Cervical Cancer Screening: Comparing PAPs Smear with VIA/VILI in Semiurban Women of Delhi
CC BY 4.0 · Indian J Med Paediatr Oncol 2025; 46(02): 200-206
DOI: DOI: 10.1055/s-0044-1800949
Abstract
Introduction Screening with PAPs smear for screening of cervical cancer has been the gold standard for many years in high-income countries but has still not been successful in low- and middle-income country like India due to unavailability at public ground level. Thus, a simple, effective, and low-cost alternative to cervical cytology for cervical cancer prevention is urgently needed for high-risk, low-resource settings.
Objectives The aim was to compare the efficacy of visual inspection with acetic acid (VIA) and visual inspection with Lugol's iodine (VILI) with the PAP smear for screening precursor intraepithelial lesions and early signs of cervical cancer, and to evaluate their potential as alternative screening methods to the PAP smear in a semiurban population in Delhi.
Materials and Methods A total of 127 married, nonpregnant patients between 18 and 65 years were randomly selected from gynecology outpatient department. Then, PAP smear samples were taken from all patients followed by VIA and VILI. Biopsies were then taken from those who showed positive findings in either of the screening methods. Out of these, 50 PAP and VIA-negative women were included as a control group. The diagnostic accuracy of VIA and VILI was compared with PAP smear, for diagnosis of precancerous lesions.
Results VIA and VILI results were positive in 22 patients out of 127 (17.3%). PAP cytology report showed epithelial cell abnormality in 13 cases (10.2%) with atypical squamous cells of undetermined significance in 1 case, atypical glandular cells of undetermined significance in 4 cases, low-grade squamous intraepithelial lesion in 3 cases, and high-grade squamous intraepithelial lesions in 5 cases. PAP smear had showed better specificity (90.79%) and less sensitivity (85.71%) as compared with VIA and VILI method. Sensitivity of VIA was 100% and specificity was 80.26%. Similar parameters were seen with the VILI method also. The overall p-value for all the parameters of either screening method was > 0.05; hence, both methods are comparable for screening.
Conclusion VIA and VILI can be employed as initial screening tools in place of PAP smear, particularly in countries with limited resources or developing regions.
Keywords
visual inspection by acetic acid (VIA) - visual inspection by Lugol's iodine (VILI) - PAP smear - cancer cervix - screening - low- and middle-income countries (LMIC)Recommendations
The advantages of affordability, straightforward implementation, and a point-of-care diagnosis and treatment protocol should serve as compelling reasons for developing countries like India to adopt visual inspection as a screening method for cervical cancer.
Patient Consent
Informed patient consent was obtained for this study.
Ethics Statement
This article does not contain any studies with human participants or animals performed by any of the authors. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975, as revised in 2000. The resources used in the research were totally provided by the hospital and the Municipal Corporation of Delhi. Informed consent was obtained from all individual participants included in the study.
Publication History
Article published online:
11 December 2024
© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Cervical cancer screening feasibility study MorocOncoE6 comparing VIA with molecular HPV oncogene expression testingJ Saidi, VCOT Open, 2018
- Study on cervical cancer screening amongst nursesAstha Srivastava, Asian Journal of Oncology, 2016
- Cervical Cancer Screening with HPV Testing: Updates on the RecommendationCarla Fabrine Carvalho, Revista Brasileira de Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics
- Prevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian AmazonDaniel Valim Duarte, RBGO Gynecology and Obstetrics, 2017
- Prevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian AmazonDaniel Valim Duarte, Revista Brasileira de Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics, 2017
- P756 Cervical smear screening results amongst women with inflammatory bowel disease at an Irish hospital<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Cervical cancer screening history among women diagnosed with cervical cancer in Estonia 2017–18<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Breast and Cervical Cancer Screening: Reaching Women with Disabilities in Alaska.<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Cervical Cancer Screening Among Adult Women in China, 2010<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Evaluating Prior Pap Screening Intervals Among Women With Newly Diagnosed Cervical Cancer<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
Abstract
Introduction Screening with PAPs smear for screening of cervical cancer has been the gold standard for many years in high-income countries but has still not been successful in low- and middle-income country like India due to unavailability at public ground level. Thus, a simple, effective, and low-cost alternative to cervical cytology for cervical cancer prevention is urgently needed for high-risk, low-resource settings.
