Case of childhood laryngeal papillomatosis with metastatic carcinoma esophagus in adulthood
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2013; 34(01): 34-37
DOI: DOI: 10.4103/0971-5851.113420
Abstract
A young male patient was diagnosed to have laryngeal papillomas at the age of 3 years for which he underwent permanent tracheostomy and also multiple surgical and laser excision procedures. Then, later in life, the patient had progressive breathlessness and dysphagia. On examination, he had supraclavicular lymphadenopathy showing squamous carcinoma pathology. Since laryngeal papillomas have a high propensity to transform into laryngeal squamous cell carcinoma, he was first evaluated for laryngeal carcinoma which was negative. Esophagoscopy showed a growth in the esophagus, the biopsy of which was positive for squamous malignant cells. Patient was then started on palliative chemotherapy with combination of paclitaxel and carboplatin, and at progression with weekly nanoxel with stable disease. This is a rare case of childhood laryngeal papillomatosis progressing to metastatic esophageal carcinoma. This case has been presented to highlight the fact that patients with laryngeal papillomas are not only at high risk of progressing to laryngeal carcinoma but can also have other malignancies of the upper aerodigestive tract and lung. Most of them have been correlated to human papilloma virus (HPV), but in our patient HPV DNA was negative.
Publication History
Article published online:
20 July 2021
© 2013. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
A young male patient was diagnosed to have laryngeal papillomas at the age of 3 years for which he underwent permanent tracheostomy and also multiple surgical and laser excision procedures. Then, later in life, the patient had progressive breathlessness and dysphagia. On examination, he had supraclavicular lymphadenopathy showing squamous carcinoma pathology. Since laryngeal papillomas have a high propensity to transform into laryngeal squamous cell carcinoma, he was first evaluated for laryngeal carcinoma which was negative. Esophagoscopy showed a growth in the esophagus, the biopsy of which was positive for squamous malignant cells. Patient was then started on palliative chemotherapy with combination of paclitaxel and carboplatin, and at progression with weekly nanoxel with stable disease. This is a rare case of childhood laryngeal papillomatosis progressing to metastatic esophageal carcinoma. This case has been presented to highlight the fact that patients with laryngeal papillomas are not only at high risk of progressing to laryngeal carcinoma but can also have other malignancies of the upper aerodigestive tract and lung. Most of them have been correlated to human papilloma virus (HPV), but in our patient HPV DNA was negative.
INTRODUCTION
Recurrent laryngeal papillomas progressing to laryngeal carcinoma is well known. Here we present a case of recurrent laryngeal papillomatosis progressing to esophageal carcinoma and its management.
CASE REPORT
A 29-year-old male patient, a nonsmoker, was referred to our center in June 1993 with history of repeated episodes of breathlessness since the age of 3 years. Workup resulted in a diagnosis of multiple laryngeal papillomas [Figure 1]. Breathlessness in laryngeal papillomas is because of air flow obstruction due to structural interference. For these attacks of breathlessness, the patient had undergone a permanent tracheostomy at the age of 3 years. Since childhood, the patient had undergone multiple surgeries for laryngeal papilloma excision, about twice monthly, and was then referred to our center for further management. Since 1993, the patient has been on regular follow-up with multiple repeated laser excisions; the last excision was done 1½ years ago.
