Cryptococcal meningitis in a human immunodeficiency virus negative patient with follicular lymphoma
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2014; 35(01): 118-119
DOI: DOI: 10.4103/0971-5851.133739
|
Publication History
Article published online:
19 July 2021
© 2014. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Sir,
Cryptococcal infections frequently develop as opportunistic fungal infections in human immunodeficiency virus (HIV) patients and have also been reported in other immunocompromised conditions such as transplant patients, diabetes mellitus, liver cirrhosis and alcoholism. Cryptococcal infections are rare in cancer patients and the literature which consists of only case reports and case series from single institutions.
A 45-year-old male who presented with a history of swellings in the right side of neck since 15 months, headache and diminution of vision, low grade fever and occasional episodes of vomiting since 3 weeks. Clinical examination revealed that patient had bilateral cervical lymphadenopathy. Neurologic examination revealed an alert, oriented patient. His pupils were equal and reacting to light. He had paralysis of the left lateral rectus muscle. Funduscopic examination was normal. However, he had only light perception in both eyes. There were no other neurological deficits.
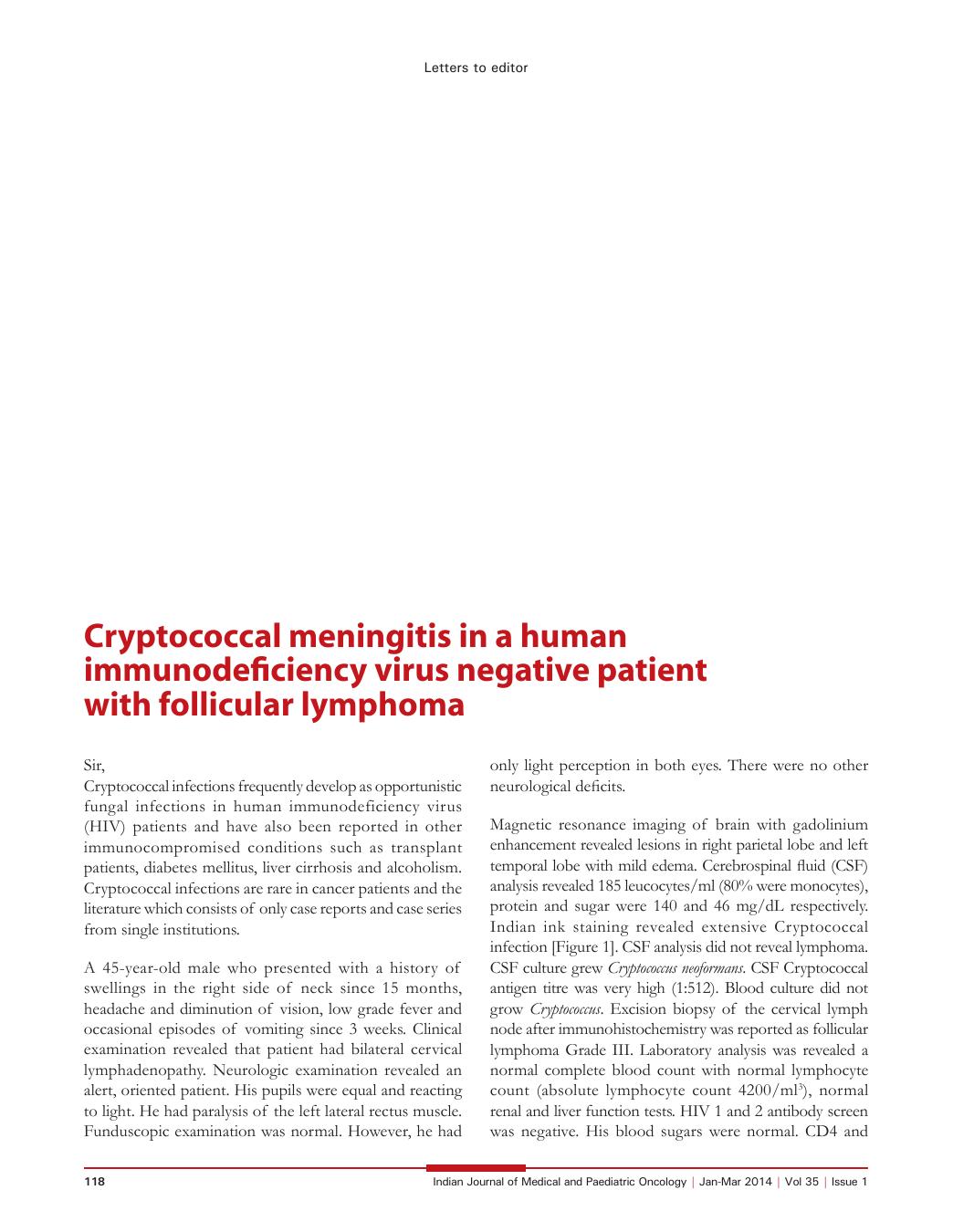
Magnetic resonance imaging of brain with gadolinium enhancement revealed lesions in right parietal lobe and left temporal lobe with mild edema. Cerebrospinal fluid (CSF) analysis revealed 185 leucocytes/ml (80% were monocytes), protein and sugar were 140 and 46 mg/dL respectively. Indian ink staining revealed extensive Cryptococcal infection [Figure 1]. CSF analysis did not reveal lymphoma. CSF culture grew Cryptococcus neoformans. CSF Cryptococcal antigen titre was very high (1:512). Blood culture did not grow Cryptococcus. Excision biopsy of the cervical lymph node after immunohistochemistry was reported as follicular lymphoma Grade III. Laboratory analysis was revealed a normal complete blood count with normal lymphocyte count (absolute lymphocyte count 4200/ml3), normal renal and liver function tests. HIV 1 and 2 antibody screen was negative. His blood sugars were normal. CD4 and CD8 counts were also normal. The patient was started on amphotericin