Cognizance and utilization about breast cancer screening among the health professional female students and staffs of University Kuala Lumpur, Royal College of Medicine Perak, Malaysia
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(04): 286-292
DOI: DOI: 10.4103/0971-5851.195752
Abstract
Background: Breast cancer (BC) is a major life-threatening problem and a global concern including Malaysia. BC is an equal threat for both developing and developed countries. The aim of this study was to determine the relationship between sociodemographic factors with knowledge, attitude, and perception on BC screening among the females of University Kuala Lumpur, Royal College of Medicine Perak (UniKL RCMP). Materials and Methods: This cross-sectional study was conducted from 2015 to 2016. The populations included were the students and staff of UniKL RCMP. The simple sampling method was used and a set of questionnaire was prepared and distributed to the participants who were willing to participate. The data were analyzed by using the SPSS version 17. Results: Of the 220 only 203 questionnaires were returned. Nearly 87.7% of participants indicated genetic factors as the cause of BC, followed by exposure to carcinogenic and X-ray. Excessive smoking (54.2%) and sedentary lifestyle (52.2%) were the risk factors of the BC. 100% of participants thought that breast self-examination (BSE) is important to detect a breast lump and most of them (76.8%) knew what a mammogram is but only 2.0% went for a mammogram. Chemotherapy (71.9%) and surgery (71.9%) were treatments options according to study participants. Nearly 91.1% agreed that regular mammogram could help to detect BC at an early stage. Nearly 88.2% thought BC is not easily curable. Finally, for the attitude on BC screening, most of them knew how to perform BSE (69.0%) with the frequency of 36.0% doing it once a year. Conclusions: The majority of the participants found the good knowledge on BC and on how to perform BSE. Although most of them knew what a mammogram is, only a few have gone for it since perhaps it is recommended for those who are above 50-year-old. Therefore, researchers believe and trust that there is an urgent need of state-funded multicenter study to prevent and early diagnosis of BC in Malaysia.
Keywords
Awareness - breast cancer screening - females - Malaysia - practice - “University Kuala Lumpur - Royal College of Medicine Perak”Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Background:
Breast cancer (BC) is a major life-threatening problem and a global concern including Malaysia. BC is an equal threat for both developing and developed countries. The aim of this study was to determine the relationship between sociodemographic factors with knowledge, attitude, and perception on BC screening among the females of University Kuala Lumpur, Royal College of Medicine Perak (UniKL RCMP).
Materials and Methods:
This cross-sectional study was conducted from 2015 to 2016. The populations included were the students and staff of UniKL RCMP. The simple sampling method was used and a set of questionnaire was prepared and distributed to the participants who were willing to participate. The data were analyzed by using the SPSS version 17.
Results:
Of the 220 only 203 questionnaires were returned. Nearly 87.7% of participants indicated genetic factors as the cause of BC, followed by exposure to carcinogenic and X-ray. Excessive smoking (54.2%) and sedentary lifestyle (52.2%) were the risk factors of the BC. 100% of participants thought that breast self-examination (BSE) is important to detect a breast lump and most of them (76.8%) knew what a mammogram is but only 2.0% went for a mammogram. Chemotherapy (71.9%) and surgery (71.9%) were treatments options according to study participants. Nearly 91.1% agreed that regular mammogram could help to detect BC at an early stage. Nearly 88.2% thought BC is not easily curable. Finally, for the attitude on BC screening, most of them knew how to perform BSE (69.0%) with the frequency of 36.0% doing it once a year.
Conclusions:
The majority of the participants found the good knowledge on BC and on how to perform BSE. Although most of them knew what a mammogram is, only a few have gone for it since perhaps it is recommended for those who are above 50-year-old. Therefore, researchers believe and trust that there is an urgent need of state-funded multicenter study to prevent and early diagnosis of BC in Malaysia.
