably malignant
- Malignant
- Unsatisfactory.
In the present study, maximum numbers of cytologically benign lesions were seen in the age group ranging from 19 to 50 years. This was similar to the findings by Khemka et al.[12] and Rocha et al.[6] who had maximum cytological benign cases in the age groups 15-44 years and 14-40 years respectively. MacIntosh et al.[13] had majority of benign cases in the age group 27-77 years. Maximum atypical category lesions were seen in the age group 21-70 years in the present study, while other studies do not mention this category in their study. In the present study, cytological suspicious lesions were most common in the age group 31-70 fs almost similar findings have been reported by MacIntosh et al.[13] and Rocha et al.,[6] who reported maximum number of suspicious cases in the age groups 33-75 years and 31-75 years, respectively. Malignant lesions were common in the age groups 31-70 years in the present study, 35-84 years in the study by Khemka et al.,[12] 63-79 years in the study by MacIntosh et al.[13] and 41-75 years in the study by Rocha et al.[6] Unsatisfactory lesions were common in the age groups 21-60 years in the present study and 14-50 years in the study by Rocha et al.[6] So overall pattern of occurrence is as expected with benign lesions are seen in younger age group and suspicious and malignant in older age group.
In the present study, both sides (right and left) were almost equally involved by the different types of cytological lesions. This is in contrast with the findings of Meena et al.,[2] Reddy and Reddy[14] and Clegg-Lamptey and Hodasi[15] in which the left side was slightly more common.
Upper and outer quadrant was the most commonly involved quadrant (46.28%) in the present study. This is in agreement with the findings of other studies like Rocha et al.[6] (45.20%), Zuk et al.[10] (42.20%), Reddy and Reddy[14] (54.20%), Meena et al.[2] (54%) and Clegg-Lamptey and Hodasi[15] (42.40%). The exact cause of this finding is not known.
In the present study, less benign cases and more malignant were found histologically than studies by Mohammed et al.,[3] Kim et al.,[16] Park and Ham[5] and Choi et al.[17] [Table 4]. This higher number of benign and lower number of malignant cases in other studies may be due to good follow up or more awareness amongst the patients. The present study is from rural area, so benign lesions on cytology may not have come for operations.
Table 4
Histological cases
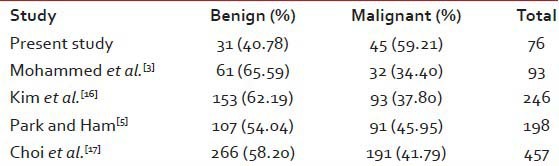
|
As per present study fibrocystic disease can be misinterpreted as fibroadenoma on cytology. This may occur because of clinical appearance of fibrocystic disease as a localized lesion. IDC on cytology may appear as fibrocystic disease. This may be due to FNAC done from nonrepresentative area. Angiosarcoma was identified as phylloides tumor. Exact cause could not be determined, but may be due to less cellular smear with more stroma.
As per this study IDC on histopathology can be identified as IDC on cytology. As the representative area is less, it is difficult to identify medullary carcinoma on cytology. Sometimes, lobular carcinoma can appear as poorly differentiated carcinoma, as no pattern is seen. Sometimes, mastitis cases can be confused with IDC. This may be because, in the background to heavy inflammation; few cells may appear more atypical. The exact cause of poor cellularity in some benign or, malignant cases cannot be determined. The findings of Dey and Luthra in 1999 indicate that the presence of associated fibrocystic disease may be misleading because it can mask a malignancy. Hypocellularity and relatively mild nuclear atypia are the most common reasons for failure to diagnosis a malignant breast lesion. In these cases careful attention to extreme nuclear monomorphism and absence of naked bipolar cells along with radiologic suspicion should suggest a diagnosis of malignancy.[18,19]
In the present study, sensitivity was more than the study by Choi et al.[17] and Park and Ham[5] but less than study by Mohammed et al.[3] and Kim et al.[16] In the present study, specificity was more than the study by Park and Ham[5] and Kim et al.[16] but less than study by Mohammed et al.[3] and Choi et al.[17] In the present study, positive predictive value was more than the study by Kim et al.[16] but less than study by Choi et al.[17] and Mohammed et al.[3] In the present study, negative predictive value was less than the study by Choi et al.,[17] Mohammed et al.[3] and Kim et al.[16] [Table 5]. Hence overall, all have good sensitivity, specificity, positive and negative predictive value.
