B-Acute Lymphoblastic Leukemia in a Follow-up Case of Breast Cancer
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2020; 41(01): 99-101
DOI: DOI: 10.4103/ijmpo.ijmpo_16_19
Sir,
Therapy-related leukemias are a well-known complication of the treatment of solid or hematological malignancies. Among solid malignancies, breast cancer is the most common cause of therapy-related leukemias. Therapy-related leukemias usually present within 5?7 years of the primary treatment. The majority of these leukemias are of the myeloid lineage, but therapy-related acute lymphoblastic leukemia (t-ALL) has been rarely described. Because of the rarity, the clinical and molecular markers have been poorly described in t-ALL. Hence, we report a case of B-acute lymphoblastic leukemia (ALL) developing in a patient of carcinoma breast on follow-up.
Publication History
Received: 23 January 2019
Accepted: 06 October 2019
Article published online:
23 May 2021
? 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Sir,
Therapy-related leukemias are a well-known complication of the treatment of solid or hematological malignancies. Among solid malignancies, breast cancer is the most common cause of therapy-related leukemias. Therapy-related leukemias usually present within 5?7 years of the primary treatment. The majority of these leukemias are of the myeloid lineage, but therapy-related acute lymphoblastic leukemia (t-ALL) has been rarely described. Because of the rarity, the clinical and molecular markers have been poorly described in t-ALL. Hence, we report a case of B-acute lymphoblastic leukemia (ALL) developing in a patient of carcinoma breast on follow-up.
Case Report
We report a case of 40-year-old female, who was diagnosed with breast cancer, Stage IIIA (AJCC 7th?edition) with a hormonal profile of ER+ (8/8)/PR+ (6/8)/Her2?. She received standard adjuvant chemotherapy with 4#FEC (5-fluorouracil - 600 mg/m2, epirubicin - 75 mg/m2, cyclophosphamide - 600 mg/m2) and 4#Docetaxel (85 mg/m2). After completion of chemotherapy, she underwent chest wall radiation 50 Gray/25#/5 weeks. Along with radiotherapy, she was started on hormone therapy with tamoxifen. She completed her radiotherapy in August 2014 and after which was on regular follow-up with annual gynecology examination and mammogram.
She presented to us at the end of September 2018 with complaints of easy fatigability and generalized weakness. On clinical examination, she was pale with multiple, bilateral, level 2?3 cervical lymph nodes with hepatosplenomegaly (liver-4 cm and spleen-6 cm below the costal margin).
On further evaluation, she had pancytopenia with suppression of all hematopoietic lineages. Her bone marrow aspiration repeatedly showed dry tap, and her bone marrow flow cytometry could not be done despite multiple attempts. However, bone her bone marrow biopsy showed large areas of fibrosis with immature cells (blasts) suggestive of B-ALL with CD20+, TDT+ [Figure 1]. With a final diagnosis of B-ALL, she was started on B-ALL (AYA) protocol with a further aim of HLA-Matched Allogenic Stem Cell Transplant. At present, she has completed the induction phase and her postinduction bone marrow examination is in complete remission.
