Chediak–Higashi Syndrome Presented With Hemophagocytic Lymphohistiocytosis
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2018; 39(01): 122-123
DOI: DOI: 10.4103/ijmpo.ijmpo_54_16
Sir,
Herein, we report a case of Chediak–Higashi syndrome (CHS) presented with hemophagocytic lymphohistiocytosis (HLH). A 3-year-old girl presented with recurrent infections, fever, and icterus. Physical examination revealed hepatosplenomegaly, bilateral cervical and inguinal lymphadenopathy, silvery gray hair, strabismus, and bilateral nystagmus. Giant granules in lymphocytes and monocytes were seen on blood smear. Bone marrow aspirate exhibited erythrophagocytosis and numerous giant granules of predominantly myeloid lineage [Figure 1]a. Examination of the hair showed an irregular distribution of large and small pigment clumps [Figure 1]b. Magnetic resonance imaging of the brain showed diffuse cerebral atrophic [Figure 1]c. The girl's parents were consanguineous. On laboratory examination, urinary analysis was unremarkable. Hemoglobin, white blood cell count, and thrombocyte count were 7, 6 g/dL, 2300/mm 3, and 76.000/mm 3, respectively. Sedimentation rate was 2 mm/h (N: 0–20 mm/h), and serum triglyceride 390 mg/dL (N: 32–99 mg/dL), fibrinogen 67 ng/dL (N: 200–400 ng/dL), and ferritin was 129.000 ng/mL (N: 7–140 ng/mL) [Table 1]. Prothrombin time was 21 s (N: 11–15 s), and activated partial thromboplastin time was 62 s (N: 25–35 s).
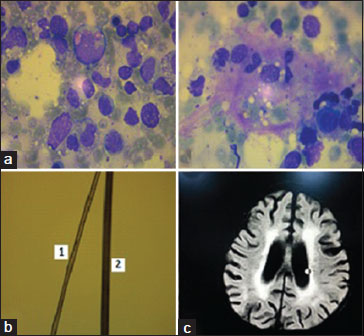
| Figure.1(a) Bone marrow aspirate smears showing giant cytoplasmic granules with in myeloid precursors and hemophagocytosis. (b) 1 patient’s hair, 2 Normal hair. (c) Magnetic resonance imaging images show diffüz cerebral atrophy
|
Result |
|
|---|---|
|
WBC – White blood cell; PLT – Platelet |
|
|
Hemoglobin (g/dL) |
7.6 |
|
WBC (/mm3) |
2300 |
|
PLT (/mm3) |
76.000 |
|
Sedimentation (mm/h) |
2 |
|
Triglyceride (mg/dL) |
390 |
|
Fibrinogen (ng/dL) |
67 |
|
Serum sodium (mEq/dL) |
122 |
|
Ferritin (ng/mL) |
129.000 |
Sir,
Herein, we report a case of Chediak–Higashi syndrome (CHS) presented with hemophagocytic lymphohistiocytosis (HLH). A 3-year-old girl presented with recurrent infections, fever, and icterus. Physical examination revealed hepatosplenomegaly, bilateral cervical and inguinal lymphadenopathy, silvery gray hair, strabismus, and bilateral nystagmus. Giant granules in lymphocytes and monocytes were seen on blood smear. Bone marrow aspirate exhibited erythrophagocytosis and numerous giant granules of predominantly myeloid lineage [Figure 1]a. Examination of the hair showed an irregular distribution of large and small pigment clumps [Figure 1]b. Magnetic resonance imaging of the brain showed diffuse cerebral atrophic [Figure 1]c. The girl's parents were consanguineous. On laboratory examination, urinary analysis was unremarkable. Hemoglobin, white blood cell count, and thrombocyte count were 7, 6 g/dL, 2300/mm 3, and 76.000/mm 3, respectively. Sedimentation rate was 2 mm/h (N: 0–20 mm/h), and serum triglyceride 390 mg/dL (N: 32–99 mg/dL), fibrinogen 67 ng/dL (N: 200–400 ng/dL), and ferritin was 129.000 ng/mL (N: 7–140 ng/mL) [Table 1]. Prothrombin time was 21 s (N: 11–15 s), and activated partial thromboplastin time was 62 s (N: 25–35 s).
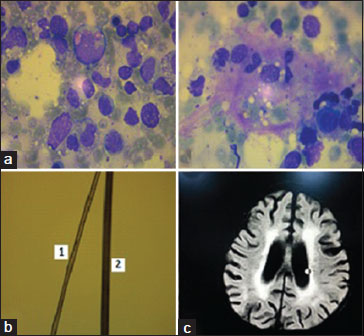
| Figure.1(a) Bone marrow aspirate smears showing giant cytoplasmic granules with in myeloid precursors and hemophagocytosis. (b) 1 patient’s hair, 2 Normal hair. (c) Magnetic resonance imaging images show diffüz cerebral atrophy
|
Result |
|
|---|---|
|
WBC – White blood cell; PLT – Platelet |
|
|
Hemoglobin (g/dL) |
7.6 |
|
WBC (/mm3) |
2300 |
|
PLT (/mm3) |
76.000 |
|
Sedimentation (mm/h) |
2 |
|
Triglyceride (mg/dL) |
390 |
|
Fibrinogen (ng/dL) |
67 |
|
Serum sodium (mEq/dL) |
122 |
|
Ferritin (ng/mL) |
129.000 |
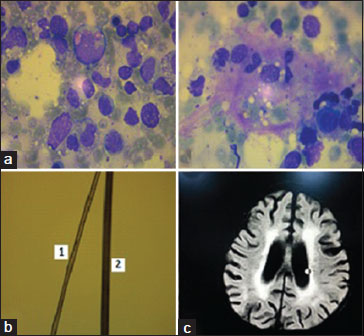
| Figure.1(a) Bone marrow aspirate smears showing giant cytoplasmic granules with in myeloid precursors and hemophagocytosis. (b) 1 patient’s hair, 2 Normal hair. (c) Magnetic resonance imaging images show diffüz cerebral atrophy
References
- Akbayram S, Akgun C, Basaranoglu M, Kaya A, Balta G, Ustyol LN. et al. A case of Chediak Higashi syndrome presented with hemophagocytic lymphohistiocytosis. Int J Hematol Oncol 2011; 21: 196-9
- Pujani M, Agarwal K, Bansal S, Ahmad I, Puri V, Verma D. et al. Chediak-higashi syndrome – A report of two cases with unusual hyperpigmentation of the face. Turk Patoloji Derg 2011; 27: 246-8
- Page AR, Berendes H, Warner J, Good RA. The Chediak-Higashi syndrome. Blood 1962; 20: 330-43
- Rubin CM, Burke BA, McKenna RW, McClain KL, White JG, Nesbit MEJr. et al. The accelerated phase of Chediak-Higashi syndrome. An expression of the virus-associated hemophagocytic syndrome?. Cancer 1685; 56: 524-30
- Barak Y, Nir E. Chediak-higashi syndrome. Am J Pediatr Hematol Oncol 1987; 9: 42-55


 PDF
PDF  Views
Views  Share
Share