INTRODUCTION
Breast cancer (BC) is a major life-threatening global concern including Malaysia.[1,2,3,4,5] Increase incidence of BC is observed both in developed and developing countries.[6,7,8,9,10] Globally, BC is also the most common cause of cancer death, the most frequently diagnosed cancer, and now represents one in four of all cancers in women.[11] The incidence rates of BC in the developing countries are escalating because of increasing life expectancy, growing urbanization, particularly in younger women, and greater adoption of Western lifestyles.[12,13,14,15] Another study reported that “the increasing toll of BC in developing nations is really a devastating situation.”[16] The emergence of BC and subsequent complications of cancer tend to be more aggressive in young women compared to older population mainly due to lack of awareness and resulting in lower survival rates.[17,18,19,20,21] Therefore, early detection, accurate diagnosis, and self-awareness of BC are more crucial among young female for the treatment outcome.[20,21,22] The WHO stated, 7% of BC cases in Malaysia occur in women under the age of 35, 14% occur in women under 40%, and 28% in women under the age of 45. Forty-eight percent of the cases occur in women under the age of 50.[23] The majority of Malaysian does not go for screenings and perform breast self-examinations (BSEs) because of unawareness about a deadly issue of BC. There are a number of barriers, including psychological, social, and behavioral in relation to a mammogram in Malaysia.[24,25,26] The understanding of the causes, signs, and symptoms of BC is undeniably important to prevent BC.[27,28] A study reported that most of the women are aware that a lump in the breast or under the armpit is a symptom of BC, but they had less knowledge of nonlump symptoms.[29,30] Early detection of lumps can reduce the mortality and morbidity of BC.[31,32] Malaysian women present with a lump in the breast, usually painless, grow slowly and may alter the contour or size of the breast. Later, may have skin changes, an inverted nipple or blood stained nipple discharge. The lymph gland in the armpit will be swollen may be due to the proliferation of cancer cells.[33,34] The exact cause of BC is unknown and also not well understood.[35,36,37] Women with a family history of BC have an increased risk. The BRCA I and BRCA II gene carriers have at least 56–85% increased risk.[38,39] Other risk factors include exposure to radiation, a history of benign breast lumps, obesity, high fatty diet, early menarche, and late menopause.[40,41] Women with higher educational level are more likely to recognize earlier than others.[30,42] In general, most of the females have low knowledge on the risk factors of BC.[43,44,45] Early discovery of breast lumps through BSE is important for prevention and early detection of this disease. BSE is an easy screening and inexpensive method to detect BC.[46] Women will be more likely to find the breast lump themselves, but most of the women do not have sufficient knowledge of BSE.[47,48] Furthermore, most women have a lack of awareness to go for mammography excluding educated population.[21,49] One study revealed that most of the rural women with BC refused surgery because of fear of death.[49] Nearly all respondents opined that there are substantial benefits of mammograms and early detection, but there are practical barriers to conducting mammograms, especially financial constraint, even they were advised by a medical doctor.[49] Mammography above the age 50 years with or without clinical breast examination decreases both morbidity and mortality of BC, but women with a family history of BC, mammography suggested at the 40–49 age.[39,50,51] Mammography is advisable every 1–2 years, but below 35 years, the ultrasound scans of the breast may be helpful to detect early signs.[52] Low participations in screening programs have been attributed to many factors, including lack of knowledge. Therefore, many women miss early detection and treatment opportunities due to lack of knowledge, information, and awareness of BC, as well as cancer screening practices. Hopefully, the outcome of this study will help raise awareness among females and improve future research in BC. The purpose of this study was therefore to determine the knowledge, perception, and behavioral practice on BC screening and to find an association between sociodemographic data with knowledge and perception of BC and practice of BSE among female staff and students of University Kuala Lumpur, Royal College of Medicine Perak (UniKL RCMP), Perak, Malaysia.
MATERIALS AND METHODS
This was a cross-sectional, descriptive study to identify the level of awareness and practice about BC screening among the students and staff of UniKL RCMP, Malaysia. It was conducted on both the Campuses of UniKL RCMP, and the study period was from October 2015 to January 2016. All the female students and staff who agreed to participate and were available during the study period were included. Of the 800 students and staff, approximately 200 females were calculated as the sample size using the Epi Info 6.04d (January 2001, Centers for Disease Control and Prevention) application with the prevalence to the previous study. Targeted samples were informed about the study, and the consent was taken through the informed consent form. Study participants were distributed a questionnaire which was prepared and validated by an expert panel. Ethical approval was also obtained from the Ethics Committee of UniKL RCMP, Malaysia. Participants’ responses and information were kept strictly confidential, and the raw data were then collected and entered into the Microsoft Excel and was analyzed by using the SPSS version 21.0 (IBM Corporation, Armonk, NY).
