Angiosarcoma of the scalp associated with Xeroderma pigmentosum
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2012; 33(02): 126-129
DOI: DOI: 10.4103/0971-5851.99753
Abstract
Xeroderma pigmentosum (XP) is a rare autosomal recessive genodermatosis associated with hypersensitivity to ultraviolet light due to defects in Deoxyribonucleic acid (DNA) repair. These patients have more than a 1000-fold increased risk of developing skin cancers. Although multiple cutaneous malignancies are common, the simultaneous occurrence of angiosarcoma and basal cell carcinoma is a rare phenomenon. We report a case of a 25-year-old male with XP with angiosarcoma scalp and basal cell carcinoma of face and occiput and discuss the treatment of this aggressive neoplasm with a review of the literature pertaining to it.
Publication History
Article published online:
13 April 2022
© 2012. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Xeroderma pigmentosum (XP) is a rare autosomal recessive genodermatosis associated with hypersensitivity to ultraviolet light due to defects in Deoxyribonucleic acid (DNA) repair. These patients have more than a 1000-fold increased risk of developing skin cancers. Although multiple cutaneous malignancies are common, the simultaneous occurrence of angiosarcoma and basal cell carcinoma is a rare phenomenon. We report a case of a 25-year-old male with XP with angiosarcoma scalp and basal cell carcinoma of face and occiput and discuss the treatment of this aggressive neoplasm with a review of the literature pertaining to it.
INTRODUCTION
Xeroderma pigmentosum (XP) is a rare autosomal recessive genodermatosis characterized by hypersensitivity to ultraviolet (UV) light affecting the cutaneous, ocular and nervous systems. It results due to a defect in the nucleotide excision repair mechanism, which is involved in DNA repair following UV irradiation. Defect in these genes leads to build up of unrepaired DNA damage which is responsible for a majority of the features of XP. There is a 1000-fold increased risk of development of cutaneous and 10-20-fold increased risk of developing non-cutaneous malignancies.
