Bowel Lymphoma in Children: Management and Outcome
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2018; 39(02): 184-187
DOI: DOI: 10.4103/ijmpo.ijmpo_94_17
Abstract
Background: Primary bowel lymphoma is an uncommon neoplasm in children and not well documented in literature with regard to its outcome and management. Materials and Methods: A case record review of children with bowel lymphoma was undertaken in a tertiary care institute, from 2010 to 2016 and the relevant data were recorded. Results: 21 children were managed with bowel lymphoma over a period of 7 years. Pain abdomen was the most common presenting symptom (19/21). Ileum was the site of involvement in most children (17/21). Localised disease was seen in 13/21 while 8 had diffuse involvement. Predominantly (13/21) children presented at an advanced stage (III/IV). Surgical intervention was needed in 14/21 while 7/21 were managed only with chemotherapy. Majority (15/21) had Burkitt's lymphoma on histology. 13 of 21 (61.9%) have completed chemotherapy and on regular follow up. Among 8 who died, 6 were directly related to disease progression despite aggressive management. Conclusion: Bowel lymphoma in children is distinctly different in the site of presentation from that of the adults. Advanced stage at presentation portends poor prognosis. Bowel lymphoma is to be considered in case of recurrent intussusception in children.
Publication History
Article published online:
23 June 2021
© 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Background: Primary bowel lymphoma is an uncommon neoplasm in children and not well documented in literature with regard to its outcome and management. Materials and Methods: A case record review of children with bowel lymphoma was undertaken in a tertiary care institute, from 2010 to 2016 and the relevant data were recorded. Results: 21 children were managed with bowel lymphoma over a period of 7 years. Pain abdomen was the most common presenting symptom (19/21). Ileum was the site of involvement in most children (17/21). Localised disease was seen in 13/21 while 8 had diffuse involvement. Predominantly (13/21) children presented at an advanced stage (III/IV). Surgical intervention was needed in 14/21 while 7/21 were managed only with chemotherapy. Majority (15/21) had Burkitt's lymphoma on histology. 13 of 21 (61.9%) have completed chemotherapy and on regular follow up. Among 8 who died, 6 were directly related to disease progression despite aggressive management. Conclusion: Bowel lymphoma in children is distinctly different in the site of presentation from that of the adults. Advanced stage at presentation portends poor prognosis. Bowel lymphoma is to be considered in case of recurrent intussusception in children.
Keywords
Bowel lymphoma - Burkitt's lymphoma - childhood malignancies - non-Hodgkin's lymphomaIntroduction
The pediatric population constitutes 32.4% of the total population of India and malignancy is an emerging major childhood killer.[1] Primary tumors of the gastrointestinal (GI) tract are rare in children and represent <5 href="https://www.thieme-connect.com/products/ejournals/html/10.4103/ijmpo.ijmpo_94_17#JR_2" xss=removed>2] The scarcity of the disease and variable clinical presentation preclude early diagnosis when the likelihood of cure exists.
Among GI malignancies, non-Hodgkin's lymphoma (NHL), especially Burkitt's lymphoma (BL) is the predominant variety.[3] In children, Paediatric gastrointestinal tract lymphoma (PGTLs) tend to occur in the small and large intestines, as opposed to the stomach in adults.[3]
Although lymphoma is the most common pediatric GI malignancy, there are not many studies available in the literature. The study documents the experience of pediatric bowel lymphomas in a tertiary care institute.
Objective
-
To evaluate the clinical presentation of pediatric GI lymphoma
-
To determine the prognosis and prognostic factors of pediatric GI lymphoma.
Materials and Methods
It is a retrospective plus prospective study of GI lymphomas in pediatric age group presented to Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, over a period of 7 years (2010–2016). Patient demography, history, examination, investigations, treatment, and follow-up were recorded.
Dawson et al.'s [4] criteria were used to differentiate primary from secondary bowel lymphoma. The tumor was considered primary when there is no superficial adenopathy at diagnosis, no mediastinal adenopathy at chest radiography, normal blood cell counts, no involvement of liver and spleen, and involvement of only regional lymph nodes at laparotomy.
St Jude's Staging system [5] was used to stage the disease.
Investigations to complete the workup included ultrasonogram, computed tomography [Figure 1], biopsy of mass, bone scan, and bone marrow biopsy.