RESULTS
Sociodemographic characteristics
A total of 203 participated in this study. The participants’ age range was 19–60 years, consisting of medical and pharmacy students and staff. Age was grouped as 19–20, 21–22, 23–24, and above 25, and their responses were 61.1% (124), 17.2% (35), 7.9% (16), and 13.8% (28), respectively. Nearly 43.8% (89) had known about BC screening, but the majority (56.2% (114)) respondents did not have any knowledge of BC screening. Eighty-nine respondents had previous knowledge on BC because their relatives (19.2% 39), friends (10.8% 22), neighbor (8.9% 18), and family members (8.4% 17) suffered from it. The educational background of the respondents was 71.9% (146) medical students, 13.3% (27) pharmacy students, 6.4% (13) diploma, 3% (6) masters, 2.5% (5) SPM, 2% (4) bachelors, and 1% (2) PhD, respectively. Almost all participants were Muslims 92.6% (188) and the rest were Hindus 3% (6), Christians 2.5% (5), Buddhists 1% (2), and others 1% (2). The ethnic distribution was 89.7% Malay, 4.5% (9) Indian, 1% (2) Chinese, and 4.9% (10) from other ethnic group, respectively. The marital status of the respondents was 85.7% (174) single and 14.3% (29) married, but none was widowed or divorced.
Knowledge of breast cancer
Twenty-three percent (47), 21% (43), 19% (39), 18% (36), 13% (26), and 6% (12) of the study respondents cited as a source of information about BC from the internet; pamphlets, book and etc.; television either documentaries or advertise; academic classes; relatives, friends, and lecturers; and radio, respectively. Nearly 34%, 27%, 13%, 12%, 10%, and 4% study respondents thought that genetic factors, exposure to carcinogens, exposure to X-rays, prolonged or early use of oral contraceptives, estrogen replacement therapy, and overweight, especially after menopause were the cause of BC. Nearly 54.18% (110), 52.21% (106), 42.36% (86), 42.36% (86), 40.39% (82), 27.09% (55), and 5.91% (12) of study respondents opined that excessive smoking, sedentary lifestyle, high junk food consumption, stress, excessive alcohol consumption, high animal fat diet, and prolonged use hair dyes, respectively, were the risk factors of BC. Respondents often reported multiple causes. Other than the risk factors mentioned, the race also was related to the occurrence of BC. White women were more likely to get BC compared to nonwhites. Other than that reduced levels of melatonin, which is related to sleeping patterns, are related to BC. About 100% of the participants believed that BSE is important to detect a breast lump in an early stage and can help to reduce morbidity and mortality. The majority (76.8% (156)) of study respondents knew about mammogram and its strength to detect BC. Thirty-five percent (71), 34% (69), 16% (33), 10% (20), and 5% (10) knew about the treatment options such as chemotherapy, surgery, radiotherapy, spiritually, and traditionally, respectively. Some respondents also know chemotherapy for BC is actually a combination of drugs that can be given by mouth and parenterally, chemotherapy shrinks the tumor prior to surgery, decrease the chances of recurrence following surgery, and to prevent metastasis. Nearly 84.73% (172), 52.71% (107), 51.23% (104), 36.95% (75), and 13.30% (27) of the study respondents believed that BC can be prevented by with regular BSE, control diet, regular exercise, breastfeeding, and vaccination, respectively. At many occasions, responders opted multiple options.
The correlation between sociodemographics and total knowledge scores
Age group and total knowledge scores
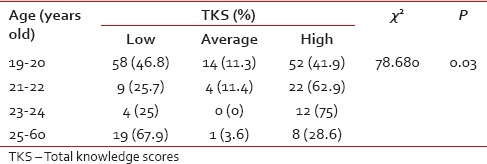
The was statistically (P = 0.03) significant correlation observed between four age groups 19–20, 21–22, 23–24, and 25–60 and total knowledge scores (TKS) [Table 1].
The was statistically (P = 0.03) significant correlation observed between four age groups 19–20, 21–22, 23–24, and 25–60 and total knowledge scores (TKS) [Table 1].