Objectives The aim was to compare the efficacy of visual inspection with acetic acid (VIA) and visual inspection with Lugol's iodine (VILI) with the PAP smear for screening precursor intraepithelial lesions and early signs of cervical cancer, and to evaluate their potential as alternative screening methods to the PAP smear in a semiurban population in Delhi.
Materials and Methods A total of 127 married, nonpregnant patients between 18 and 65 years were randomly selected from gynecology outpatient department. Then, PAP smear samples were taken from all patients followed by VIA and VILI. Biopsies were then taken from those who showed positive findings in either of the screening methods. Out of these, 50 PAP and VIA-negative women were included as a control group. The diagnostic accuracy of VIA and VILI was compared with PAP smear, for diagnosis of precancerous lesions.
Results VIA and VILI results were positive in 22 patients out of 127 (17.3%). PAP cytology report showed epithelial cell abnormality in 13 cases (10.2%) with atypical squamous cells of undetermined significance in 1 case, atypical glandular cells of undetermined significance in 4 cases, low-grade squamous intraepithelial lesion in 3 cases, and high-grade squamous intraepithelial lesions in 5 cases. PAP smear had showed better specificity (90.79%) and less sensitivity (85.71%) as compared with VIA and VILI method. Sensitivity of VIA was 100%. and specificity was 80.26%. Similar parameters were seen with the VILI method also. The overall p-value for all the parameters of either screening method was > 0.05; hence, both methods are comparable for screening.
Conclusion VIA and VILI can be employed as initial screening tools in place of PAP smear, particularly in countries with limited resources or developing regions.
Keywords
visual inspection by acetic acid (VIA) - visual inspection by Lugol's iodine (VILI) - PAP smear - cancer cervix - screening - low- and middle-income countries (LMIC)Introduction
Carcinoma cervix is the fourth most common cancer among women worldwide, while in low- and middle-income countries (LMICs) it ranks second in gynecological cancers, with approximately 660,000 new cases and 350,000 deaths globally in 2022.[1] GLOBOCAN also estimated an age-standardized incidence rate of 18 per 100,000 women and a cumulative risk of 2.01%.[2] The cervical cancer occurs as a result of long-term persisting infection with high-risk human papillomavirus (HPV), which is accountable for 90 to 100%. of cervical cancer cases. Out of which high-risk type 16 and 18 are the two most common, and constitute for about 70%. of carcinoma cervix cases.[3]
High-risk behaviors are poor genital hygiene, early age at marriage, early age at first sexual intercourse, multiple partners, repeated pregnancies, long-term contraceptive use particularly oral contraceptives, smoking, and multiparity, which increase the risk of acquiring HPV in women.[4] Though deadliest, yet it is one cancer which is preventable if an effective treatment is given at an earliest stage, which is easily detectable by routine screening. There are approximately 272.8 million women eligible for screening in India.[5] Numerous efforts are in progress for the prevention of cervical cancer by both the government and nonprofit organizations since long but are yet to make any meaningful impact. The screening methods employed by most advanced countries include PAP smear, HPV deoxyribonucleic acid testing, visual inspection with acetic acid (VIA), or a combination of all these. The United States and other high-income countries have reported a reduction in number of new cases of carcinoma cervix by routine screening with PAP smear in sexually active women.[6] The implementation of PAP smears in low resource settings like India is limited due to inadequate health care infrastructure, restricted health budgets, and a shortage of laboratories and specialized personnel needed for slide preparation and diagnosis. Repeat PAPs smear is needed once every 3 years due to its lower sensitivity. Technical and financial limitations in organizing cytology screenings have prompted the evaluation of visual inspection methods as viable alternatives.