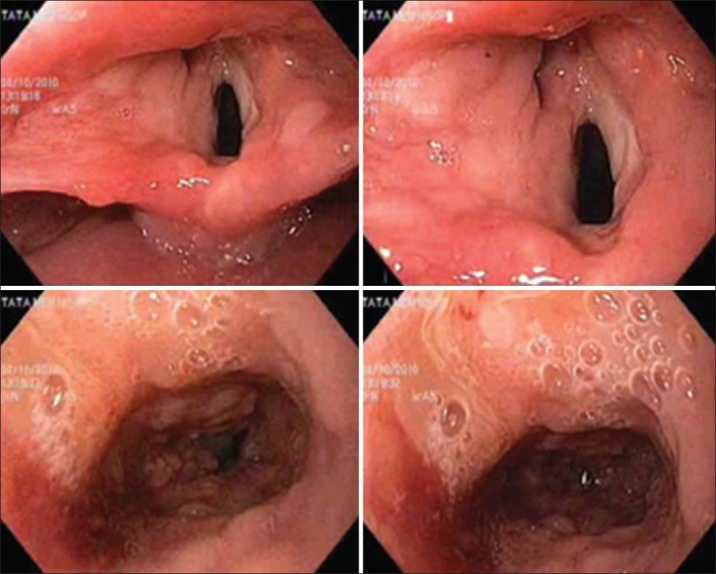
| Fig. 1 Multiple papillomas seen in the infraglottic region
Laryngeal papillomatosis is a benign condition in which there are multiple polypoidal growths in the larynx. It is the most common benign airway neoplasm in children.[1] Laryngeal involvement is usually seen in 100% of cases, trachea is involved in 3-26%, and pulmonary involvement is seen in 1-3% of cases.[2,3] The incidence in children is around 4.3 per 100,000 and about three-fourths of them are symptomatic by the age of 3 years.[4,5] In a study by Armstromg et al., out of 399 children, the mean number of surgeries per child was 4.4 per year and children who were diagnosed before the age of 3 years had two or more anatomical sites affected[6] and had more aggressive disease. The symptoms can vary from chronic cough, hemoptysis, breathlessness, stridor, hoarseness of voice, and some patients may be asymptomatic. It is caused by human papilloma virus (HPV), with the child getting infected during vaginal delivery, and subtypes 6 and 11 account for more than 90% cases.[7,8] Failure of both humoral and cell-mediated immunity to limit the uncontrolled proliferation of HPV-infected cells leads to the formation of laryngeal papillomas, and hence the patient's level of immunocompetence decides the aggressiveness of the disease.[7] The rate of tracheostomy is around 11% according to Armstrong et al.,[6] and Scraff et al.[1] in their study found a rate of 14% in patients who were treated with cidofovir. Scraff et al. did a web-based survey, which included 700 patients, among whom 25 patients died and in 89% of them the main causes of mortality were progressive pulmonary disease, complications during anesthesia, and malignant transformation of the disease.
HPV infects the keratinocyte within the basal layer of airway mucosa[9] and activates the epidermal growth factor receptor (EGFR) pathway and inactivates several tumor suppressor proteins, thus leading to cellular proliferation and defective epithelial differentiation.[10]
Further, it has been proposed that the oncoproteins of HPV, E6 and E7, promote rapid degradation of tumor suppressor proteins (p53 and pRB-retinoblastoma), thus interfering with cell growth control[8,11] and progressing to malignant transformation. In a study by Stephen et al., the contribution of promoter hypermethylation to the pathogenesis of respiratory papillomatosis and progression to squamous cell carcinoma (SCC) was analyzed in a cohort of 25 laryngeal papilloma cases. Aberrant methylation of CDKN2B and TIMP3 was most frequent and promoter hypermethylation of BRCA2, APC, CDKN2A, and CDKN2B was detected in two cases with subsequent progression to SCC. Of the 25 cases, 22 were positive for HPV-6, 2 for HPV-11, and 1 for HPV-16 and 33.[12] In juvenile cases, Derkay[4] reported a transformation rate of < 1%, while in adults a rate of 3-7% has been described.[8]
In September 2010, our patient presented with dysphagia, 7 kg weight loss over the past 4 months, and difficulty in breathing in spite of tracheostomy. On examination, he had abnormally enlarged bilateral level 4 lymph nodes. His computed tomography (CT) scan neck and thorax [Figure 2] revealed large right supraclavicular lymph node with central necrosis, measuring 3 cm, and small bilateral cervical, pretracheal, and subcarinal lymph nodes, with the largest measuring 1.8 cm. A large superior mediastinal soft tissue density mass lesion encasing and compressing the trachea, extending from supraclavicular region to the middle mediastinum, was present. The lesion encased the left carotid, right brachiocephalic trunk, and superior and mid esophagus. Laryngeal airway was mildly compromised.
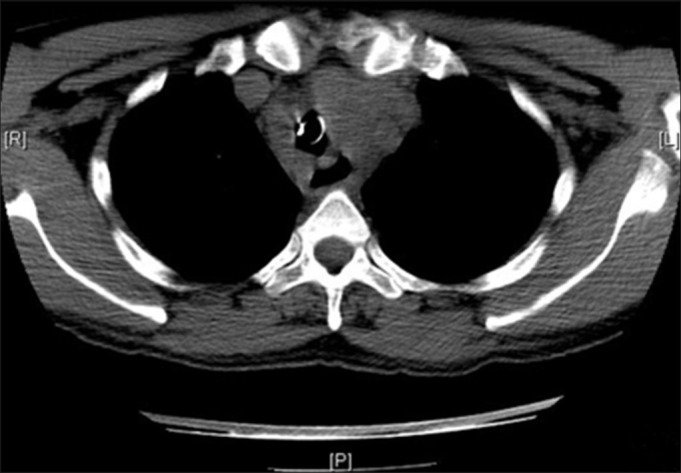
| Fig. 2 Computed tomography scan showing mediastinal lymphadenopath
With a background of recurrent papillomatosis, the first possibility of worsening symptoms with cervical lymphadenopathy is laryngeal carcinoma because there is a risk of 3-7%[11,13] of laryngeal papillomas progressing to SCC of the larynx. But in our patient, punch biopsy from the larynx lesion was negative for malignancy. Patients with laryngeal papillomas are also at increased risk for other head and neck, esophageal, and lung SCCs.