Table 1
Correlation between age and total knowledge scores stated by the study participants
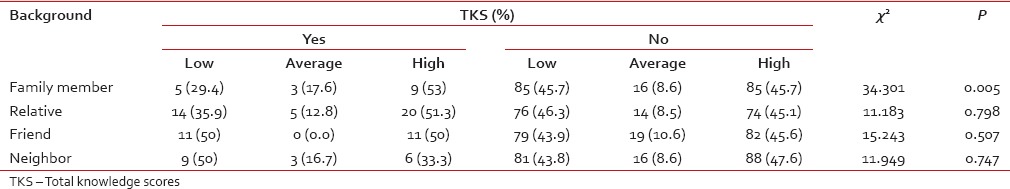
Background history of breast cancer and total knowledge scores
Table 2
Correlation between background history and total knowledge scores stated by the study participants
Educational qualifications and total knowledge scores
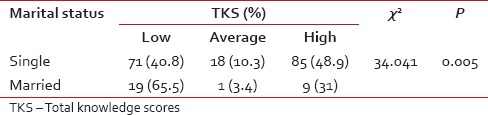
In addition, there was also statistically no significant (P = 0.055) correlation observed between educational qualification and TKS [Table 3]. Furthermore, there was also statistically no significant (P = 0.055) correlation observed between Religion and TKS (P = 0.727), Ethnicity and TKS (P = 0.117). Nevertheless, there was also statistically significant (P = 0.005) correlation observed between marital status and TKS [Table 4].
Table 3
Correlation between educational qualification and total knowledge scores stated by the study participants
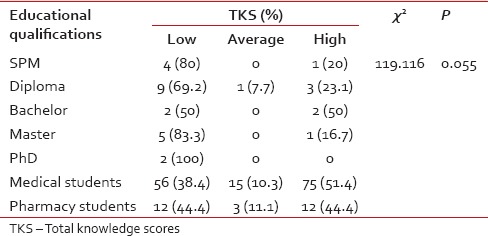
Table 4
Correlation between marital status and total knowledge scores stated by the study participants
Perception on breast cancer, breast self-examination, and mammogram
The majority of participants (77.3%) thought that mammogram screening is useful to keep updated on their health status. Approximately, 30% indicate that they preferred the examination to be done by a female physician and 15.8% thought the mammogram procedure is painful. Even though there were some respondents (3.0%) did not bother having a BC screening, almost all (91.1%) considered mammogram as a useful method to help detect any signs of BC at an early stage. The majority of respondents (71.9%) considered BC will cause them worried, but nearly half (52.7%) also gets depressed if they were to be diagnosed as such. About 51.7% have a thought that they have to continue life without giving up, and some of them (12.8%) felt embarrassed to tell their relatives and friends about the serious disease they are having. Most of the participants had a perception that BC cannot be cured easily.
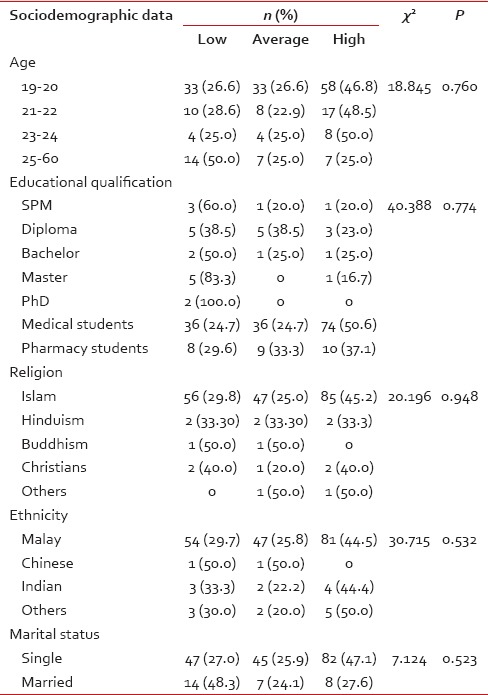
The correlation between sociodemographic and perception of breast cancer
The result of the study showed a relation between the sociodemographic factor and perceptions of BC, BSE, and mammogram [Table 5]. There was no statistically significant correlation found between age groups (P = 0.0760), educational qualifications (P = 0.774), religion (P = 0.948), ethnicity (P = 0.532), and marital status (P = 0.523) and perception about BC. By the same token, there was no statistically significant correlation between background history – family members (P = 0.499), relatives (P = 0.192), friends (P = 0.814), neighbor (P = 0.269), and perception of BC among the study participants.