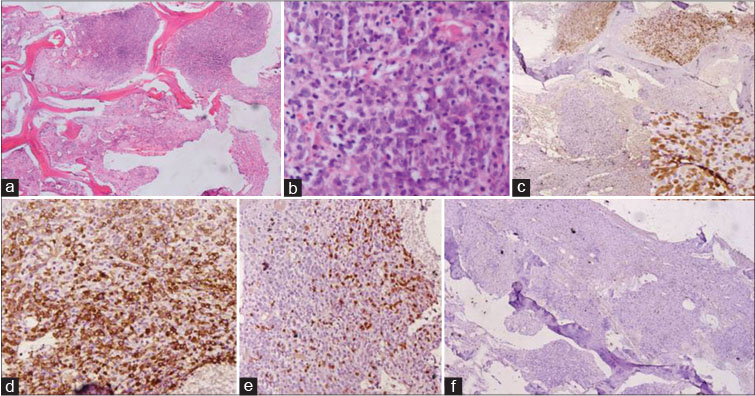
|?Fig. 1: (a) Microphotograph shows bone marrow biopsy with large areas of fibrosis. (b) The well preserved space shows immature cells (blasts). The cell are immunopositive for TDT ([c] ?200), CD20 ([d] ?200) while negative for CD3 ([e] ?200) and MPO ([f] ?100)
Discussion
Therapy-related leukemias are one of the known and rare complications of anticancer drugs. Out of myeloid and lymphoid series, most of the cases of secondary leukemia are reported to be acute myeloid leukemia/myelodysplastic syndromes. t-ALL are among one of the rare causes of ALL. The incidence of t-ALL is difficult to decipher as the results of larger studies have been confounded by the inclusion of secondary ALL (s-ALL) [Table 1]. In most of the studies, both t-ALL and s-ALL account for <1.5%?2.5?ses of ALL[5] [6]
Out of all anticancer drugs, alk?ylating agents and topoisomerase inhibitors are the most common drugs to be associated with therapy-related hematological malignancies. Therapy-related myeloid neoplasms have been reported to occur with a latency of 5?7 years with alkylating agents and 1?3 years with topoisomerase II inhibitors.[7]
In the recent study by Aldoss?et al.,[1] the median time to develop t-ALL was 6.8 years. Breast cancer was the most common primary malignancy reported in their cohort. In their retrospective cohort, 83% of the patients had available molecular markers, and the most common abnormality was Philadelphia (Ph) chromosome, followed by normal karyotype and mixed-lineage leukemia (MLL) gene rearrangement.
Our patient presented within 5 years of chemotherapy. She presented with typical symptoms of acute leukemia leading to symptoms of bone marrow failure. We could not identify any molecular abnormality of polymerase chain reaction and karyotyping studies because of the dry tap on bone marrow aspiration. This also raises a question of whether it was a therapy-related leukemia or an incidental finding of a breast cancer patient developing leukemia on follow up.
Therapy-related leukemias are biologically different from?de novo?ALL in terms of the clinical and molecular findings. The most consistent finding which has been reported among various series is the presence of molecular markers.[4] [8] The most consistent and common molecular markers associated with t-ALL are the presence of Ph chromosome and MLL gene rearrangement [Table 1].
It is difficult to arrive at a firm conclusion regarding the prognosis of patients with t-ALL because of the rarity of cases, but previous studies have reported t-ALL has a poor prognosis. Because of rarity, clinicians struggle to define a standard leukemia protocol, and the role of stem cell transplant has not been defined clearly.
According to the literature, data are sparse regarding ALL occurring as a therapy-related leukemia in a follow-up case of breast cancer. We could find only one case series of five patients published from India.[9] In which of five patients, only one had t-ALL. Hence, we report this case to increase the awareness of the same and the need for a high index of suspicion and the importance of regular follow-up even after remission of the primary malignancy.
The large scale database search is required to know the exact incidence and the outcomes of patients with t-ALL in Indian patients.
Conflict of Interest
There are no conflicts of interest.