Fine needle aspiration cytology (FNAC) of cervical lymph node was suggestive of metastatic SCC. To diagnose the primary site of malignancy, direct laryngoscopy was performed. This revealed supraglottic thickening along with a circumferential tumor below the vocal cords, extending distally, and was fragile and bleeding on touch. This raised the suspicion of laryngeal malignancy; hence, a punch biopsy was done. Histopathology showed a proliferating squamous lesion with papillary architecture. Surface epithelium showed few cells with features of HPV-associated changes. Focal mild dysplasia was seen. Features were consistent with laryngeal papillomatosis. There was no evidence of malignancy and HPV from the lesion was negative [Figure 3].
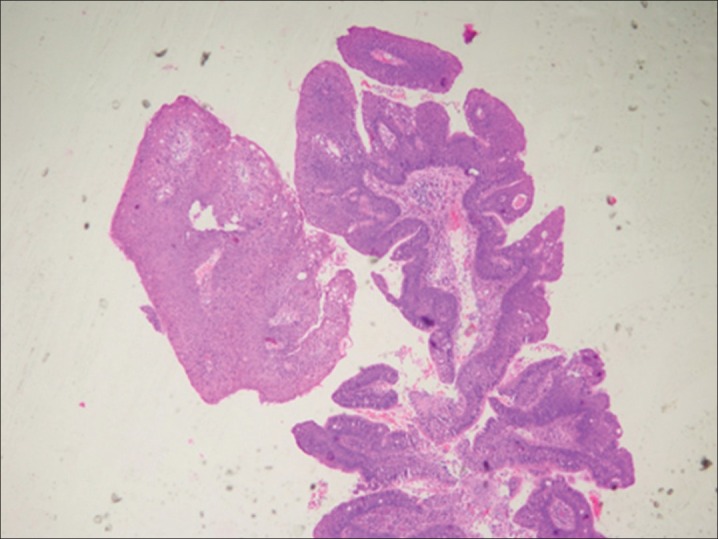
| Fig. 3 Slide of laryngeal papilloma
Since suspicion of malignancy was high, further examination of the upper aerodigestive tract was performed. Upper gastrointestinal (UGI) endoscopy showed infiltrated areas (patches) in the esophagus from 20 to 22 cm and the distal end was free. Biopsy from the lesion was performed which revealed squamous cells with hyperchromatic nuclei suggestive of SCC, which was correlating with the histopathology of the cervical lymph node [Figure 4]. Thus, our patient was diagnosed with SCC of the esophagus. The most common association of laryngeal papillomatosis and carcinoma has been correlated to the presence of HPV DNA synergistic with mucosal irritation, but in our patient HPV was negative.
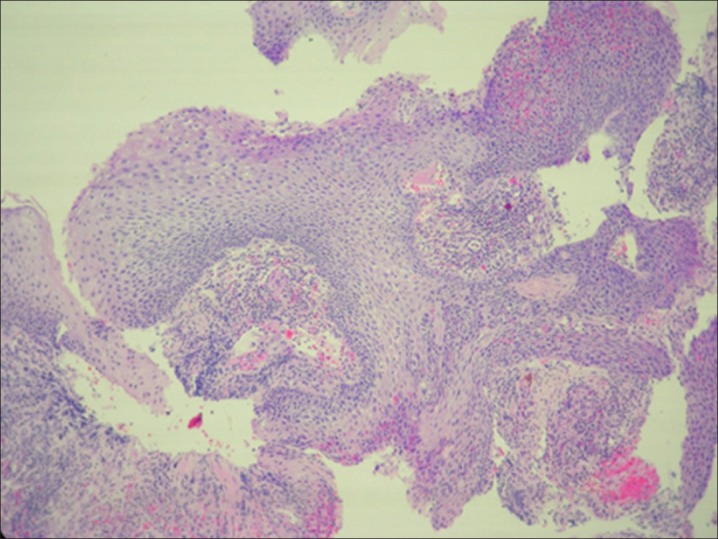
| Fig. 4 Slide of squamous carcinoma
The disease was locally advanced and not amenable to therapy with definitive intent, hence he was started on palliative chemotherapy with paclitaxel (175 mg/m2 on day 1) and carboplatin (AUC 5) every 21 days. After the first cycle of chemotherapy, the patient had significant improvement in dysphagia, he was able to take solid food, cervical nodes were not palpable, and there was complete resolution of breathing difficulty. CT scan after four cycles was suggestive of significant reduction in the mediastinal soft tissue and right supraclavicular nodal mass to 1.1 cm, and so the patient was given a total of six cycles.