CASE REPORT
A 25-year-old male, known case of XP, presented with a non-healing bleeding ulcer over the scalp following a minor trauma of 9 months duration. In addition, he had two other lesions below the left eyelid and the right occipital region of 4 months duration. He had a history of prior surgery done for a lower lip lesion (squamous cell carcinoma) and for two lesions over the scalp (myoepithelial carcinoma of dermis, benign skin adnexal tumor of hair follicle differentiation). Two of his 2nd- and 3rd-degree relatives on the maternal side had a history of XP. There was no history of consanguinity present in the family.
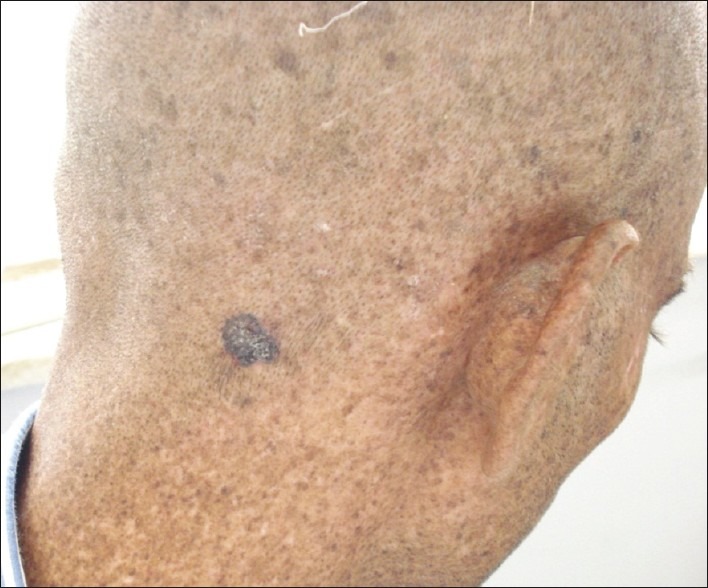
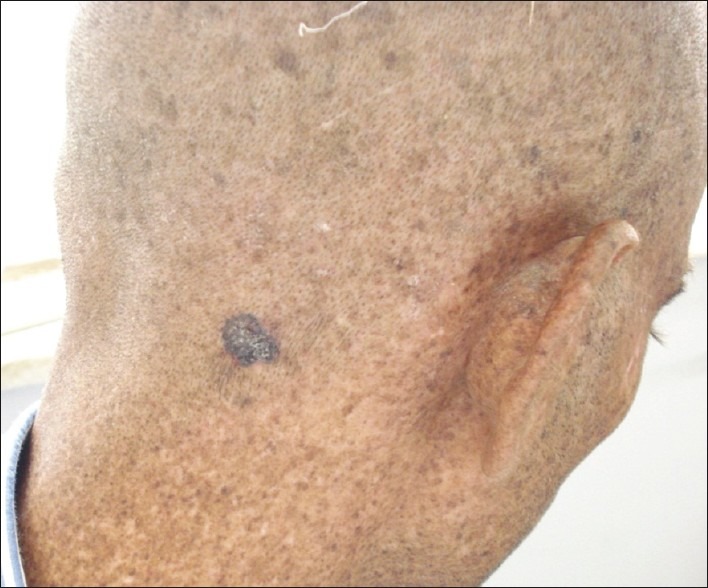
On examination all three lesions were distinctly different. There was a 10 cm×5 cm ulcer with irregular, rolled out edges over the frontoparietal region of the scalp [Figure 1]. The underlying bone was clinically eroded. The lesion over the right occipital region was a 2 cm×2 cm hyperpigmented macule and that below the left eyelid was a 1.0 cm×0.50 cm hyperpigmented papule [Figures [Figures22 and and3].3]. Classical stigmata of XP with dry atrophic skin and patchy hyperpigmentation were present all over the body. Detailed neurological and ophthalmological examination revealed no abnormality. In view of the high index of suspicion of malignancy biopsies from all three sites were taken and sent for histopathological examination.

| Fig. 1 Angiosarcoma of the scalp in a 25-year-old patient of Xeroderma pigmentosum with skin atrophy and patchy hyperpigmentation

| Fig. 2 Basal cell carcinoma in the same patient. Arrow pointing towards lesion
| Fig. 3 Basal cell carcinoma of the occipital region in the same patient