HPV testing is also recommended as an alternative for screening, but it is associated with high costs. Thus, visual inspection methods like VIA and visual inspection with Lugol's iodine (VILI) are the low-cost screening tools that have been proposed as alternatives to PAP smear-based programs, with VIA being the most commonly employed and researched. VIA is simple, cost-effective, and easily scalable for large populations. It requires no laboratory support and can be reliably performed by trained paramedical staff, nurses, and doctors. However, the gold standard for diagnosis of cervical dysplasia is colposcopy-guided biopsy but it is more time-consuming and requires handling by a specialist with good experience.[7] Thus, in this study, it is hypothesized that visual inspection methods have similar screening efficacy as compared with PAPs, and hence they can replace PAPs for mass screening. They have the potential to be utilized as an alternate first screening method and be a pragmatic and effective public health approach for cervical cancer prevention.
Materials and Methods
Study Design
This is a cross-sectional study, carried out at the Department of Obstetrics and Gynecology, Kasturba Hospital, Delhi, India, after due clearance from the institutional ethical committee.
Sample Size
A total of 127 patients were selected from the gynecology outpatient department (OPD) and enrolled for the study after informed consent. The sample size was calculated as per the study by Das et al,[8] using the formula:

The minimum sample size was around 102.67, nearly = 103, taking Zα at a confidence level of 95%. as 1.96. L as margin of error = 5%. P is the prevalence of preinvasive lesion of cervical cancer being 7.2%.[9]
Inclusion Criterion
Only married, nonpregnant women between the age group of 18 and 65 years were included.
Exclusion Criterion
Unmarried women, women with confirmed or suspected pregnancy, those having active bleeding per vaginal, previously diagnosed and treated cases of cervical intraepithelial lesion or carcinoma cervix, posthysterectomy patients, and females with major degree of uterine prolapse were excluded from the present study.
Ethics
The institutional ethics committee approved the study, number: D /880/KH/2022 dated August 30, 2022. All participants were explained about the purpose of the study in detail. Consent was taken for participation and all the procedures. Their participation in the study was completely voluntary with the option to withdraw anytime during study. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional) and with the Helsinki Declaration of 1964, as revised in 2000.
Most women in this hospital-based study are from semiurban areas of Delhi, presenting to the gynecological OPD with various complaints such as vaginal discharge, abnormal bleeding, and other related issues. A detailed pro forma was filled including their socioeconomic status and other demographic details, followed by proper clinical examination. PAP smear samples were taken from all patients followed by VIA and VILI.
VIA was performed by applying 3 to 5%. acetic acid on to the ectocervix, findings were observed after a gap of 60 seconds. The test results were reported as VIA positive if clearly demarcated, opaque/dense acetowhite lesions with well-defined or raised margins, in the transformation zone or close to the squamocolumnar junction (SCJ), were present. The time taken to appear and disappear was also noted. The location of lesion and area as demarcated by quadrant involvement were also noted. The patients who did not take up white color on acetic acid or showed faint acetowhitening, which disappeared in less than 60 seconds (early to appear, early to disappear), were classified as VIA negative.
VILI was done by Lugol's iodine application to the ectocervix and it was visualized within 30 seconds. The test results were reported as VILI positive if there was presence of bright canary yellow/mustard yellow/saffron yellow areas, without any iodine uptake seen in the transformation zone close to or abutting the SCJ, or when the entire ectocervix seems yellow.
A total 50 VIA/VILI and PAPs negative cases were taken as controls from this group. PAPs smear was reported using the Bethesda System 2014.[10] Biopsy was taken in those who showed positive findings in either of the screening method, and random four-quadrant biopsy was taken from these 50 controls.
Patients were followed up in the OPD for 2 weeks. Further management was done as per the diagnosis established and hospital management protocol. The study outcomes were measured as per the following:
Primary outcome: Diagnostic accuracy of VIA and VILI for screening of preinvasive and early manifestations of carcinoma cervix.
Secondary outcome: Comparison of diagnostic accuracy including sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of VIA and VILI with PAPs smear for the detection of intraepithelial lesions, preinvasive, and early manifestations of carcinoma cervix.
Statistical Analysis
The collected data was entered in Microsoft Excel and statistically evaluated using Statistical Package for Social Sciences (SPSS) version 25.0. Sensitivity, specificity, PPV, and NPV of each screening test were calculated. Chi-square test was performed and a p-value of less than 0.05 was considered statistically significant.