B (1 mg/kg) and tablet fluconazole 800 mg/day. The patient developed poorly controlled generalized tonic clonic seizures and later had fluctuating levels of sensorium. Amphotericin B was given for 14 days without any significant toxicity. Cyclophosphamide, Adriamycin, Vincristine and Prednisolone (CHOP) chemotherapy was given 3 weeks after starting antifungal therapy. However, there was no improvement in his seizures, ophthalmoplegia and vision. Patient was discharged at request and lost to follow-up.
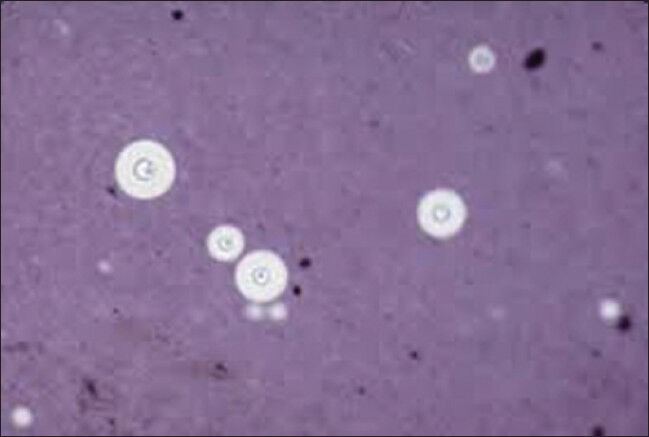
| Figure 1:India ink stain of cerebrospinal fluid showing Cryptococci
Cryptococcosis is infection caused by encapsulated yeast Cryptococcus. Two varieties are recognized: C. neoformans and Cryptococcus gattii. C. neoformans is commonly found world-wide and is the type associated with pigeon excreta. C. neoformans is acquired when aerosolized and inhaled and from respiratory route it causes disseminated disease with predilection for central nervous system, sometimes also involving lungs, bone, prostate, skin, eyes and liver. Cryptococcal meningitis usually presents as fever, malaise, headache, vomiting, meningeal signs, seizures. Visual loss in patients with cryptococcosis may be due to intracranial hypertension, direct infiltration or compression of optic nerve, endophthalmitis and inflammatory adhesions as seen in arachnoiditis.[1]
Records of 31 patients with cancer who developed cryptococcosis during the study period of 1989-1999 were reviewed by Kontoyiannis et al. and they found that hematological malignancy (in 20 patients [65%]) was the most common underlying disease.[2] Pagano et al. from the Gruppo Italiano Malattie Ematologiche dell‘Adulto group reported on 17 cases of cryptococcosis (8 with acute leukemia and 3 with non-Hodgkin lymphoma (NHL)) in patients with hematological malignancies in their 10 year retrospective study.[3] Reisfeld-Zadok et al. reported about Cryptococcal meningitis occurring in 2 patients of chronic lymphocytic leukemia.[4] Korfel et al. reported 2 cases with advanced Hodgkin lymphoma and cryptococcal meningitis.[5] They found that the risk factors for acquiring cryptococcosis in their patients were the presence of hematologic disease >12 months, advanced Stage IV disease, absolute lymphopenia and extensive pretreatment.