Biopsy from the scalp lesion revealed disordered proliferation of atypical endothelial cells with hyperchromatic markedly pleomorphic nuclei and eosinophilic cytoplasm. Small vascular channels with red blood cells were seen lined by similar cells dissecting through the dermis and around the adnexal structure [Figure 4]. Tumor cells expressed Clusters of differentiation (CD) 34 and CD31, and were negative for cytokeratin [Figure 5]. These histological findings were suggestive of poorly differentiated angiosarcoma. Biopsies from the occipital region and face were consistent with basal cell carcinoma.
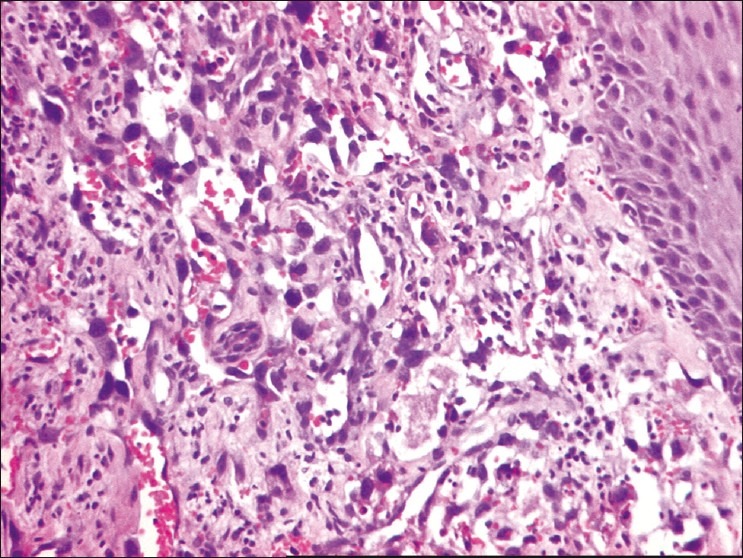
| Fig. 4 Scalp angiosarcoma. Pleomorphic malignant cells forming inter-anastomosing vascular channels beneath the epidermis (hematoxylin and eosin; original magnification ×200)
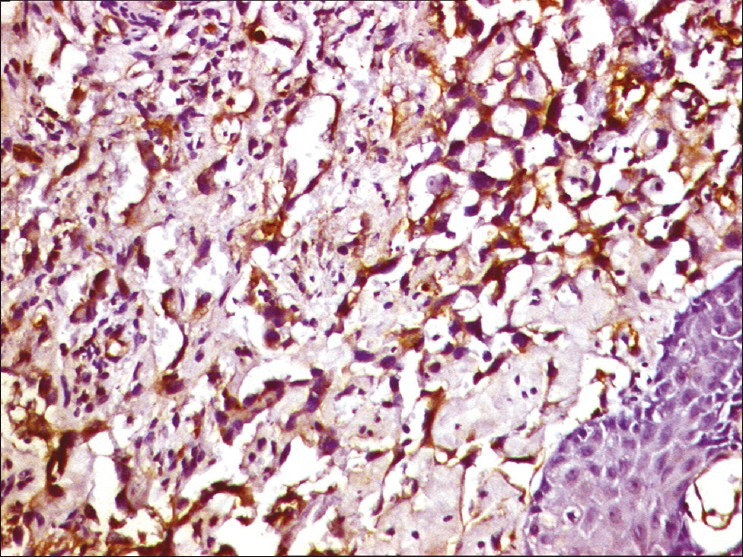
| Fig. 5 Tumor cells express vascular antigen CD31 on immunohistochemistry. (Indirect immunoperioxidase; original magnification ×200)
Computed tomographic scan of the skull showed erosion of both outer and inner table of the frontal and parietal bones. Whole body positron emission tomography scan was performed which ruled out distant metastasis. Megnatic resonance venogram revealed tumor invading the superior sagittal sinus [Figure 6].
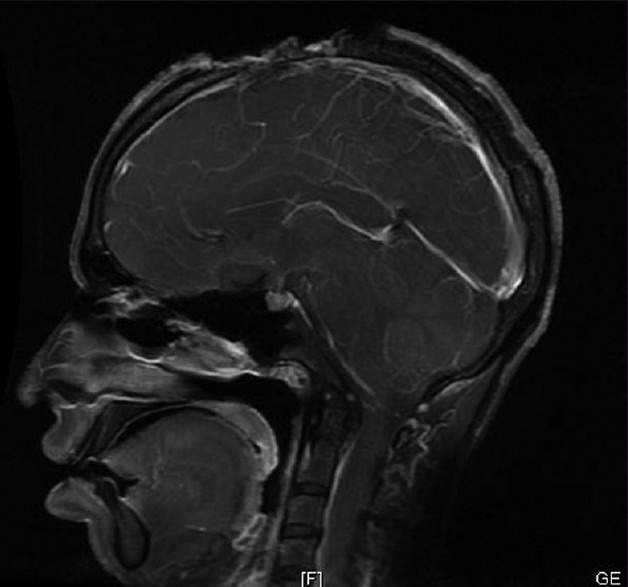
| Fig. 6 Magnatic resonance Venogram showing tumor invading the superior sagittal sinus
In view of unresectability due to the involvement of the superior sagittal sinus, the patient was not considered a candidate for surgery. Scalp lesion and occipital lesion were treated with external beam radiotherapy. Radiotherapy to the scalp in the doses of 72 Gy in 36 fractions was given. Face lesion was treated by interstitial brachytherapy at the doses of 35 Gy in 10 fractions. The patient was advised to adopt strict sun protection life style and was offered genetic counselling with blood DNA banking and instructed to come for regular follow-up.