Results
Majority of the study participants belonged to the age group of 30 to 39 years (40.2%) and lower middle-class category from semiurban areas of Delhi. Note that 50.4%. of women in our study group had > 2 children. The mean age at coitus was 20.11 ± 3.65 years. Majority of patients presented with pelvic inflammatory symptom (88.9%), and only 8 patients had postcoital bleeding.
Ninety-six patients (75.6%) had negative PAP smear report for intraepithelial lesion or malignancy. Thirteen out of 127 women showed epithelial cell abnormality on PAPs (10.2%), with atypical squamous cells of undetermined significance (ASCUS) in 1 case, atypical glandular cells of undetermined significance (AGUS) in 4 cases, low-grade squamous intraepithelial lesion (LSIL) in 3 cases, and high-grade squamous intraepithelial lesions (HSIL) in 5 cases. All patients with AGUS on PAP report were further evaluated by endocervical curettage and endometrial aspiration biopsy, which came out to be negative in all four cases. These patients were advised for regular follow-up.
Twenty-two women were positive for both VIA and VILI (17.3%). The positive results on VIA and VILI were same in the study participants. Comparing VIA and VILI with PAP, of 105 VIA-negative cases, PAP detected 1 LSIL, 1 ASCUS, and 4 AGUS ([Table 1]) ([Fig. 1]).
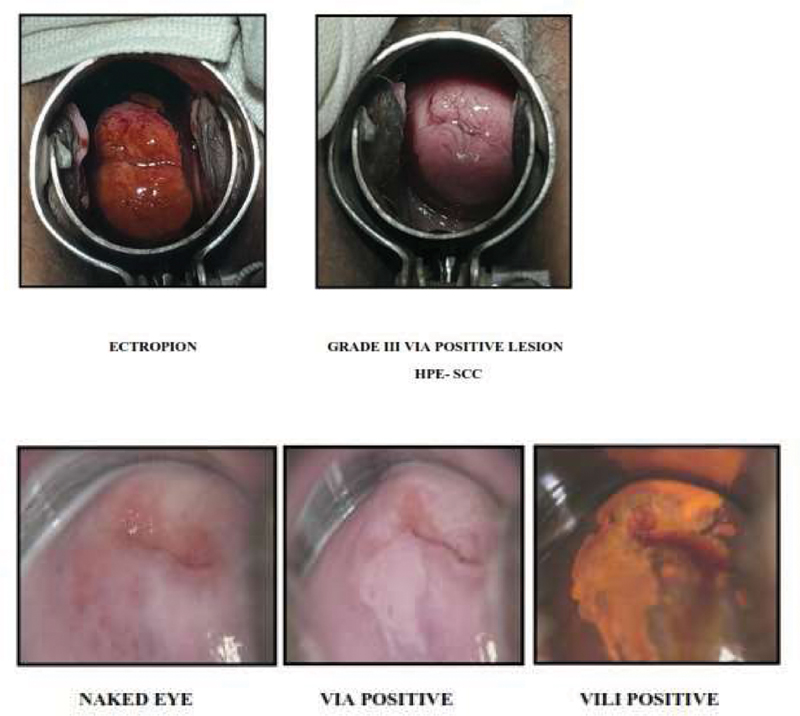
Fig 1: Visual inspection with acetic acid/visual inspection with Lugol's iodine (VIA/VILI) appearance.
Cervical biopsies were performed on 78 patients: 28 with positive screening results (either PAP positive or positive on both VIA and VILI) and 50 controls. Histopathology from cervical biopsy was used as the confirmatory test, serving as the gold standard for evaluating the diagnostic efficacy of PAP, VIA, and VILI in detecting preinvasive cervical lesions.
For these 78 patients, sensitivity, specificity, PPV, and NPV were calculated for each diagnostic method (PAP, VIA, and VILI) by constructing 2 × 2 tables. Groups of subjects were organized according to test results from each method, and outcomes were compared against the histopathology results. The chi-square test was used to assess diagnostic accuracy, with statistical significance set at a p-value < 0.05.
