Classical Hodgkin Lymphoma Presenting as Cutaneous and Soft Tissue Mass Lesion: An Enigmatic Presentation Posing a Diagnostic Challenge—A Case Report and Review of Literature
CC BY 4.0 · Indian J Med Paediatr Oncol 2024; 45(06): 538-541
DOI: DOI: 10.1055/s-0041-1740441
Abstract
Hodgkin lymphoma (HL) is primarily a nodal disease. Cutaneous involvement of HL as a presenting feature is extremely rare. Skin involvement is usually seen as a metachronous involvement in the course of disease and is associated with poor prognosis. Primary skin and soft tissue involvement can be construed as nonhematological, inflammatory, or infective etiology. We report a 14-year-old girl with fever, weight loss, lymphadenopathy, and multiple papular lesions over the right chest wall as initial manifestation of HL, posing a diagnostic challenge. In view of stage IVBE, patient was managed with intensive chemotherapy regimen and is currently free of disease at 6 months of follow-up.
Keywords
cutaneous - extranodal - Hodgkin lymphomaDeclaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
Publication History
Article published online:
03 February 2022
© 2022. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Cutaneous Hodgkin’s lymphomaAsawari Anant Ambekar, South Asian Journal of Cancer, 2017
- Primary Hodgkin Lymphoma: A Rare Manifestation in the Hard PalateIury Lima Veloso, International Archives of Otorhinolaryngology, 2014
- Chest Wall Mass as the Dominant Presentation of Low-Grade B-Cell Non-Hodgkin's Lymphoma: A Case ReportSunita Nitin Sonavane, VCOT Open, 2022
- Chest Wall Mass as the Dominant Presentation of Low-Grade B-Cell Non-Hodgkin's Lymphoma: A Case ReportSunita Nitin Sonavane, World Journal of Nuclear Medicine, 2022
- Positron emission tomography-computed tomography in subcutaneous panniculitis-like T-cell lymphomaPrathyusha Bikkina, World Journal of Nuclear Medicine, 2019
- Primary cutaneous Hodgkin’s lymphomaM. Mukesh, Clinical and Experimental Dermatology, 2009
- Primary lymphoblastic non‐Hodgkin's lymphoma of the skinR. WILLEMZE, British Journal of Dermatology, 1981
- Cutaneous Lymphoma Complicating Basal Cell Carcinoma of the FaceRobert G. Chambers, JAMA Otolaryngology Head Neck Surgery, 1970
- Cutaneous Hodgkin's DiseaseCraig L. Silverman, JAMA Dermatology, 1982
- Cutaneous Granulomas in Malignant LymphomaHenry W. Randle, JAMA Dermatology, 1980
Abstract
Hodgkin lymphoma (HL) is primarily a nodal disease. Cutaneous involvement of HL as a presenting feature is extremely rare. Skin involvement is usually seen as a metachronous involvement in the course of disease and is associated with poor prognosis. Primary skin and soft tissue involvement can be construed as nonhematological, inflammatory, or infective etiology. We report a 14-year-old girl with fever, weight loss, lymphadenopathy, and multiple papular lesions over the right chest wall as initial manifestation of HL, posing a diagnostic challenge. In view of stage IVBE, patient was managed with intensive chemotherapy regimen and is currently free of disease at 6 months of follow-up.
Keywords
cutaneous - extranodal - Hodgkin lymphomaIntroduction
Hodgkin lymphoma (HL), previously known as Hodgkin disease, is a monoclonal lymphoid neoplasm, originating most often from B lymphocytes. It is characterized by the orderly spread of disease from one lymph node group to another and usually begins in lymph nodes.[1] Extranodal invasion of adjacent tissue is observed in up to 15%-of cases.[2] Cutaneous involvement of HL as a presenting feature is extremely rare. Skin involvement is usually seen as a metachronous involvement in the course of disease and is associated with poor prognosis. We report here an interesting case of HL in a 14-year-old girl, with fever and lymphadenopathy associated with skin and soft tissue involvement as initial manifestation of HL, which posed a diagnostic challenge. Informed consent was obtained from the parents.