The most common risk factor for reduced survival after cryptococcal infection is therapeutic failure. Risk factors for treatment failure are absolute lymphopenia, lymphoreticular malignancies, low white blood cells counts in CSF, high antigen titers in CSF and/or blood, focal palsies, abnormal mental status and sometimes age.[6] Our patient though having normal absolute lymphocyte count had almost all other poor prognostic factors for therapeutic failure.
In conclusion, cryptococcal meningitis is rare in cancer patients. Possible risk factor for our patient to develop cryptococcal meningitis was the prolonged duration of underlying NHL (about 15 months). We are reporting this case due to the rarity of presentation and the fact that he did not have any of the typical risk factors mentioned in the literature.
References
- Prada JL, Torre-Cisneros J, Kindelan JM, Jurado R, Villanueva JL, Navarro M, et al. Deafness and blindness in a HIV-positive patient with cryptococcal meningitis. Postgrad Med J 1996;72:575.
- Kontoyiannis DP, Peitsch WK, Reddy BT, Whimbey EE, Han XY, Bodey GP, et al. Cryptococcosis in patients with cancer. Clin Infect Dis 2001;32:E145-50.
- Pagano L, Fianchi L, Caramatti C, D′Antonio D, Melillo L, Caira M, et al. Cryptococcosis in patients with hematologic malignancies. A report from GIMEMA-infection. Haematologica 2004;89:852-6.
- Reisfeld-Zadok S, Elis A, Szyper-Kravitz M, Chowers M, Lishner M. Cryptococcal meningitis in chronic lymphocytic leukemia patients. Isr Med Assoc J 2009;11:437-9.
- Korfel A, Menssen HD, Schwartz S, Thiel E. Cryptococcosis in Hodgkin′s disease: Description of two cases and review of the literature. Ann Hematol 1998;76:283-6.
- Dromer F, Mathoulin S, Dupont B, Brugiere O, Letenneur L. Comparison of the efficacy of amphotericin B and fluconazole in the treatment of cryptococcosis in human immunodeficiency virus-negative patients: Retrospective analysis of 83 cases. French Cryptococcosis Study Group. Clin Infect Dis 1996;22 Suppl 2:S154-60.
| Figure 1:India ink stain of cerebrospinal fluid showing Cryptococci
References
- Prada JL, Torre-Cisneros J, Kindelan JM, Jurado R, Villanueva JL, Navarro M, et al. Deafness and blindness in a HIV-positive patient with cryptococcal meningitis. Postgrad Med J 1996;72:575.
- Kontoyiannis DP, Peitsch WK, Reddy BT, Whimbey EE, Han XY, Bodey GP, et al. Cryptococcosis in patients with cancer. Clin Infect Dis 2001;32:E145-50.
- Pagano L, Fianchi L, Caramatti C, D′Antonio D, Melillo L, Caira M, et al. Cryptococcosis in patients with hematologic malignancies. A report from GIMEMA-infection. Haematologica 2004;89:852-6.
- Reisfeld-Zadok S, Elis A, Szyper-Kravitz M, Chowers M, Lishner M. Cryptococcal meningitis in chronic lymphocytic leukemia patients. Isr Med Assoc J 2009;11:437-9.
- Korfel A, Menssen HD, Schwartz S, Thiel E. Cryptococcosis in Hodgkin′s disease: Description of two cases and review of the literature. Ann Hematol 1998;76:283-6.
- Dromer F, Mathoulin S, Dupont B, Brugiere O, Letenneur L. Comparison of the efficacy of amphotericin B and fluconazole in the treatment of cryptococcosis in human immunodeficiency virus-negative patients: Retrospective analysis of 83 cases. French Cryptococcosis Study Group. Clin Infect Dis 1996;22 Suppl 2:S154-60.


 PDF
PDF  Views
Views  Share
Share