The data shows that the PAP smear has better specificity (90.79%) as compared with that of VIA (80.26%) and VILI (80.26%), which means PAP has better ability to designate a patient without disease as negative.
Whereas the sensitivity of VIA (100%) and VILI (100%) is much better than that of PAP smear reports (85.71%), that is, they have better ability to designate an individual with disease as positive.
The PPV of PAPs is better (46.15%) than the PPV of VIA (31.82%) and VILI (31.82%), whereas the NPV is better with VIA (100%) and VILI (100%) than that of PAP smear (98.57%).
But the overall p-value of comparisons of diagnostic accuracy of all the three methods, that is, PAPs, VIA, and VILI is > 0.05; hence, the difference is not statistically significant.
Abnormal histopathology was found in seven cases (cervical intraepithelial neoplasia [CIN] grade 1 in two cases and squamous cell carcinoma in five cases), all of which VIA/VILI detected, yielding a 100%. NPV. Of 13 PAP-positive cases, only 6 showed abnormal biopsy results. PAP smear showed better specificity (90.79%) but lower sensitivity (85.71%) compared with VIA/VILI, which had 80.26%. specificity and 100%. sensitivity. The PPV/NPV for PAP were 46.15%/98.57%, and for VIA/VILI, 31.82%/100% ([Tables 2] [3] [4]).
|
VIA |
VILI |
PAP smear |
–p-Value |
|||
|---|---|---|---|---|---|---|
|
VIA vs. VILI |
VIA vs. PAP |
VILI vs. PAP |
||||
|
Sensitivity |
100% |
100% |
85.71% |
– |
1 |
1 |
|
Specificity |
80.26% |
80.26% |
90.79% |
– |
0.06 |
0.06 |
|
Positive predictive value |
31.82% |
31.82% |
46.15% |
– |
0.14 |
0.14 |
|
Negative predictive value |
100% |
100% |
98.57% |
– |
0.98 |
0.98 |
|
Accuracy |
81.93% |
81.93% |
90.36% |
– |
0.11 |
0.11 |
References
-
Accessed May 20, 2024 at: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
- Sung H, Ferlay J, Siegel RL. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- Wheeler CM. HPV genotypes: implications for worldwide cervical cancer screening and vaccination. Lancet Oncol 2010; 11 (11) 1013-1014
-
Accessed September 17, 2024 at: https://www.cancer.org/cancer/types/cervical-cancer/causes-risks-prevention/risk-factors.html
- Bhatla N, Meena J, Kumari S, Banerjee D, Singh P, Natarajan J. Cervical cancer prevention efforts in India. Indian J Gynecol Oncol 2021; 19 (03) 41
- Cubie HA, Campbell C. Cervical cancer screening - the challenges of complete pathways of care in low-income countries: focus on Malawi. Womens Health (Lond Engl) 2020; 16: 1745506520914804
- Blumenthal PD, Gaffikin L, Chirenje ZM, McGrath J, Womack S, Shah K. Adjunctive testing for cervical cancer in low resource settings with visual inspection, HPV, and the Pap smear. Int J Gynaecol Obstet 2001; 72 (01) 47-53
- Pangarkar MA. The Bethesda System for reporting cervical cytology. Cytojournal 2022; 19: 28
-
Accessed November 30, 2024 at: https://www.who.int/publications/i/item/9789240030824
- Huy NVQ, Tam LM, Tram NVQ. et al. The value of visual inspection with acetic acid and Pap smear in cervical cancer screening program in low resource settings - a population-based study. Gynecol Oncol Rep 2018; 24: 18-20
