Child's Understanding of Cancer when Faced with Advancing Disease: A Retrospective Chart Review
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2022; 43(03): 262-269
DOI: DOI: 10.1055/s-0042-1750208
Abstract
Introduction It is difficult to comprehend a child's understanding of disease-related information as they might be unwilling to talk or feel inhibited about raising their concerns. Understanding children's perception is important to facilitate better communication in palliative care.
Objectives To study child's understanding of advancing disease when referred to the Pediatric Palliative Care Services.
Materials and Methods A retrospective chart review of 34 case record forms from March 2019 to March 2020 was conducted after obtaining a waiver of consent and Institutional Ethics Committee approval. The inclusion criteria were children having advanced cancer referred for palliative care, incomplete records were excluded. Data were analyzed using thematic analysis.
Results Twenty-three were male, and 11 were female children, the mean age was 12 years. Five major themes were identified—the child's understanding of disease diagnosis and prognosis, nature of communication between parents and the child, barriers to communication, child's means of support, and interventions used during counseling.
Conclusion Communication between children suffering from advanced cancer and their parents/caregivers is a sensitive issue, and noncommunication is often due to mutual effort to shield each other from the stress of difficult conversations. Lack of communication contributes to poor coping and forces children to seek comfort in other sources leaving parents distressed. Psychological interventions like resource building and psychoeducation are effective.
Keywords
cancer - palliative care - pediatrics - thematic analysis - qualitative research - chart reviewPublication History
Article published online:
02 July 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Introduction It is difficult to comprehend a child's understanding of disease-related information as they might be unwilling to talk or feel inhibited about raising their concerns. Understanding children's perception is important to facilitate better communication in palliative care.
Objectives To study child's understanding of advancing disease when referred to the Pediatric Palliative Care Services.
Materials and Methods A retrospective chart review of 34 case record forms from March 2019 to March 2020 was conducted after obtaining a waiver of consent and Institutional Ethics Committee approval. The inclusion criteria were children having advanced cancer referred for palliative care, incomplete records were excluded. Data were analyzed using thematic analysis.
Results Twenty-three were male, and 11 were female children, the mean age was 12 years. Five major themes were identified—the child's understanding of disease diagnosis and prognosis, nature of communication between parents and the child, barriers to communication, child's means of support, and interventions used during counseling.
Conclusion Communication between children suffering from advanced cancer and their parents/caregivers is a sensitive issue, and noncommunication is often due to mutual effort to shield each other from the stress of difficult conversations. Lack of communication contributes to poor coping and forces children to seek comfort in other sources leaving parents distressed. Psychological interventions like resource building and psychoeducation are effective.
Keywords
cancer - palliative care - pediatrics - thematic analysis - qualitative research - chart reviewIntroduction
Most parents would like their child's prognosis to be explained to them, however difficult it could be for them to accept.[1] Sometimes it is the oncologist who is not ready for the discussion.[2] When the prognosis turns adverse due to relapse or resistant disease, a palliative care referral can help parents to cope.[3] Routinely in a pediatric palliative care clinic, communication channels are opened for discussion of prognosis. Keim et al have shown that open communication with parents (especially mothers) helped them to cope with advanced cancer at the end of 1 year.[4]
At the department of palliative medicine, pediatric palliative has been offered to children and their families since 2002. Routinely, the cases are discussed in a tumor board/multidisciplinary clinic, and children with resistant disease or relapse are referred for palliative care. At this clinic, the child is “counseled” separately. With the help of toys, stories, and other diversion methods, the counseling psychologist, along with a trained child life counselor comprehends the concept of what the child understands about the disease and how he/she is coping. These observations are conveyed to the psychologist and doctor who are counseling parents separately. If necessary, they are also communicated to the parents, to aid in communication between the child and parents. All of these are documented routinely in the case record form and this workflow has been described in an earlier paper.[5]