One month later, the patient once again presented with increasing dysphagia. CT scan showed enlarged bilateral level 3 and 4 lymph nodes, the largest of which measured 1.7 × 1.4 cm. Repeat UGI scopy showed an ulceroproliferative tumor, measuring from 16 to 27 cm in the esophagus. In view of progressive disease, second-line chemotherapy was administered with nanoxel (cremaphor-free paclitaxel using nanotechnology) 100 mg/m2 weekly. Following 8 weeks of chemotherapy, reassessment CT scan suggested stable disease. Patient is now continuing on weekly nanoxel for the past 3 months.
DISCUSSION
Management
Treatment of recurrent laryngeal papillomatosis is difficult, with the disease showing remissions and recurrences. Our patient had undergone multiple excisions till the age of 29 years and then after that has undergone CO2 laser excision at our center which has shown good results in the management of recurrent laryngeal papillomatosis.[13] Other options tried in literature are inhalational interferon,[13] intralesional cidofovir,[14] propranolol,[15] imiquimod and ribavirin,[7] with variable results. The most important factor predisposing patients of laryngeal papilloma to carcinoma was found to be prior radiation therapy to this benign lesion.[16] In the Mayo clinic case series of 101 cases, it was found that 14% of patients who were treated with radiation developed SCC of the larynx, whereas patients treated with surgery did not.[17] Our patient initially underwent surgical excisions of laryngeal papilloma outside followed by laser excisions at our center. There is not much literature on the consequences of laser therapy for laryngeal papilloma.
There is no definitive literature available on whether the management of laryngeal or esophageal carcinoma differs in a patient with recurrent laryngeal papillomatosis. In our patient, for SCC of esophagus, in view of the advanced disease, palliative chemotherapy was given. He initially responded well, with subjective and objective tumor response. However, a month after completion of six cycles of first-line chemotherapy, disease progression occurred, necessitating second-line chemotherapy with weekly nanoxel. Weekly paclitaxel has shown benefit in the management of advanced unresectable esophageal and gastric carcinomas. In a study by Ilson et al., partial responses were seen in 13% (95% confidence interval (CI) 6-20%). In patients without prior chemotherapy, partial responses were seen in 15%, whereas in patients who had received prior chemotherapy, response was seen in 5%. The median duration of response was 172 days.[18]
In a study by Kato et al., weekly paclitaxel was studied in patients who had previously received platinum-based chemotherapy. The overall response rate was 44.2% and 7.7% achieved complete response. The median duration of response was 4.8 months, and median overall survival was 10.4 months.[19] In both the studies, weekly paclitaxel had a manageable toxicity profile. In our patients, following 8 weeks of therapy, imaging showed stable disease and our patient did not have any grade 3 or grade 4 toxicity.