- Goldie SJ, Gaffikin L, Goldhaber-Fiebert JD. et al; Alliance for Cervical Cancer Prevention Cost Working Group. Cost-effectiveness of cervical-cancer screening in five developing countries. N Engl J Med 2005; 353 (20) 2158-2168
-
- Ami S Y, Singh R. A prospective study of comparison Pap's smear, Vili's Test and colposcopy in cervical cancer screening. Int J Med Res Health Sci 2016; 5 (04) 50-57
-
- Sinha S, Singh V, Mishra B, Singh A. Comparing the efficacy of visual inspection of cervix with acetic acid and Lugol's iodine with Pap smear cytology in screening for cancer cervix. J Curr Res Sci Med 2018; 4 (01) 10-16
- Consul S, Agrawal A, Sharma H, Bansal A, Gutch M, Jain N. Comparative study of effectiveness of Pap smear versus visual inspection with acetic acid and visual inspection with Lugol's iodine for mass screening of premalignant and malignant lesion of cervix. Indian J Med Paediatr Oncol 2012; 33 (03) 161-165
- Shastri SS, Dinshaw K, Amin G. et al. Concurrent evaluation of visual, cytological and HPV testing as screening methods for the early detection of cervical neoplasia in Mumbai, India. Bull World Health Organ 2005; 83 (03) 186-194
-
- Juneja A, Sehgal A, Sharma S, Pandey A. Cervical cancer screening in India: strategies revisited. Indian J Med Sci 2007; 61 (01) 34-47
-
- Davis-Dao CA. et al Effect of cervicitis on visual inspection with acetic acid. Journal of Lower Genital Tract Disease 2008; 12 (04) 282-286
- Ngoma T, Muwonge R, Mwaiselage J, Kawegere J, Bukori P, Sankaranarayanan R. Evaluation of cervical visual inspection screening in Dar es Salaam, Tanzania. Int J Gynaecol Obstet 2010; 109 (02) 100-104
- Cervical cancer screening feasibility study MorocOncoE6 comparing VIA with molecular HPV oncogene expression testingJ Saidi, VCOT Open, 2018
- Study on cervical cancer screening amongst nursesAstha Srivastava, Asian Journal of Oncology, 2016
- Cervical Cancer Screening with HPV Testing: Updates on the RecommendationCarla Fabrine Carvalho, Revista Brasileira de Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics
- Prevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian AmazonDaniel Valim Duarte, RBGO Gynecology and Obstetrics, 2017
- Prevalence of Human Papillomavirus Infection and Cervical Cancer Screening among Riverside Women of the Brazilian AmazonDaniel Valim Duarte, Revista Brasileira de Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics, 2017
- Sharing Cellavision Blood Smear Images with Clinicians Via the Electronic Medical Record<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Development of a Screening Tool in Women Presenting with Unexplained Menorrhagia.<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Do Aromatase Inhibitors Increase Hemoglobin in Women with Breast Cancer?<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Colorectal Cancer Screening in Patients with Inherited Bleeding Disorders: High Cancer Detection Rate in Hemophilia Patients<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Screening Tool for Bleeding Disorders in Women with Menorrhagia: Evaluation in a Prospective US Multi-Site Cohort.<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
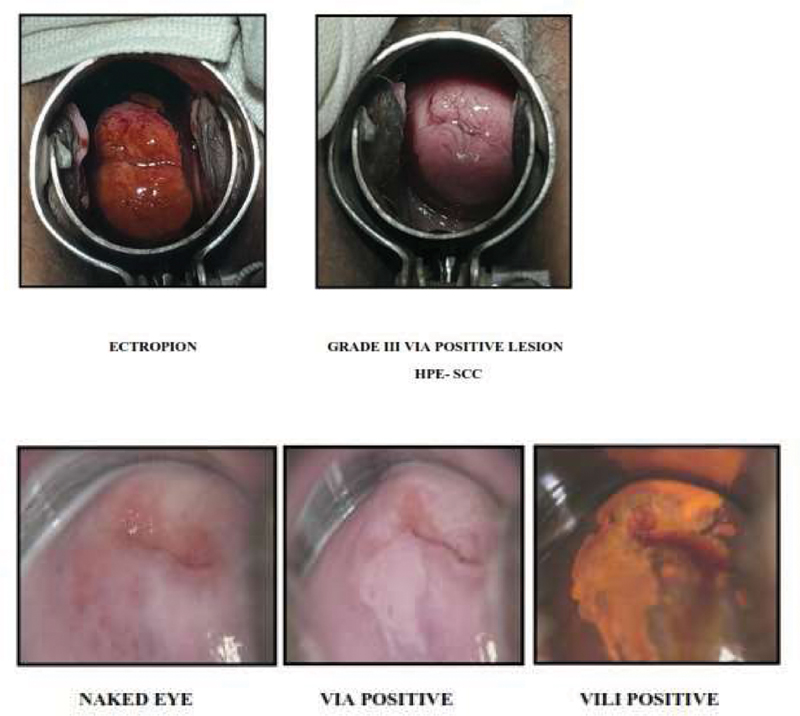
Fig 1: Visual inspection with acetic acid/visual inspection with Lugol's iodine (VIA/VILI) appearance.
