Classical or pylorus-preserving pancreatoduodenectomy in pancreatic and periampullary cancer: “The jury is still out!”
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(04): 209-210
DOI: DOI: 10.4103/0971-5851.195747
Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
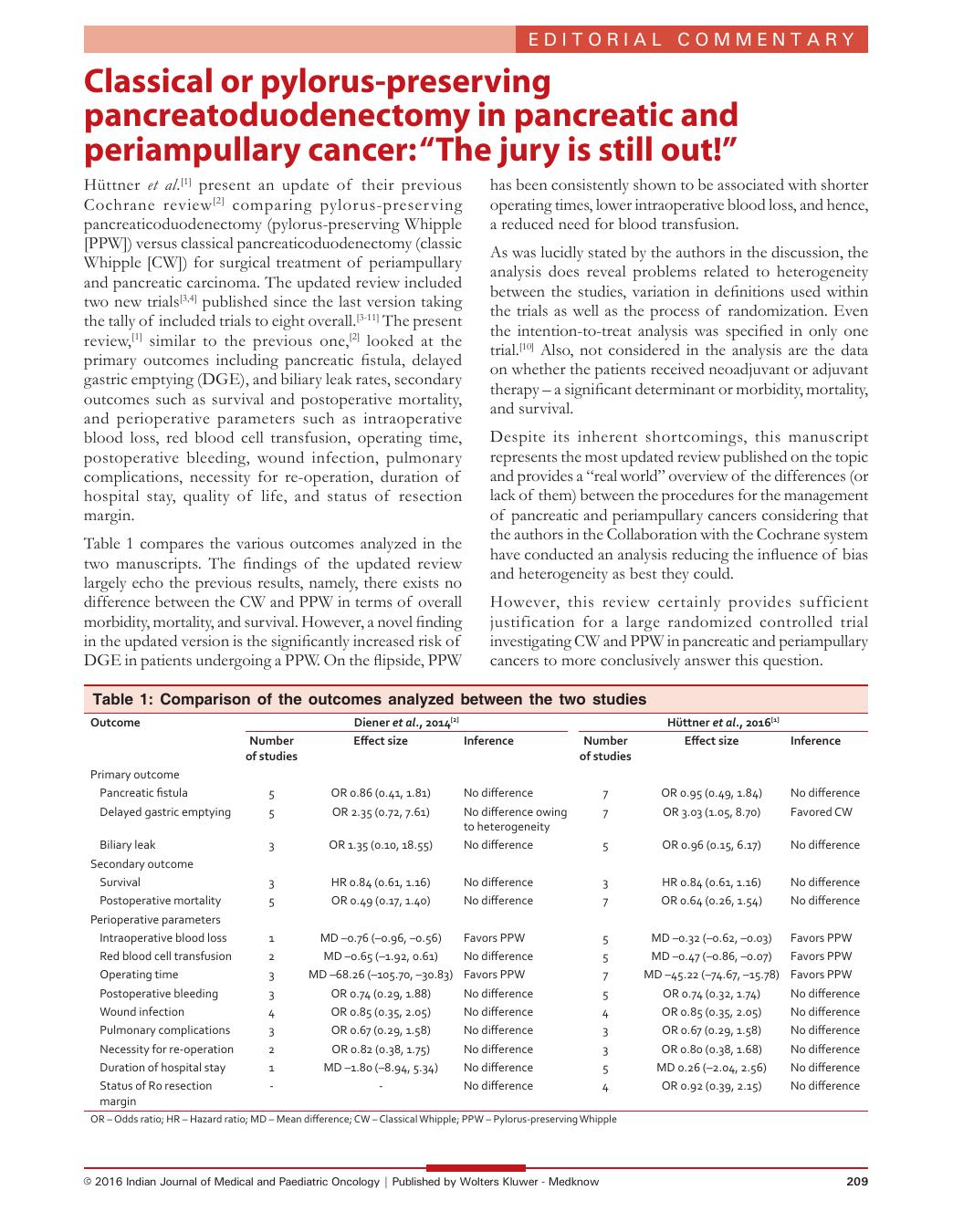
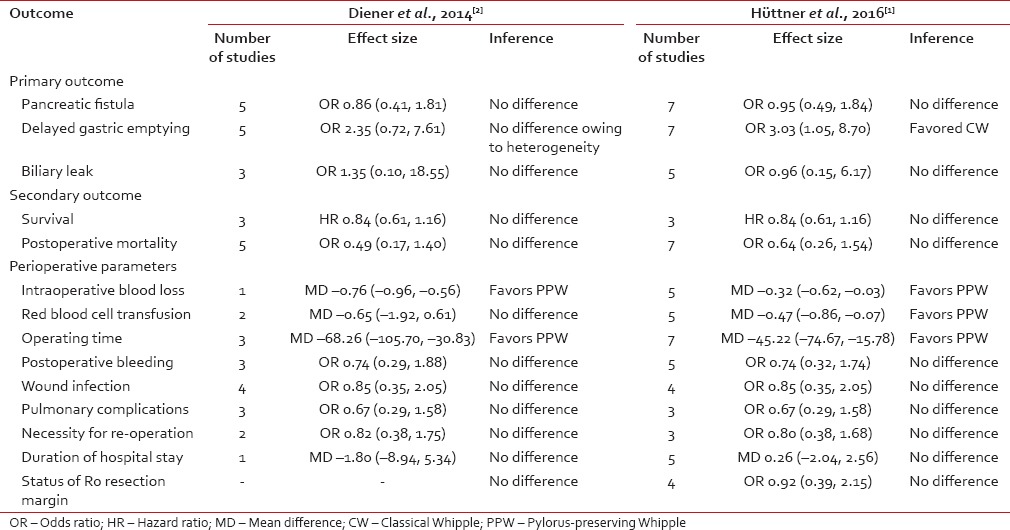
Hüttner et al.[1] present an update of their previous Cochrane review[2] comparing pylorus-preserving pancreaticoduodenectomy (pylorus-preserving Whipple [PPW]) versus classical pancreaticoduodenectomy (classic Whipple [CW]) for surgical treatment of periampullary and pancreatic carcinoma. The updated review included two new trials[3,4] published since the last version taking the tally of included trials to eight overall.[3,4,5,6,7,8,9,10,11] The present review,[1] similar to the previous one,[2] looked at the primary outcomes including pancreatic fistula, delayed gastric emptying (DGE), and biliary leak rates, secondary outcomes such as survival and postoperative mortality, and perioperative parameters such as intraoperative blood loss, red blood cell transfusion, operating time, postoperative bleeding, wound infection, pulmonary complications, necessity for re-operation, duration of hospital stay, quality of life, and status of resection margin.
Table 1 compares the various outcomes analyzed in the two manuscripts. The findings of the updated review largely echo the previous results, namely, there exists no difference between the CW and PPW in terms of overall morbidity, mortality, and survival. However, a novel finding in the updated version is the significantly increased risk of DGE in patients undergoing a PPW. On the flipside, PPW has been consistently shown to be associated with shorter operating times, lower intraoperative blood loss, and hence, a reduced need for blood transfusion.