DISCUSSION
We have presented a case of angiosarcoma in an XP patient. Majority of the lesions in XP patients are basal cell carcinoma and squamous cell carcinoma but rare aggressive neoplasms such as angiosarcomas may occur and, hence, should always be kept as a differential. Because of its rarity in XP and lack of clinical suspicion, the neoplastic ulcer was confused with post-traumatic, infected ulcer in this patient and diagnosis was delayed outside for 9 months and no biopsy was taken. As a result of which otherwise surgically resectable tumor became unresectable and the patient could be offered radiotherapy alone which is not the standard of care for this aggressive neoplasm. As XP patients are deficient in normal DNA repair mechanism, there is a possibility that they may develop extreme sensitivity to therapeutic radiation as well, further complicating the management in such patients. Thus a high index of suspicion is required to detect such aggressive neoplasms at the earliest. XP patients, carry a life-long risk of developing cutaneous and noncutaneous neoplasms. Squamous cell carcinomas, basal cell carcinomas and melanomas are commonly present but their association with angiosarcoma is rare. Only five such cases have been reported till now.[1–5]
The first case of cutaneous angiosarcoma complicating XP was described by Leake in 1992.[1] Angiosarcomas are rare malignant vascular tumors that comprise approximately 2% of all soft tissue sarcomas. Fifty percent of the angiosarcomas occur in the head and neck. Scalp and face are the most common sites of involvement.
Angiosarcoma generally affects the elderly male. The mean age of presentation is 60-70 years. However in XP patients it may occur at a younger age. Our patient as well as the previous four out of five reported cases of angiosarcoma in XP patients affected patients in the younger age group. Angiosarcoma in XP patients may develop as a result of the UV-induced damage or it may arise from the abnormal ectatic vessel from telengectetic lesion, commonly present in XP cases. However telengectesias were absent in our patient. There may be a history of prior trauma as in our case, but no causal relationship has been proven. Patients may present with macules resembling bruises, plaques, nodules and ulcers which bleed often. Diagnosis is often delayed because of a lack of clinical suspicion as happened in our case as well. Abnormal pleomorphic malignant endothelial cells forming interanastomosing vascular channels are the histological hallmark of angiosarcoma. Histologically, they can be divided into well-, moderate- and poorly differentiated tumors. Diagnosis is confirmed by Immunohistochemistry. CD31, CD 34, VonWillebrand factor and UEA 1 are the most useful endothelial markers. Of these CD31 is found to be the most sensitive endothelial marker.[6]