References
-
Accessed May 20, 2024 at: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
- Sung H, Ferlay J, Siegel RL. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- Wheeler CM. HPV genotypes: implications for worldwide cervical cancer screening and vaccination. Lancet Oncol 2010; 11 (11) 1013-1014
-
Accessed September 17, 2024 at: https://www.cancer.org/cancer/types/cervical-cancer/causes-risks-prevention/risk-factors.html
- Bhatla N, Meena J, Kumari S, Banerjee D, Singh P, Natarajan J. Cervical cancer prevention efforts in India. Indian J Gynecol Oncol 2021; 19 (03) 41
- Cubie HA, Campbell C. Cervical cancer screening - the challenges of complete pathways of care in low-income countries: focus on Malawi. Womens Health (Lond Engl) 2020; 16: 1745506520914804
- Blumenthal PD, Gaffikin L, Chirenje ZM, McGrath J, Womack S, Shah K. Adjunctive testing for cervical cancer in low resource settings with visual inspection, HPV, and the Pap smear. Int J Gynaecol Obstet 2001; 72 (01) 47-53
- Pangarkar MA. The Bethesda System for reporting cervical cytology. Cytojournal 2022; 19: 28
-
Accessed November 30, 2024 at: https://www.who.int/publications/i/item/9789240030824
- Huy NVQ, Tam LM, Tram NVQ. et al. The value of visual inspection with acetic acid and Pap smear in cervical cancer screening program in low resource settings - a population-based study. Gynecol Oncol Rep 2018; 24: 18-20
- Goldie SJ, Gaffikin L, Goldhaber-Fiebert JD. et al; Alliance for Cervical Cancer Prevention Cost Working Group. Cost-effectiveness of cervical-cancer screening in five developing countries. N Engl J Med 2005; 353 (20) 2158-2168
-
- Ami S Y, Singh R. A prospective study of comparison Pap's smear, Vili's Test and colposcopy in cervical cancer screening. Int J Med Res Health Sci 2016; 5 (04) 50-57
-
- Sinha S, Singh V, Mishra B, Singh A. Comparing the efficacy of visual inspection of cervix with acetic acid and Lugol's iodine with Pap smear cytology in screening for cancer cervix. J Curr Res Sci Med 2018; 4 (01) 10-16
- Consul S, Agrawal A, Sharma H, Bansal A, Gutch M, Jain N. Comparative study of effectiveness of Pap smear versus visual inspection with acetic acid and visual inspection with Lugol's iodine for mass screening of premalignant and malignant lesion of cervix. Indian J Med Paediatr Oncol 2012; 33 (03) 161-165
- Shastri SS, Dinshaw K, Amin G. et al. Concurrent evaluation of visual, cytological and HPV testing as screening methods for the early detection of cervical neoplasia in Mumbai, India. Bull World Health Organ 2005; 83 (03) 186-194
-
- Juneja A, Sehgal A, Sharma S, Pandey A. Cervical cancer screening in India: strategies revisited. Indian J Med Sci 2007; 61 (01) 34-47
-
- Davis-Dao CA. et al Effect of cervicitis on visual inspection with acetic acid. Journal of Lower Genital Tract Disease 2008; 12 (04) 282-286
- Ngoma T, Muwonge R, Mwaiselage J, Kawegere J, Bukori P, Sankaranarayanan R. Evaluation of cervical visual inspection screening in Dar es Salaam, Tanzania. Int J Gynaecol Obstet 2010; 109 (02) 100-104


 PDF
PDF  Views
Views  Share
Share