Case Report
A 14-year-old female presented with history of intermittent fever, weight loss, and progressively increasing bilateral neck masses over a period of 6 months. She also reported skin lesions over the right chest wall for 3 months and cough associated with breathlessness for about a month. There were no bone pains or symptoms suggestive of aerodigestive tract involvement.
Examination findings revealed the patient to be thin built, anxious, with pallor and mild respiratory distress, bilateral firm, nontender cervical (level 2–4), supraclavicular and axillary lymphadenopathy. The large conglomerate of fused right cervical nodes measured 7x4cm. There were multiple papules and nodules present over entire right half of chest wall involving breast, infra-axillary, and scapular regions and extending to right shoulder and neck, few lesions were ulcerative with purulent discharge ([Fig. 1]). Systemic examination revealed reduced air entry over right chest.

| Fig 1Multiple papulonodular lesions over right breast and axilla; few lesions show ulceration and purulent discharge.
She was initially investigated elsewhere and in view of generalized lymphadenopathy and right-sided pleural effusion, she was clinicoradiologically diagnosed as pulmonary tuberculosis and had received 5 months of antitubercular therapy. Her skin lesions were suspected as herpes zoster infection and treated with acyclovir. She was unresponsive to both of the therapies, instead the lymph node mass and skin lesions progressed, for which patient was referred to our institute for further management.
At our institute, patient was investigated and initial complete blood counts, erythrocyte sedimentation rate (24 mm), liver and renal function tests were normal. Biopsy from the cutaneous lesion revealed unremarkable epidermis with underlying dermis showing infiltrate of polymorphous population of lymphocytes, histiocytes, and eosinophils. Numerous interspersed large neoplastic cells were seen monolobated to polylobated nuclei having vesicular chromatin and prominent nucleoli ([Figs. 2A] and [B] ). On subsequent immunohistochemical staining, the large scattered neoplastic cells were positive for CD30, PAX-5 (heterogenous; [Figs. 2C] and [D] ) while negative for CD20, LCA, CD3, CD15, BCL-6, and EBER-ISH. Overall histopathological features were conclusive of classical HL, nodular sclerosis. The concurrent biopsy from lymph node also revealed HL involvement. Staging investigations revealed the bone marrow (aspirate and biopsy) to be uninvolved by HL, while positron emission tomography computed tomography (PET-CT) scan ([Fig. 3]) showed metabolically active multiple bilateral cervical, supraclavicular, subpectoral, axillary, internal mammary, paratracheal, retrocrural, aortocaval, and para-aortic adenopathy, with extranodal disease involving bone (osteodestructive lesion involving head and shaft of right humerus), soft tissue deposits (right chest wall and right upper arm), right pleural deposits, and right pleural effusion with collapse, hence conforming to stage IVBE. The cross-sectional images reveal that the involvement was contiguous.
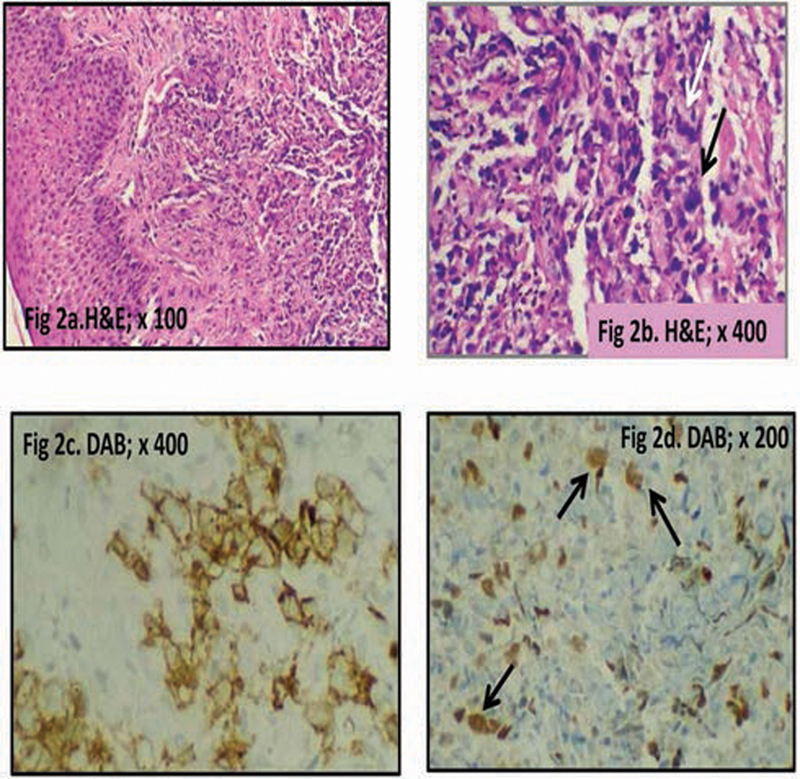
| Fig 2 (A) Section from skin lesion shows unremarkable epidermis with underlying atypical lymphoid infiltrate in dermis. (B) Numerous scattered large neoplastic cells (arrow) with multilobated convoluted nuclei (Reed-Sternberg [RS] cells) seen amid lymphoid infiltrate. (C) The scattered RS cells show strong membranous positivity for CD30. (D) The scattered RS cells (arrow) are also positive for PAX-5. DAB, diaminobenzidine; H&;E, hematoxylin and eosin.