It has been observed that many children, aged 6 years and above, have some understanding of the disease and their condition based on their self-reporting about disease-related questions.[6] This may give rise to related queries and concerns, but in most cases, children do not feel comfortable speaking about this with physicians or parents. Sometimes it is the parents who can be a barrier to effective communication, as they might favor collusion to protect their child from bad news.[7] A major shift in children's understanding of key biological concepts about the structure and function of the human body and disease transmission takes place between the ages of 7 and 11 years.[8] Yet, parents may have their own set of reservations and beliefs against communicating with a child, regarding a child's disease and its progression. Parents' decisions not to talk to their children might also reflect their emotional distress and a desire to protect themselves from the “unbearable reality of the situation.”[9]
Like adults, facing challenges against a serious illness like cancer can provoke thoughts of death and dying in children as well; but there can be unique ways in which children cope, and it is worthwhile to provide a supportive framework for such kids to express themselves. Studies have found out that a child might learn about their disease and how serious it is without being explicitly told.[10] Children might be unwilling to talk, or feel inhibited about raising their concerns, particularly if they are aware of their parents' anxiety and discomfort around the subject.[11] Also, a child's perception of the disease can give a deeper insight into their disease burden. According to Rutishauser, understanding this burden of illness can help in forming the basis for negotiating age-appropriate therapeutic goals and strategies.[12] Also, communication between the child, their parents or caregivers, and health care professionals helps to gain the trust of the child and is associated with enhanced adherence through improved understanding of illness and the importance of treatment.[13]
There is inadequate information in the literature on how the child perceives a referral to the palliative care services amid advancing disease. This retrospective chart review was planned to understand this lacuna and will help the pediatric palliative care team plan future strategies in bridging any communication gaps between the child with cancer and the parents.
This project aimed to record a child's understanding of cancer and its prognosis, and the psychosocial methods employed.
Objectives
The primary objective is to study the child's understanding of advancing disease when referred to the pediatric palliative care services. Second, to assess how much of a communication gap exists between the child and parents and also to understand psychosocial strategies used to overcome any such barrier.
Materials and Methods
Sample and Setting
At the Department of Palliative Medicine, Tata Memorial Centre, Mumbai, Maharashtra, India, pediatric palliative has been offered to children and their families since 2002. The cases are discussed before a multidisciplinary team meeting in pediatric oncology and children with a resistant disease or relapse are referred for palliative care. Every child who is referred to the pediatric palliative care service is seen separately by a counseling psychologist and/or a trained child life counselor. Their evaluation is recorded in the Case Record Form. The notes which are compiled for every interview were retrospectively analyzed to look for:
-
The child's understanding of his/her disease, prognosis, related concerns, and the psychosocial interventions offered in aiding these concerns.
-
Communication between parents and child regarding disease and prognosis and barriers to it.
-
Any other sources of help obtained.
Inclusion Criteria
Every chart where the child and parents were counseled separately at referral to the Department of Palliative Medicine, Pediatric Unit between March 2019 and March 2020.
Age range was between 6 and 18 years.
Exclusion Criteria
Any incomplete case records, that is, a medical record that fails to tell the patient's whole story, and lacks clarity, specificity, or completeness.
Data Collection and Procedure
The primary outcome measure was to record the child's understanding of cancer and its prognosis, while the secondary outcome was to record the psychosocial methods employed. We recorded demographic and clinical data from the patient charts. The data were summarized by descriptive statistics. Counseling notes were analyzed for emerging themes. We could screen through 50 participants from case records. The final sample size was determined by thematic saturation, the point at which new data appears to no longer contribute to the findings due to the repetition of themes and comments by participants.[14] At this point, data generation was terminated.
The information in the study records/audio records was kept confidential and the clinical charts are housed in the Tata Memorial Hospital Clinical Research Secretariat in safe custody, made available only to persons conducting the study and to the regulatory authorities. No reference has been made in oral or written reports which could link the participant to the study. No extra funding was needed for this chart review.