Table 5
Statistical analyses of FNAC as a diagnostic test
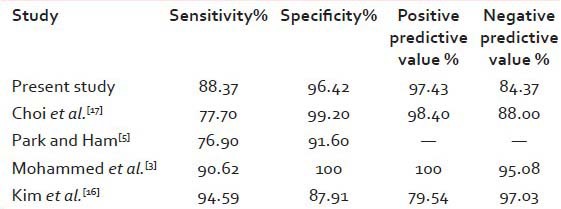
|
Certain constraints and clarifications that need mention are: “Is FNAC adequate for diagnosis?” In this study, there was only one case (out of 36) that was false positive for malignancy based on FNAC's. This case on histopathology (lumpectomy) was diagnosed as mastitis. Hence, the specificity (probability that a test result will be negative when the disease is not present and is given by the ratio of true negative to the sum of true negative and false positive) of the test becomes high. This ensures that no patient undergoes a mutilating surgery for cancer of the breast based on the FNAC report alone.
In this study, we have realized that one cannot overlook the importance of clinical and radiological assessment for diagnosing breast lumps. This is especially so in cases that is labeled on cytology as atypical or suspicious. In such conditions, triple assessment (which assigns a score to a breast lesion by taking into consideration the clinical diagnosis, mammography diagnosis and the cytology diagnosis together and not any one diagnosis in isolation) is must. Triple test is particularly beneficial in a false negative scenario, in which the clinical decision to undertake a biopsy is usually based on index of suspicion and radiological imaging. This usually manifests as a concordance in clinical and imaging based diagnosis and discordance in clinical and cytological or imaging and cytological diagnosis.
The general protocol in this hospital is that any patient with lump in breast is visits a surgeon who then clinically examines the patient and makes a clinical diagnosis. Then a mammogram is performed in the Department of Imaging. After that the patient undergoes FNAC. The patient then returns to surgeon with reports of FNAC and mammogram. The surgeons then operate for cancer based on the FNAC report.
Of the 65 “FNAC positive for malignancy” cases, the histopathology follow-up of only 36 cases was available as only these patients underwent surgery for breast cancer in this institute. Remaining 29 cases were lost as some of them were not operated due to advanced stage of malignancy, some preferred surgery at outside centers that were convenient to them and some refused surgery and turned to unconventional healing techniques.
Of these 36 cases that were found to be positive for malignancy on FNAC, 35 were confirmed as malignant on high platelet reactivity (HPR). Thus there was high concordance between the cases with final HPR, in spite of these limitations.
CONCLUSION
Fine-needle aspiration cytology is a rapid and effective method for the primary categorization of palpable breast lumps into benign, malignant, atypical, suspicious, and unsatisfactory categories. Benign breast lesions are common than malignant lesions, fibro adenoma and fibrocystic disease are more common in benign disease, whereas IDC accounts for the highest number of malignant lesions. Histological correlation indicated FNAC to be a good diagnostic tool.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- Chopra R. The Indian scene. J Clin Oncol 2001;19:106-11.
- Meena SP, Hemrajani DK, Joshi N. A comparative and evaluative study of cytological and histological grading system profile in malignant neoplasm of breast - An important prognostic factor. Indian J Pathol Microbiol 2006;49:199-202.
- Mohammed AZ, Edino ST, Ochicha O, Alhassan SU. Value of fine needle aspiration biopsy in preoperative diagnosis of palpable breast lumps in resource-poor countries: A Nigerian experience. Ann Afr Med 2005;4:19-22.
- Yeoh GP, Chan KW. Fine needle aspiration of breast masses: An analysis of 1533 cases in private practice. Hong Kong Med J 1998;4:283-88.
- Park IA, Ham EK. Fine needle aspiration cytology of palpable breast lesions. Histologic subtype in false negative cases. Acta Cytol 1997;41:1131-8.
- Rocha PD, Nadkarni NS, Menezes S. Fine needle aspiration biopsy of breast lesions and histopathologic correlation. Acta Cytol 1997;41:705-12.
- Domínguez F, Riera JR, Tojo S, Junco P. Fine needle aspiration of breast masses. An analysis of 1,398 patients in a community hospital. Acta Cytol 1997;41:341-7.
- Tiwari M. Role of fine needle aspiration cytology in diagnosis of breast lumps. Kathmandu Univ Med J (KUMJ) 2007;5:215-7.
- Qasim M, Ali J, Akbar SA, Mustafa S. Lump breast: Role of FNAC in diagnosis. Prof Med J 2009;16:235-8.
- ;Zuk JA, Maudsley G, Zakhour HD. Rapid reporting on fine needle aspiration of breast lumps in outpatients. J Clin Pathol 1989;42:906-11.