References
- Aldoss I, Stiller T, Tsai NC, Song JY, Cao T, Bandara NA. et al.?Therapy-related acute lymphoblastic leukemia has distinct clinical and cytogenetic features compared to de novo acute lymphoblastic leukemia, but outcomes are comparable in transplanted patients. Haematologica 2018; 103: 1662-8
- Rosenberg AS, Brunson A, Paulus JK, Tuscano J, Wun T, Keegan TH. et al.?Secondary acute lymphoblastic leukemia is a distinct clinical entity with prognostic significance. Blood Cancer J 2017; 7: e605
- Abdulwahab A, Sykes J, Kamel-Reid S, Chang H, Brandwein JM.?Therapy-related acute lymphoblastic leukemia is more frequent than previously recognized and has a poor prognosis. Cancer 2012; 118: 3962-7
- Shivakumar R, Tan W, Wilding GE, Wang ES, Wetzler M.?Biologic features and treatment outcome of secondary acute lymphoblastic leukemia ? A review of 101 cases. Ann Oncol 2008; 19: 1634-8
- Pagano L, Pulsoni A, Mele L, Leone G.?Clinical and epidemiological features of acute lymphoblastic leukemia following a previous malignancy. Leuk Lymphoma 2000; 39: 465-75
- Ishizawa S, Slovak ML, Popplewell L, Bedell V, Wrede JE, Carter NH. et al.?High frequency of pro-B acute lymphoblastic leukemia in adults with secondary leukemia with 11q23 abnormalities. Leukemia 2003; 17: 1091-5
- Hawkins MM, Wilson LM, Stovall MA, Marsden HB, Potok MH, Kingston JE. et al.?Epipodophyllotoxins, alkylating agents, and radiation and risk of secondary leukaemia after childhood cancer. BMJ 1992; 304: 951-8
- Tang G, Zuo Z, Thomas DA, Lin P, Liu D, Hu Y. et al.?Precursor B-acute lymphoblastic leukemia occurring in patients with a history of prior malignancies: Is it therapy-related?. Haematologica 2012; 97: 919-25
- Bhatia P, Das R, Ahluwalia J, Malhotra P, Varma N, Varma S. et al.?Acute leukemia/myelodysplastic syndrome as a sequelae of carcinoma breast: A report of five cases from North India. Indian J Pathol Microbiol 2009; 52: 167-70
Address for correspondence
Publication History
Received: 23 January 2019
Accepted: 06 October 2019
Article published online:
23 May 2021
? 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
References
- 1?Aldoss I, Stiller T, Tsai NC, Song JY, Cao T, Bandara NA. et al.?Therapy-related acute lymphoblastic leukemia has distinct clinical and cytogenetic features compared to de novo acute lymphoblastic leukemia, but outcomes are comparable in transplanted patients. Haematologica 2018; 103: 1662-8
- 2?Rosenberg AS, Brunson A, Paulus JK, Tuscano J, Wun T, Keegan TH. et al.?Secondary acute lymphoblastic leukemia is a distinct clinical entity with prognostic significance. Blood Cancer J 2017; 7: e605
- 3?Abdulwahab A, Sykes J, Kamel-Reid S, Chang H, Brandwein JM.?Therapy-related acute lymphoblastic leukemia is more frequent than previously recognized and has a poor prognosis. Cancer 2012; 118: 3962-7
- 4?Shivakumar R, Tan W, Wilding GE, Wang ES, Wetzler M.?Biologic features and treatment outcome of secondary acute lymphoblastic leukemia ? A review of 101 cases. Ann Oncol 2008; 19: 1634-8
- 5?Pagano L, Pulsoni A, Mele L, Leone G.?Clinical and epidemiological features of acute lymphoblastic leukemia following a previous malignancy. Leuk Lymphoma 2000; 39: 465-75
- 6?Ishizawa S, Slovak ML, Popplewell L, Bedell V, Wrede JE, Carter NH. et al.?High frequency of pro-B acute lymphoblastic leukemia in adults with secondary leukemia with 11q23 abnormalities. Leukemia 2003; 17: 1091-5
- 7?Hawkins MM, Wilson LM, Stovall MA, Marsden HB, Potok MH, Kingston JE. et al.?Epipodophyllotoxins, alkylating agents, and radiation and risk of secondary leukaemia after childhood cancer. BMJ 1992; 304: 951-8
- 8?Tang G, Zuo Z, Thomas DA, Lin P, Liu D, Hu Y. et al.?Precursor B-acute lymphoblastic leukemia occurring in patients with a history of prior malignancies: Is it therapy-related?. Haematologica 2012; 97: 919-25
- 9?Bhatia P, Das R, Ahluwalia J, Malhotra P, Varma N, Varma S. et al.?Acute leukemia/myelodysplastic syndrome as a sequelae of carcinoma breast: A report of five cases from North India. Indian J Pathol Microbiol 2009; 52: 167-70


 PDF
PDF  Views
Views  Share
Share