Anatomical diagnosis
Multiple recurrent laryngeal papillomatosis with metastatic carcinoma esophagus
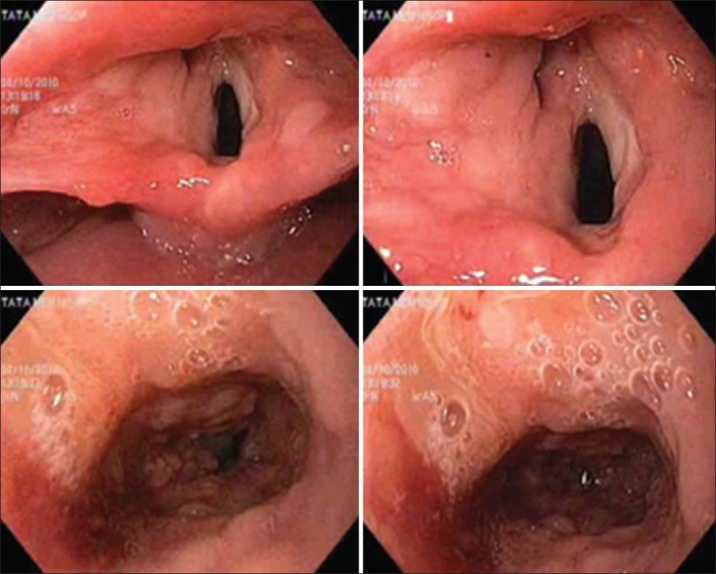
| Fig. 1 Multiple papillomas seen in the infraglottic region
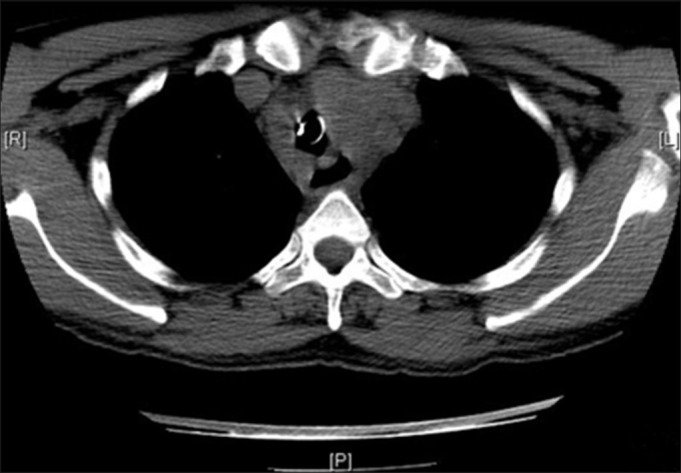
| Fig. 2 Computed tomography scan showing mediastinal lymphadenopath
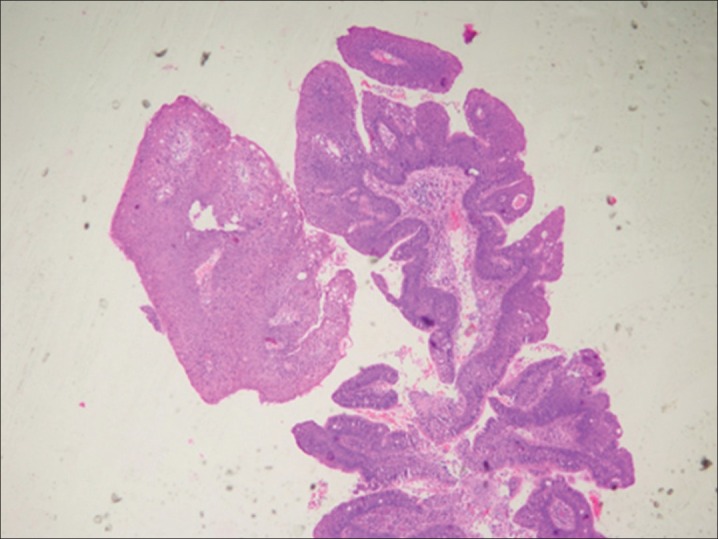
| Fig. 3 Slide of laryngeal papilloma
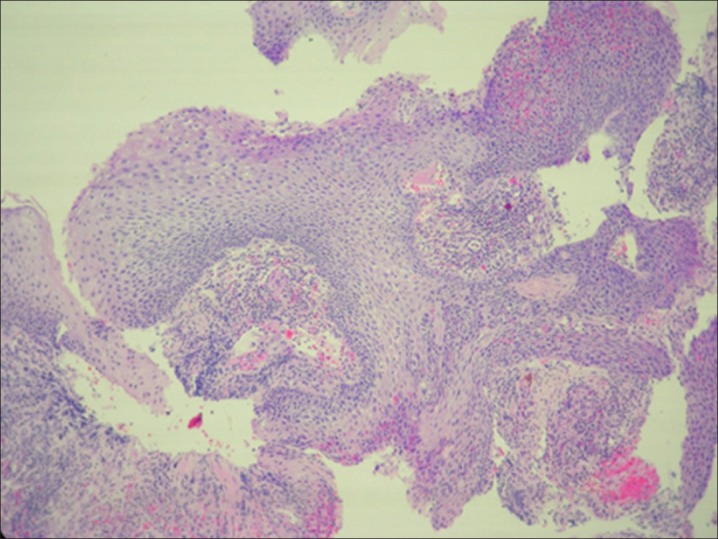
| Fig. 4 Slide of squamous carcinoma


 PDF
PDF  Views
Views  Share
Share