- Tabbara SO, Frost AR, Stoler MH, Sneige N, Sidawy MK. Changing trends in breast fine-needle aspiration: Results of the Papanicolaou Society of Cytopathology Survey. Diagn Cytopathol 2000;22:126-30.
- Khemka A, Chakrabarti N, Shah S, Patel V. Palpable breast lumps: Fine-needle aspiration cytology versus histopathology: A correlation of diagnostic accuracy. Internet J Surg 2009;18:1.
- MacIntosh RF, Merrimen JL, Barnes PJ. Application of the probabilistic approach to reporting breast fine needle aspiration in males. Acta Cytol 2008;52:530-4.
- Reddy DG, Reddy CRR. Carcinoma of the breast, its incidence and histological variants among South Indians. Indian J Med Sci 1958;12:228-34.
- Clegg-Lamptey J, Hodasi W. A study of breast cancer in korle bu teaching hospital: Assessing the impact of health education. Ghana Med J 2007;41:72-7.
- Kim A, Lee J, Choi JS, Won NH, Koo BH. Fine needle aspiration cytology of the breast. Experience at an outpatient breast clinic. Acta Cytol 2000;44:361-7.
- Choi YD, Choi YH, Lee JH, Nam JH, Juhng SW, Choi C. Analysis of fine needle aspiration cytology of the breast: A review of 1,297 cases and correlation with histologic diagnoses. Acta Cytol 2004;48:801-6.
- Sankaye S, Kachewar S. Pathological panorama of breast cysts. Cukurova Med J 2014;39:458-63.
- Dey P, Luthra UK. False negative cytologic diagnosis of breast carcinoma. Acta Cytol 1999;43:801-5.
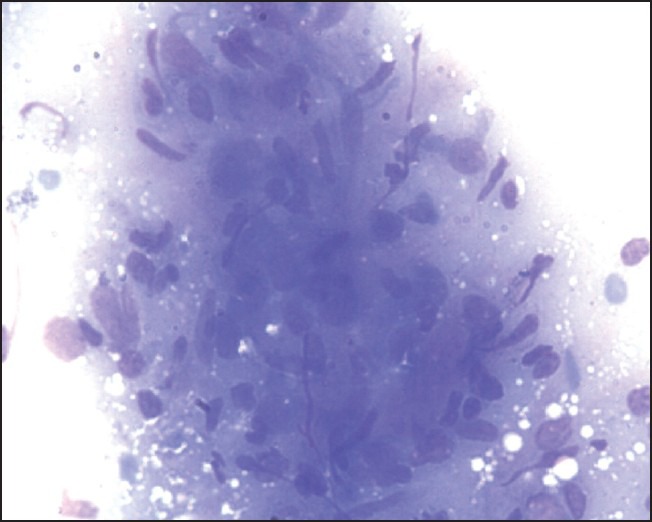
| Figure 1:Granulomatous mastitis May-Grunwald Giemsa, HP
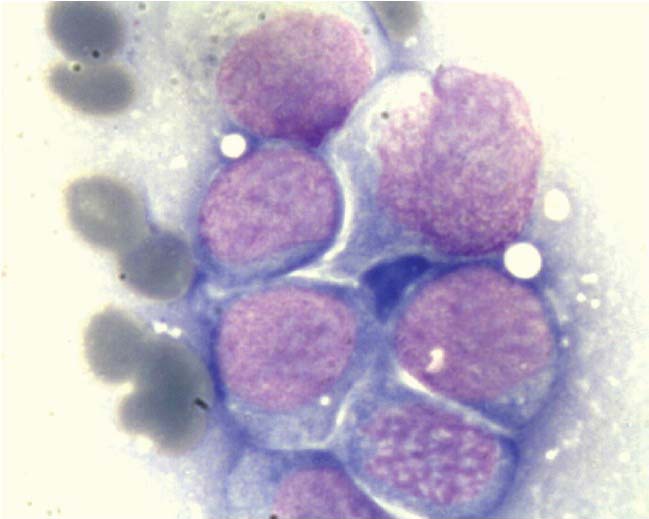
| Figure 5:Primary breast lymphoma, May-Grunwald Giemsa, oil immersion
| Figure 2:Granular cell tumor May-Grunwald Giemsa, HP
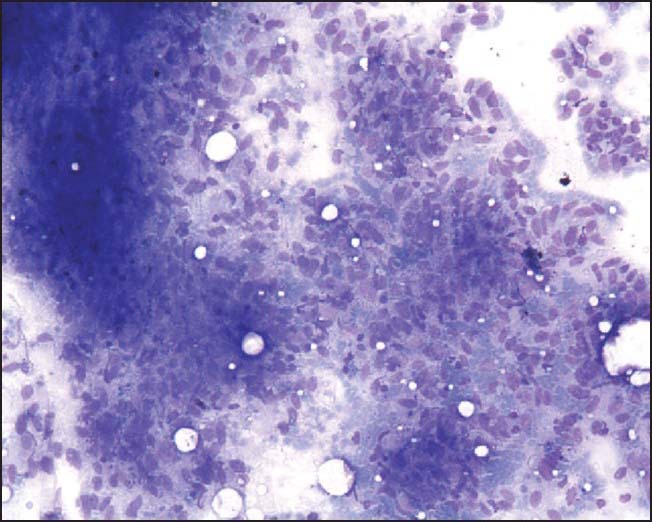
| Figure 3:Phylloides tumor, May-Grunwald Giemsa, HP
| Figure 4:Atypical ductal hyperplasia, May-Grunwald Giemsa, HP
References
- Chopra R. The Indian scene. J Clin Oncol 2001;19:106-11.