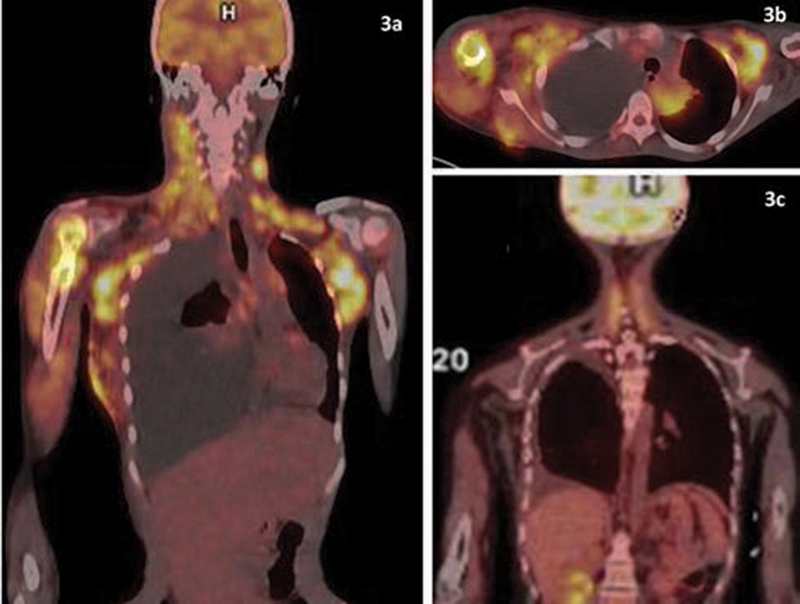
| Fig 3 (A) Whole body positron emission tomography computed tomography scan. Pretreatment image showing metabolically active supradiaphragmatic lymphadenopathy with bone (right humerus), soft tissue (right chest wall), right pleural tissue deposits, and right pleural effusion. (B) Pretreatment cross-sectional image shows contiguous involvement. (C) Posttreatment image (after 4 cycles) reveals complete metabolic response.
Subsequently, the patient was started on Adriamycin, bleomycin, vinblastine, dacarbazine chemotherapy protocol. However, disease progressed and after one cycle she was put on escalated bleomycin, etoposide, Adriamycin, cyclophosphamide, vincristine, procarbazine and prednisolone chemotherapy. Subsequent evaluation with PET-CT showed partial response (50–60%) after two cycles and complete response (including skin, except for residual pleural effusion) after four cycles ([Fig. 3C]). Hence, further consolidation with high-dose chemotherapy followed by autologous peripheral blood stem cell rescue was undertaken. After the completion of treatment, the patient is free of disease at 6 months of follow-up.
Discussion
HL is primarily a nodal disease and pattern of spread is usually contiguous, spreading from one LN (lymph nodal) region to the next along the lymphatic system. Extranodal invasion of adjacent tissue is observed in up to 15%-of cases, while hematogenous spread is seen in 5 to 10%-of cases.[2] We have described an interesting case of HL with multiple extranodal sites of disease with significant involvement of skin and soft tissue.