Workflow Process
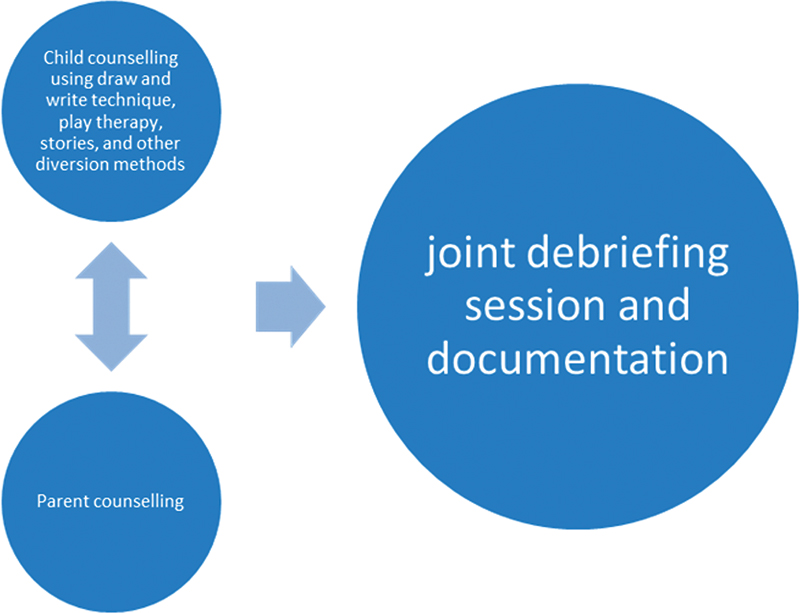
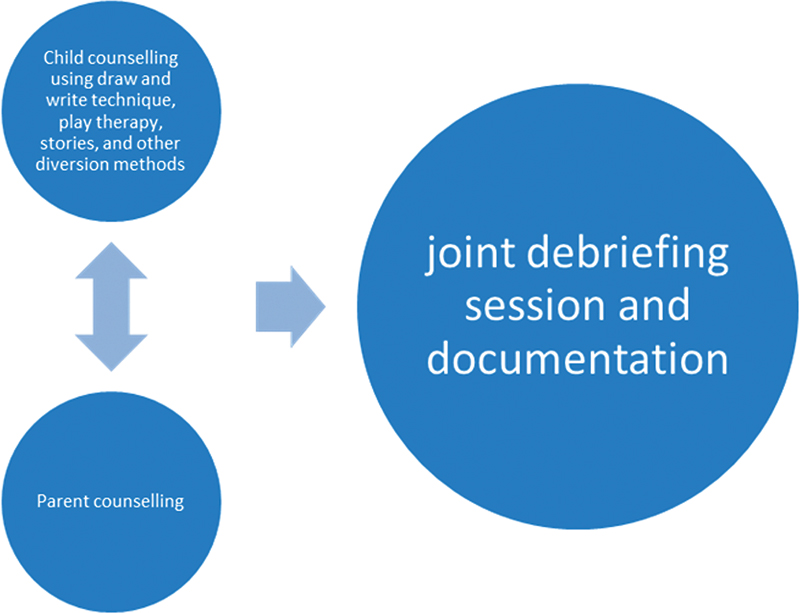
In a palliative care clinic, the child is “counseled” separately from the parent with their permission. Child counseling often involves communicating with children using the draw and write technique, and play therapy with toys, stories, and other diversion methods; duly backed by evidence from the literature.[15] [16] [17] [18] The draw and write technique[15] and play therapy[17] are jovial methods of engaging with children,[18] where they draw/write about their thoughts about cancer, and about things which help them to cope. In this activity, children are encouraged to work individually but have the option to clarify doubts with the child psychologist/researcher if they want to. Following this activity, the psychologist has a joint session with the children and their parents for any clarifications. These observations are conveyed to the psychologist and doctor who counsel parents separately. A final debriefing session involves all coming together at the end of the consultation. Everything is documented in the case record form in the English language. Parents are given contact details from the clinic for office/out-of-office hours communication and are scheduled for a follow-up visit.
|
Data Analysis
Techniques of thematic content analysis were followed by two different researchers to develop an initial list of codes.[19] [20] First, an initial list of codes was generated from the transcripts, followed by discussions to have an agreement on the set of codes. The level of intercoder agreement from a random selection demonstrated a 98% level of agreement.[21] Remaining data was then systematically examined through these sets of codes to check for consistency and any emerging codes. Finally, themes were generated based on the agreed set of codes. Quantitative data analysis like calculation of median, percentage, and range was done for the demographic and clinical variables collected.