Angiosarcomas warrant an aggressive therapeutic approach. Wide surgical excision with negative margins combined with adjuvant radiotherapy is the treatment of choice. Adjuvant radiotherapy should include high dose (>50 Gray) with wide treatment fields so as to minimize recurrence. However, patients with XP are sensitive to environmental mutagens. Sensitivity to radiation at the clinical as well as cellular level has been demonstrated in XP patients.[7] Thus radiotherapy should be given in such patients with great caution. Chemotherapy in adjuvant and neoadjuvant settings has not been found to be effective. Unresectable cases are treated with radiotherapy. Some researchers advocate adding chemotherapy in unresectable cases, although chemotherapy has not been proven to be beneficial.[8,9] Recently some studies have reported favorable responses with taxane-based chemotherapy for angiosarcomas of the face and scalp.[10,11]
The prognosis for angiosarcomas is poor with the 5-year survival rate between 12 and 33%.[12,13] Size >10 cm and positive margins of resection are the most significant predictors of poor prognosis. Local recurrence and distant metastasis usually occur within 2 years of diagnosis. Lung followed by liver and spleen are the most common sites of metastasis.
CONCLUSION
XP is a disease with increased susceptibility to develop various malignant neoplasms. Squamous cell carcinoma and basal cell carcinoma are the most common. Occurrence of angiosarcoma is a rare phenomenon. Younger age of involvement in the absence of known risk factors combined with lack of clinical suspicion often results in a delay in diagnosis and patients present in advanced stage. As early diagnosis of this aggressive neoplasm will entail surgical excision with clear margins improving prognosis, lifelong close follow-up of XP patients and early biopsy of any suspicious lesion is essential. XP patients have increased chances of receiving radiotherapy due to development of multiple malignancies therefore it is important to determine the degree of radiosensitivity in this syndrome. Radiotherapy should be used with caution.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES

| Fig. 1 Angiosarcoma of the scalp in a 25-year-old patient of Xeroderma pigmentosum with skin atrophy and patchy hyperpigmentation

| Fig. 2 Basal cell carcinoma in the same patient. Arrow pointing towards lesion
| Fig. 3 Basal cell carcinoma of the occipital region in the same patient
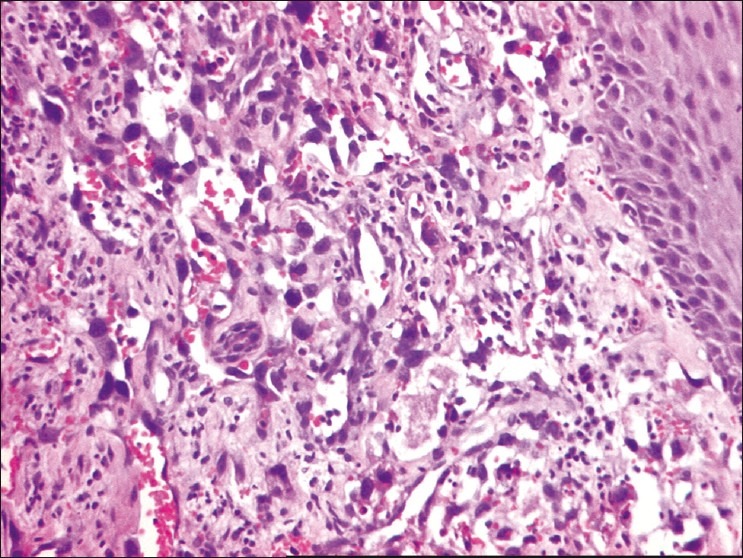
| Fig. 4 Scalp angiosarcoma. Pleomorphic malignant cells forming inter-anastomosing vascular channels beneath the epidermis (hematoxylin and eosin; original magnification ×200)
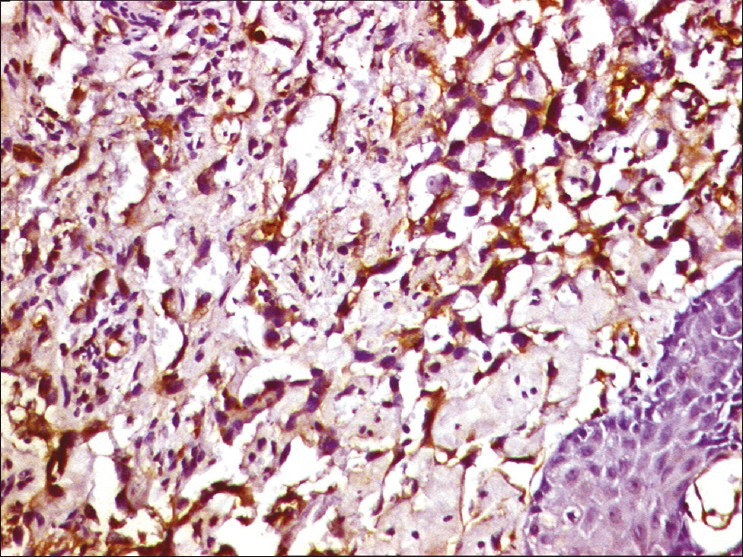
| Fig. 5 Tumor cells express vascular antigen CD31 on immunohistochemistry. (Indirect immunoperioxidase; original magnification ×200)
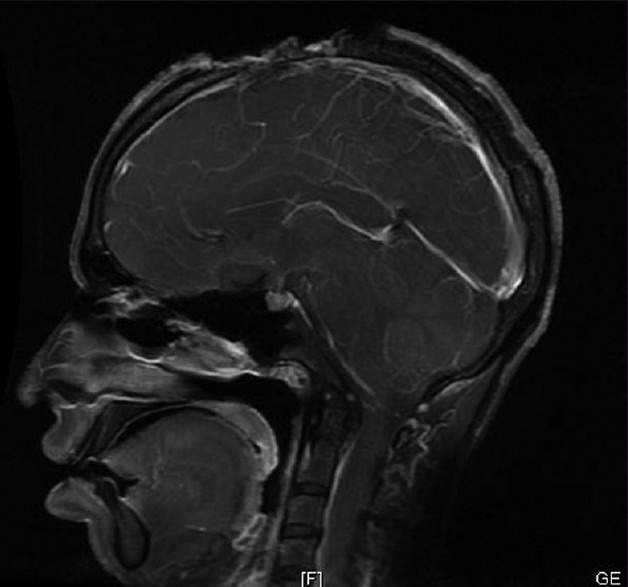
| Fig. 6 Magnatic resonance Venogram showing tumor invading the superior sagittal sinus


 PDF
PDF  Views
Views  Share
Share