Cutaneous involvement of HL is extremely rare occurring in 0.5 to 3.4%-of cases and is more frequently reported in non-HL.[3] [4] Although first reported in 1904 by Grosz et al, less than a hundred cases have been reported in literature, and this is the youngest case reported to the best of the author's knowledge ([Table 1]).[3] [4] [5] [6] [7] [8] [9] [10] Various types of skin lesions have been reported; these may be nonspecific findings due to paraneoplastic syndrome or vasculitis, like pruritis, urticaria, hyperpigmentation, or ichthyosis, or due to infiltration of skin by disease.[5] [6] The latter may present as nodules, papules, plaques, ulcers, and/or erythroderma, most of which we observed in the present case with biopsy proof of tumor infiltration.[7] [8]
Author (y) | No | Age (y) | Gender | Symptoms (No) | Duration (mo) | Stage | Treatment | Response (No) |
|---|---|---|---|---|---|---|---|---|
White and Patterson (1985)8 | 16 | 16–63 | Male (9) Female (7) | Lesion on Chest (11) Neck (3) Scalp (2) | 32.1 (mean) | IV (7) III (4) II (5) | Multiple regimens | Death due to disease (11) Death due to unrelated cause (1) Lost to follow-up (4) |
Jurisić et al (2005)9 | 1 | 77 | Female | Nodule arms and abdomen | 6 | II B | CVPP | No complete resolution |
Rubenstein and Duvic (2006)5 | 3 | Male (1) Female (2) | Nodule over chest (n=2) Rash on trunk (n=1) | – | – | – | – | |
Isao et al (2007)4 | 1 | 44 | Male | Nodule on back | 32 | IV B | Multiple regimens | Died |
Dhull et al (2012)7 | 1 | 22 | Female | Fungating mass over mid-chest | 24 | IV B | ABVD | Disease free |
Khawandanah et al (2014)6 | 1 | 46 | Male | Rash on chest and neck | 3 | IV E | AVD/Bend/GCD | Disease free 8 mo |
Goyal et al (2014)3 | 4 | 50 21 25 28 | Female Male Female Male | Nodules over neck Ulcer over sternum Nodule on breast Rash arms and legs | 1 6 12 4 | IV B IV B IV B IV B | ABVD-RT ABVD-RT ABVD ABVD | Disease free 3 y Recurrence in 6 mo Disease free Disease free 2.5 y |
References
- Marafioti T, Hummel M, Foss HD. et al. Hodgkin and Reed-Sternberg cells represent an expansion of a single clone originating from a germinal center B-cell with functional immunoglobulin gene rearrangements but defective immunoglobulin transcription. Blood 2000; 95 (04) 1443-1450
- Guermazi A, Brice P, de Kerviler EE. et al. Extranodal Hodgkin disease: spectrum of disease. Radiographics 2001; 21 (01) 161-179
- Goyal S, Biswas A, Puri T, Gupta R, Muzumder S, Julka PK. Different faces of cutaneous Hodgkin's disease. Indian J Dermatopathol Diagn Dermatol 2014; 1: 79
- Isao M, Masanori D, Masatoshi F, Hirokuni T. Cutaneous involvement in Hodgkin's disease. Int Med J Stage 2007; 46: 73-74