- Meena SP, Hemrajani DK, Joshi N. A comparative and evaluative study of cytological and histological grading system profile in malignant neoplasm of breast - An important prognostic factor. Indian J Pathol Microbiol 2006;49:199-202.
- Mohammed AZ, Edino ST, Ochicha O, Alhassan SU. Value of fine needle aspiration biopsy in preoperative diagnosis of palpable breast lumps in resource-poor countries: A Nigerian experience. Ann Afr Med 2005;4:19-22.
- Yeoh GP, Chan KW. Fine needle aspiration of breast masses: An analysis of 1533 cases in private practice. Hong Kong Med J 1998;4:283-88.
- Park IA, Ham EK. Fine needle aspiration cytology of palpable breast lesions. Histologic subtype in false negative cases. Acta Cytol 1997;41:1131-8.
- Rocha PD, Nadkarni NS, Menezes S. Fine needle aspiration biopsy of breast lesions and histopathologic correlation. Acta Cytol 1997;41:705-12.
- Domínguez F, Riera JR, Tojo S, Junco P. Fine needle aspiration of breast masses. An analysis of 1,398 patients in a community hospital. Acta Cytol 1997;41:341-7.
- Tiwari M. Role of fine needle aspiration cytology in diagnosis of breast lumps. Kathmandu Univ Med J (KUMJ) 2007;5:215-7.
- Qasim M, Ali J, Akbar SA, Mustafa S. Lump breast: Role of FNAC in diagnosis. Prof Med J 2009;16:235-8.
- ;Zuk JA, Maudsley G, Zakhour HD. Rapid reporting on fine needle aspiration of breast lumps in outpatients. J Clin Pathol 1989;42:906-11.
- Tabbara SO, Frost AR, Stoler MH, Sneige N, Sidawy MK. Changing trends in breast fine-needle aspiration: Results of the Papanicolaou Society of Cytopathology Survey. Diagn Cytopathol 2000;22:126-30.
- Khemka A, Chakrabarti N, Shah S, Patel V. Palpable breast lumps: Fine-needle aspiration cytology versus histopathology: A correlation of diagnostic accuracy. Internet J Surg 2009;18:1.
- MacIntosh RF, Merrimen JL, Barnes PJ. Application of the probabilistic approach to reporting breast fine needle aspiration in males. Acta Cytol 2008;52:530-4.
- Reddy DG, Reddy CRR. Carcinoma of the breast, its incidence and histological variants among South Indians. Indian J Med Sci 1958;12:228-34.
- Clegg-Lamptey J, Hodasi W. A study of breast cancer in korle bu teaching hospital: Assessing the impact of health education. Ghana Med J 2007;41:72-7.
- Kim A, Lee J, Choi JS, Won NH, Koo BH. Fine needle aspiration cytology of the breast. Experience at an outpatient breast clinic. Acta Cytol 2000;44:361-7.
- Choi YD, Choi YH, Lee JH, Nam JH, Juhng SW, Choi C. Analysis of fine needle aspiration cytology of the breast: A review of 1,297 cases and correlation with histologic diagnoses. Acta Cytol 2004;48:801-6.
- Sankaye S, Kachewar S. Pathological panorama of breast cysts. Cukurova Med J 2014;39:458-63.
- Dey P, Luthra UK. False negative cytologic diagnosis of breast carcinoma. Acta Cytol 1999;43:801-5.


 PDF
PDF  Views
Views  Share
Share