Ethical Approval and Informed Consent
All procedures performed in studies involving human participants were per the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethics approval was granted by the Institutional Ethics Committee (Project 900683/IEC III) at the Tata Memorial Centre, dated 18.11.2020. The committee waived the need for informed consent as the study utilized anonymized patient charts.
Results
Data from the chart review are presented below using tally counts to indicate the frequency of specific codes, subthemes, and themes. Most of the cases provided more than one, so the codes have been collapsed together to generate the final number of subthemes and themes. Of the 50 charts screened, 34 charts with complete data were identified and analyzed after reaching the point at which no new themes emerged.[14] Out of 34 participants, 23 were male and 11 were female. The demographic and clinical details of the patients are presented in [Table 1]. Average age of patients was 12 years (range 2–16 years).
|
Themes |
Subthemes |
Example quotes |
|---|---|---|
|
Child's understanding of the disease diagnosis and prognosis |
Ignorance/avoidance of communication about the disease |
I do not want to talk about it (P7) |
|
Something is there which is bad |
I am not sure, but I do not have a good feel about it (P13) |
|
|
Everything is fine |
All is well (P22) |
|
|
God will help with illness |
I leave it to God (P20) |
|
|
Knows it is cancer |
I know it is a dreadful disease (P16) |
|
|
Knows the exact diagnosis |
I know I have cancer (P17) |
|
|
Nature of communication between the child and the parents |
Child not communicating with the parents because they take stress |
I cannot watch my parents sad (P33) |
|
Child suspects parents have given partial information |
I am sure that my parents know everything, but they never tell me (P12) |
|
|
Caregivers choosing not to tell child |
We cannot tell him this (P18) |
|
|
Child choosing not to speak to parents |
I better not speak about it (P1) |
|
|
Open communication |
I share everything with my parents (P2) |
|
|
Recognized barriers to communication |
Child worries for the caregiver |
I feel sad for my parents (P30) |
|
Poor coping of the parents |
We cannot see him like this (P5) |
|
|
Parent's wishes to protect the child |
Nothing will happen to him (P31) |
|
|
Hope for cure |
My child will get better (P34) |
|
|
Child's preference |
I do not want to talk about it (P29) |
|
|
Conflicts and issues other than the disease |
My parents have dispute with my uncle (P23) |
|
|
Psychosocial interventions to improve communication |
Encouraged parents to communicate about the disease with the child |
You should talk to each other about this (P10) |
|
Supported child for better coping |
You should share your thoughts with someone (P21) |
|
|
Counseled caregivers to cope and support child |
You must be open and supportive about this (P11) |
|
References
- Lipstein EA, Brinkman WB, Britto MT. What is known about parents' treatment decisions? A narrative review of pediatric decision making. Med Decis Making 2012; 32 (02) 246-258
- Granek L, Krzyzanowska MK, Tozer R, Mazzotta P. Oncologists' strategies and barriers to effective communication about the end of life. J Oncol Pract 2013; 9 (04) e129-e135
- Verberne LM, Kars MC, Schouten-van Meeteren AYN. et al. Parental experiences and coping strategies when caring for a child receiving paediatric palliative care: a qualitative study. Eur J Pediatr 2019; 178 (07) 1075-1085