Table 1
Comparison of the outcomes analyzed between the two studies
 As was lucidly stated by the authors in the discussion, the analysis does reveal problems related to heterogeneity between the studies, variation in definitions used within the trials as well as the process of randomization. Even the intention-to-treat analysis was specified in only one trial.[10] Also, not considered in the analysis are the data on whether the patients received neoadjuvant or adjuvant therapy – a significant determinant or morbidity, mortality, and survival.
As was lucidly stated by the authors in the discussion, the analysis does reveal problems related to heterogeneity between the studies, variation in definitions used within the trials as well as the process of randomization. Even the intention-to-treat analysis was specified in only one trial.[10] Also, not considered in the analysis are the data on whether the patients received neoadjuvant or adjuvant therapy – a significant determinant or morbidity, mortality, and survival.Despite its inherent shortcomings, this manuscript represents the most updated review published on the topic and provides a “real world” overview of the differences (or lack of them) between the procedures for the management of pancreatic and periampullary cancers considering that the authors in the Collaboration with the Cochrane system have conducted an analysis reducing the influence of bias and heterogeneity as best they could.
However, this review certainly provides sufficient justification for a large randomized controlled trial investigating CW and PPW in pancreatic and periampullary cancers to more conclusively answer this question.

 PDF
PDF  Views
Views  Share
Share