| Figure.1
LMB-96 chemotherapy protocol [Figure 2] was used for treating patients. Progressive disease patients received additional rituximab, ifosfamide, carboplatin, etoposide regimen. Surgery was reserved for residual tumor and complications of mass.
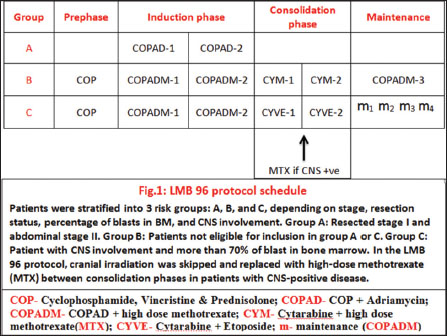
| Figure.2
Numerical data were expressed in mean ± standard deviation and range. Fisher's exact t-test was used to find a difference between two groups and Chi-square test was used to find a difference between three or more groups. P < 0>
Results
A total of 21 patients were found during the study period. Mean age was 6.05 ± 3.34 years with 14 (66.67%) patients aged ≤5 years. The smallest patient was aged 3 years while the eldest was 14 years. Males were more commonly affected (7:1). Pain abdomen was the most common presentation (90.5%), followed by distension of abdomen (85.7%) [Table 1].
|
Presentation |
n (%) |
|---|---|
|
Pain abdomen |
19 (90.5) |
|
Distension |
18 (85.7) |
|
Vomiting |
11 (52.4) |
|
Mass per abdomen |
14 (66.7) |
|
Intussusception |
3 (14.3) |
|
Blood in stools |
2 (9.5) |
|
Constipation |
1 (4.7) |
|
Intestinal obstruction |
10 (47.6) |

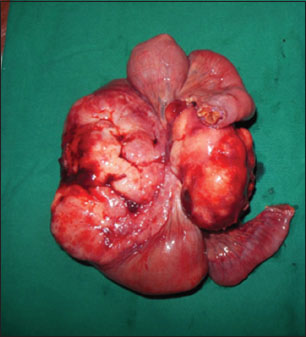
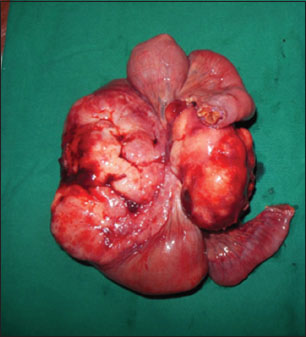
| Figure.3
Most common site of involvement was terminal ileum (81%) [Table 2]. Thirteen (61.9%) patients had localized disease while 8 (38.1%) patients had diffuse disease at presentation. Eight (38.1%) cases belonged to Stage II of St. Jude's system of classification, 7 (33.3%) belonged to Stage III, and 6 (28.6%) belonged to Stage IV. Eighteen (85.7%) patients had primary GI lymphoma whereas 3 (14.3%) had secondary GI lymphoma.
|
Site of involvement |
n (%) |
|---|---|
|
DJ – Duodenojejunal |
|
|
Terminal ileum |
17 (81) |
|
DJ junction |
1 (4.7) |
|
Jejunoileal |
2 (9.5) |
|
Ileocolic |
5 (23.8) |
| Figure.4
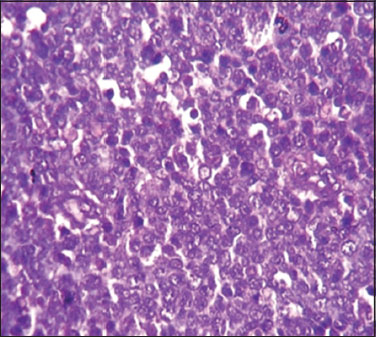
Histopathology [Figure 5] revealed 15 (71.4%) BL and 6 (28.6%) diffuse large B-cell lymphoma.
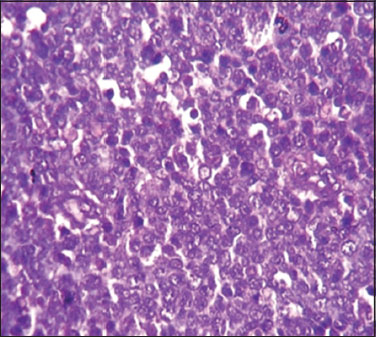
| Figure.5
Thirteen (61.9%)-patients completed chemotherapy and on follow-up ranging from 1 to 6 years with no evidence of recurrence. One patient is currently undergoing chemotherapy. There were 8 mortalities (38.1%)-in our study. All succumbed during chemotherapy; 6 patients due to progressive disease, one due to uncontrolled sepsis, and the other due to a complication of central venous access.
Stage of the disease (P - 0.0068) and diffuse disease at presentation (P - 0.0176) were found to be associated significantly with increased mortality whereas age, sex, site of involvement, primary/secondary disease, surgical intervention, and histopathology did not show statistically different outcome [Table 3].
|
Parameter |
n |
Death |
Percentage |
Fisher’s exact test (P) |
|---|---|---|---|---|
|
DLBCL – Diffuse large B‑cell lymphoma; BL – Burkitt’s lymphoma |
||||
|
Age (years) |
||||
|
≤5 |
14 |
7 |
50 |
0.173581 |
|
>5 |
7 |
1 |
14.28 |
|
|
Male |
18 |
8 |
44.44 |
0.257143 |
|
Female |
3 |
0 |
0 |
|
|
Stage II |
8 |
0 |
0 |
0.006841 |
|
Stage III and IV |
13 |
8 |
61.54 |
|
|
Localized |
13 |
2 |
15.38 |
0.017573 |
|
Diffuse |
8 |
6 |
75.00 |
|
|
Primary |
18 |
6 |
33.33 |
1.000000 |
|
Secondary |
3 |
2 |
66.67 |
|
|
Small bowel |
15 |
5 |
33.33 |
X2=1.7769 |
|
Large bowel |
1 |
1 |
100.00 |
P=0.411288 |
|
Both |
5 |
2 |
50.00 |
|
|
Resection and anastomosis |
9 |
2 |
22.22 |
X2=3.5979 |
|
Diversion |
3 |
1 |
33.33 |
P=0.308287 |
|
Biopsy |
1 |
1 |
100.00 |
|
|
No surgery |
7 |
4 |
57.14 |
|
|
BL |
15 |
6 |
40.00 |
1.000000 |
|
DLBCL |
6 |
2 |
33.33 |
|