The result of the study showed a relation between the sociodemographic factor and perceptions of BC, BSE, and mammogram [Table 5]. There was no statistically significant correlation found between age groups (P = 0.0760), educational qualifications (P = 0.774), religion (P = 0.948), ethnicity (P = 0.532), and marital status (P = 0.523) and perception about BC. By the same token, there was no statistically significant correlation between background history – family members (P = 0.499), relatives (P = 0.192), friends (P = 0.814), neighbor (P = 0.269), and perception of BC among the study participants.
Table 5
Correlation between sociodemographic and perception of breast cancer stated by the study participants
Practice on breast self-examination and mammogram
In the same way, there was no statistically significant (P > 0.05) correlation found between any of the sociodemographic and practice of BSE and mammogram. Correspondingly, there was no statistically significant (P > 0.05) correlation found between background history and practice on BSE and mammogram among the study participants.
DISCUSSION
The current study found that there were 43.8% of participants who had a family history of BC. The top risk factors chosen by participants were excessive smoking, sedentary lifestyle, high junk food consumption, stress, high alcohol consumption, high animal fat diet, and prolonged use of dark hair dye. The majority participants were aware of genetic linkage of BC. A very small group of participants were not aware that overweight and postmenopausal age may be causes of BC. Early discovery of breast lumps through BSE is important for prevention and early detection of this disease. BSE is an easy screening method which cost nothing and absolutely privacy maintained.[10,20,21,49] In the previous studies, most of the women did not have sufficient knowledge of BSE.[10,20,21,49] Our study found out that most of the participants knew that BSE is important for early detection of a breast lump. Although the majority study participants know how to perform BSE, but just over one-sixth to one-third of them does BSE 1–3 times per year.
Furthermore, most women had a lack of awareness to go for mammography with the exception of an educated community.[10,20,21,49] Although the majority of the study of participants knew about mammogram and its utility to detect BC very early and maintain their health but did not do because they have not passed on tertiary care hospital as they were mainly belonging 20–24 ages. A small group has a misconception regarding mammogram is painful, and almost one-third demanded the test should be conducted by female doctors. This can be explained as the study population was not much aware of the procedure, mainly Muslims have a conservative attitude. The majority participants were aware of BC treatment options like surgery and chemotherapy; these findings were similar to a number studies.[10,20,21,49] The greater part of participants thought that BC was not easily cured, but a minor portion thought that it was easily cured. The study participants also described that they will feel depressed, life must go on, and embarrassed if diagnosed as BC. Television and newspapers were cited as the most important sources of information regarding BC.[10,20,21,49] In our study, the internet was the most preferable source and the least choice was a radio. Women with a high awareness of BC opted for breast examination biannually by the physician and those with poor awareness did not think that breast examination is the screening approach.[10,20,21,49] The participants, by and large, thought that performing BSE is the preventive method for BC. They also gave their opinions on increasing publicity through mass media and campaign. The participants were being asked whether they are interested to attend BC awareness campaign and most of them agreed.
Limitation of study
The difficulties of coping with the timetable of the clinical year students since they were having bedside teaching in the hospital. Therefore, certain participants did not answer the questionnaire as expected and caused an interruption in our study.
CONCLUSIONS
The majority of study participants had good knowledge of BC and usually perform BSE. Only a few of them went for mammography because it is recommended only who are above 50 years, but most of the study participants were much younger. Participants were aware of causes, risk factors, treatments, and preventive methods, even though they have no family history of BC. Most of them were interested to join awareness campaign. Knowledge of the participants was adequate, but the level of practice was low. Therefore, a wider multicenter study is advocated to prevent and early diagnosis of BC.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Authors are much grateful to all the study populations for their time and energy. Furthermore, the authors want to pass their heartfelt gratitude to the Dean of UniKL-RCMP, Malaysia, for his kindest cooperation.


 PDF
PDF  Views
Views  Share
Share