- Rubenstein M, Duvic M. Cutaneous manifestations of Hodgkin's disease. Int J Dermatol 2006; 45 (03) 251-256
- Khawandanah M, Kraus T, Cherry M. Refractory classical Hodgkin lymphoma presenting with atypical cutaneous involvement and diagnosis of ZZ phenotype alpha-1 antitrypsin deficiency. Case Rep Hematol 2014; 2014: 642868
- Dhull AK, Soni A, Kaushal V. Hodgkin's lymphoma with cutaneous involvement. BMJ Case Rep 2012; 2012: bcr2012007599
- White RM, Patterson JW. Cutaneous involvement in Hodgkin's disease. Cancer 1985; 55 (05) 1136-1145
- Jurisić V, Bogunović M, Colovic N, Colović M. Indolent course of the cutaneous Hodgkin's disease. J Cutan Pathol 2005; 32 (02) 176-178
- Howlader N, Noon AM, Krapcho M. et al. Eds. SEER Cancer Statistics Review, 1975–2017. National Cancer Institute; Bethesda, https://seer.cancer.gov/csr/1975_2017 MD Accessed July 10, 2021
Address for correspondence
Publication History
Article published online:
03 February 2022
© 2022. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Cutaneous Hodgkin’s lymphomaAsawari Anant Ambekar, South Asian Journal of Cancer, 2017
- Primary Hodgkin Lymphoma: A Rare Manifestation in the Hard PalateIury Lima Veloso, International Archives of Otorhinolaryngology, 2014
- Chest Wall Mass as the Dominant Presentation of Low-Grade B-Cell Non-Hodgkin's Lymphoma: A Case ReportSunita Nitin Sonavane, VCOT Open, 2022
- Chest Wall Mass as the Dominant Presentation of Low-Grade B-Cell Non-Hodgkin's Lymphoma: A Case ReportSunita Nitin Sonavane, World Journal of Nuclear Medicine, 2022
- Positron emission tomography-computed tomography in subcutaneous panniculitis-like T-cell lymphomaPrathyusha Bikkina, World Journal of Nuclear Medicine, 2019
- Hodgkin's lymphoma. II: Treatment and delayed morbidity.P. Carde, The BMJ, 1992
- Non-Hodgkin's lymphoma. I: Characterisation and treatment.Sean O’Reilly, et al., The BMJ, 1992
- Modern management of non-Hodgkin's lymphoma.G M Mead, The BMJ, 1986
- Cutaneous Manifestations and Treatment Advances of Adult T-Cell Leukemia/LymphomaInternational Journal of Dermatology and Venereology
- Change at last at WHOFiona Godlee, The BMJ, 1998

| Fig 1Multiple papulonodular lesions over right breast and axilla; few lesions show ulceration and purulent discharge.
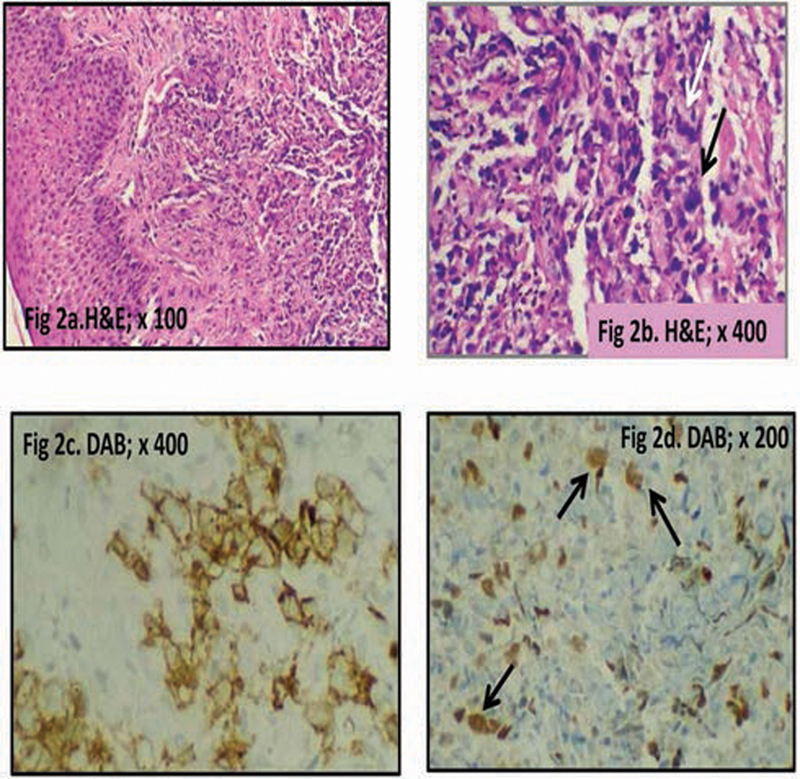
| Fig 2 (A) Section from skin lesion shows unremarkable epidermis with underlying atypical lymphoid infiltrate in dermis. (B) Numerous scattered large neoplastic cells (arrow) with multilobated convoluted nuclei (Reed-Sternberg [RS] cells) seen amid lymphoid infiltrate. (C) The scattered RS cells show strong membranous positivity for CD30. (D) The scattered RS cells (arrow) are also positive for PAX-5. DAB, diaminobenzidine; H&;E, hematoxylin and eosin.