- Keim MC, Lehmann V, Shultz EL. et al. Parent-child communication and adjustment among children with advanced and non-advanced cancer in the first year following diagnosis or relapse. J Pediatr Psychol 2017; 42 (08) 871-881
- Muckaden M, Dighe M, Balaji P. et al. Paediatric palliative care: theory to practice. Indian J Palliat Care 2011; 17 (Suppl): S52-S60
- Myant KA, Williams JM. Children's concepts of health and illness: understanding of contagious illnesses, non-contagious illnesses and injuries. J Health Psychol 2005; 10 (06) 805-819
- Vincenten JA, Sector MJ, Rogmans W, Bouter L. Parents' perceptions, attitudes and behaviours towards child safety: a study in 14 European countries. Int J Inj Contr Saf Promot 2005; 12 (03) 183-189
- Korkmaz B. Theory of mind and neurodevelopmental disorders of childhood. Pediatr Res 2011; 69 (5 Pt 2): 101R-108R
- Aldridge J, Shimmon K, Miller M, Fraser LK, Wright B. ‘I can’t tell my child they are dying'. Helping parents have conversations with their child. Arch Dis Child Educ Pract Ed 2017; 102 (04) 182-187
- Bluebond-Langner M. Worlds of dying children and their well siblings. Death Stud 1989; 13 (01) 1-16
- Srinath S, Jacob P, Sharma E, Gautam A. Clinical practice guidelines for assessment of children and adolescents. Indian J Psychiatry 2019; 61 (Suppl. 02) 158-175
- Rutishauser C. Communicating with young people. Paediatr Respir Rev 2003; 4 (04) 319-324
- ;Mărginean CO, Meliţ LE, Chinceşan M. et al. Communication skills in pediatrics - the relationship between pediatrician and child. Medicine (Baltimore) 2017; 96 (43) e8399
- Morse JM. The significance of saturation. Qual Health Res 1995; 5 (02) 147-149
- Pridmore P, Bendelow G. Images of health: exploring beliefs of children using the ‘draw-and-write’ technique. Health Educ J 1995; 54 (04) 473-488
- Angell C, Alexander J, Hunt JA. ‘Draw, write and tell’: a literature review and methodological development on the ‘draw and write’ research method. J Early Child Res 2015; 13 (01) 17-28
- Scarponi D, Pession A. Play therapy to control pain and suffering in pediatric oncology. Front Pediatr 2016; 4 (DEC): 132
- Einarsdottir J, Dockett S, Perry B. Making meaning: children's perspectives expressed through drawings. Early Child Dev Care 2009; 179 (02) 217-232
- Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today 2017; 56: 29-34
- Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci 2013; 15 (03) 398-405
- O'Connor C, Joffe H. Intercoder reliability in qualitative research: debates and practical guidelines. Int J Qual Methods 2020; 19 DOI: 10.1177/1609406919899220.
- Edlynn E, Kaur H. The role of psychology in pediatric palliative care. J Palliat Med 2016; 19 (07) 760-762
- Warth M, Kessler J, Koehler F, Aguilar-Raab C, Bardenheuer HJ, Ditzen B. Brief psychosocial interventions improve quality of life of patients receiving palliative care: a systematic review and meta-analysis. Palliat Med 2019; 33 (03) 332-345
- Irwin LG, Johnson JL, Henderson A, Dahinten VS, Hertzman C. Examining how contexts shape young children's perspectives of health. Child Care Health Dev 2007; 33 (04) 353-359
- Booth CM, Hammad N. Childhood cancer care: closing equity gaps on the ground. Lancet Oncol 2020; 21 (04) 485-487
- Oakley A, Bendelow G, Barnes J, Buchanan M, Husain OAN. Health and cancer prevention: knowledge and beliefs of children and young people. BMJ 1995; 310 (6986): 1029-1033
- Reigada C, Sapeta P, Centeno C. The value of the ethnographic approach to research issues in palliative care. Curr Opin Support Palliat Care 2019; 13 (04) 337-343
- Salins N, Hughes S, Preston N. Palliative care in paediatric oncology: an update. Curr Oncol Rep 2022; 24 (02) 175-186


 PDF
PDF  Views
Views  Share
Share