| Figure.1
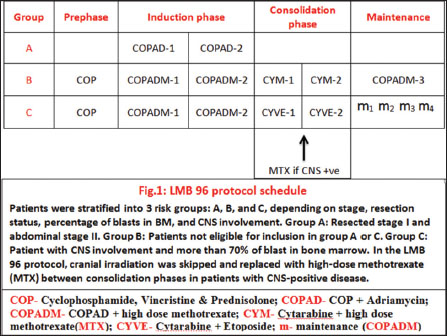
| Figure.2

| Figure.3
| Figure.4
| Figure.5
References
- Niharika P, Mobarak AK, Epari SR, Rama MR. Paediatric malignancies. J Clin Diagn Res 2012; 6: 674-7
- Bandyopadhyay R, Sinha SK, Chatterjee U, Nag D, Mukhopadhyay S, Chowdhury SR. et al. Primary pediatric gastrointestinal lymphoma. Indian J Med Paediatr Oncol 2011; 32: 92-5
- Kassira N, Pedroso FE, Cheung MC, Koniaris LG, Sola JE. Primary gastrointestinal tract lymphoma in the pediatric patient: Review of 265 patients from the SEER registry. J Pediatr Surg 2011; 46: 1956-64
- Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract.Report of 37 cases with a study of factors influencing prognosis Neonatal. Br J Surg 1961; 49: 80-9
- Murphy SB. Classification, staging and end results of treatment of childhood non-Hodgkin's lymphomas: Dissimilarities from lymphomas in adults. Semin Oncol 1980; 7: 332-9
- Morsi A, Abd El-Ghani Ael-G, El-Shafiey M, Fawzy M, Ismail H, Monir M. et al. Clinico-pathological features and outcome of management of pediatric gastrointestinal lymphoma. J Egypt Natl Canc Inst 2005; 17: 251-9
- Bethel CA, Bhattacharyya N, Hutchinson C, Ruymann F, Cooney DR. Alimentary tract malignancies in children. J Pediatr Surg 1997; 32: 1004-8
- Skinner MA, Plumley DA, Grosfeld JL, Rescorla FJ, West KW, Scherer LR. et al. Gastrointestinal tumors in children: An analysis of 39 cases. Ann Surg Oncol 1994; 1: 283-9
- Raina V, Sharma A, Vora A, Shukla NK, Deo SV, Dawar R. et al. Primary gastrointestinal non Hodgkin's lymphoma chemotherapy alone an effective treatment modality: Experience from a single Centre in India. Indian J Cancer 2006; 43: 30-5


 PDF
PDF  Views
Views  Share
Share