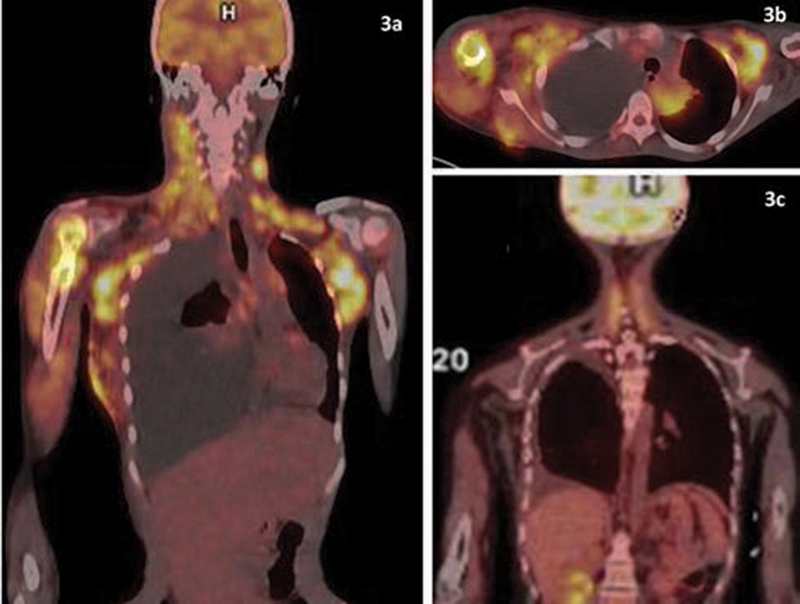
| Fig 3 (A) Whole body positron emission tomography computed tomography scan. Pretreatment image showing metabolically active supradiaphragmatic lymphadenopathy with bone (right humerus), soft tissue (right chest wall), right pleural tissue deposits, and right pleural effusion. (B) Pretreatment cross-sectional image shows contiguous involvement. (C) Posttreatment image (after 4 cycles) reveals complete metabolic response.
References
- Marafioti T, Hummel M, Foss HD. et al. Hodgkin and Reed-Sternberg cells represent an expansion of a single clone originating from a germinal center B-cell with functional immunoglobulin gene rearrangements but defective immunoglobulin transcription. Blood 2000; 95 (04) 1443-1450
- Guermazi A, Brice P, de Kerviler EE. et al. Extranodal Hodgkin disease: spectrum of disease. Radiographics 2001; 21 (01) 161-179
- Goyal S, Biswas A, Puri T, Gupta R, Muzumder S, Julka PK. Different faces of cutaneous Hodgkin's disease. Indian J Dermatopathol Diagn Dermatol 2014; 1: 79
- Isao M, Masanori D, Masatoshi F, Hirokuni T. Cutaneous involvement in Hodgkin's disease. Int Med J Stage 2007; 46: 73-74
- Rubenstein M, Duvic M. Cutaneous manifestations of Hodgkin's disease. Int J Dermatol 2006; 45 (03) 251-256
- Khawandanah M, Kraus T, Cherry M. Refractory classical Hodgkin lymphoma presenting with atypical cutaneous involvement and diagnosis of ZZ phenotype alpha-1 antitrypsin deficiency. Case Rep Hematol 2014; 2014: 642868
- Dhull AK, Soni A, Kaushal V. Hodgkin's lymphoma with cutaneous involvement. BMJ Case Rep 2012; 2012: bcr2012007599
- White RM, Patterson JW. Cutaneous involvement in Hodgkin's disease. Cancer 1985; 55 (05) 1136-1145
- Jurisić V, Bogunović M, Colovic N, Colović M. Indolent course of the cutaneous Hodgkin's disease. J Cutan Pathol 2005; 32 (02) 176-178
- Howlader N, Noon AM, Krapcho M. et al. Eds. SEER Cancer Statistics Review, 1975–2017. National Cancer Institute; Bethesda, https://seer.cancer.gov/csr/1975_2017 MD Accessed July 10, 2021


 PDF
PDF  Views
Views  Share
Share

