An Exasperating and Unusual Presentation of Buschke-Lowenstein Tumor in an Adolescent Girl: Case Report with Review of Literature
CC BY 4.0 · Indian J Med Paediatr Oncol 2025; 46(02): 226-230
DOI: DOI: 10.1055/s-0044-1788312
Abstract
Giant condylomata acuminata of Buschke-Löwenstein (GCBL) is a benign condition with a high recurrence rate and a remote possibility of developing into cancer. It is characterized by excessive proliferation of verrucous lesions on the genitalia and/or perianal region, and is frequently linked to human papillomavirus (HPV) subtypes 6 and 11. With the exception of a few case series, case reports make up the majority of the literature. Despite the literature's support for surgical excision, the current evaluation reveals a lack of clarity regarding the disease's diagnosis and best course of action. Better assessment and management of these patients are necessary to prevent any progression/recurrence of disease.
Here, we present a case of a GCBL of the vulva in an 18-year-old girl, who was effectively treated with a simple vulvectomy and split skin graft reconstruction. The reported case is one of the rarest presentations of Buschke-Löwenstein tumor as it is not associated with any of the HPV subtypes and is seen in an 18-year-old girl, one of the youngest patients reported till date. This case report is followed by a brief review of the literature on GCBL, which will add to our understanding of this entity and the most effective therapy to treat the disease.
Keywords
giant condylomata acuminata - Buschke-Löwenstein tumor - human papillomavirus - adolescent - verrucous hyperplasia
Patient's Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity.
Publication History
Article published online:
18 July 2024
© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Buschke-Löwenstein Anal Tumour in Children: Two Case ReportsA. Schneider, European Journal of Pediatric Surgery, 2009
- Buschke-Löwenstein Anal Tumour in Children: Two Case ReportsA. Schneider, European Journal of Pediatric Surgery, 2009
- Buschke-Lowenstein tumor in a patient with HIV and PsoriasisJosé Antonio Dias da Cunha e Silva, Journal of Coloproctology, 2020
- Difficulties of diagnosis and treatment in giant condyloma of Buschke and Löwenstein (GCBL) which led to fatal outcome in a womanG. Kovács, Zeitschrift für Gastroenterologie, 2004
- Successfully treated patient with verrucous carcinoma developed from anogenital giant condylomaD Kári, Zeitschrift für Gastroenterologie, 2009
- Advances in the applications of CRISPR/Cas system for tumor molecular diagnostics<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- OVERCOMING STRESS DURING COVID-19<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- New mouse genetic model of breast cancer from IKKα defects in dendritic cells revealed by single-cell RNA sequencing<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Identification of Proteins and Genes Associated with Hedgehog Signaling Pathway Involved in Neoplasm Formation Using Text-Mining Approach<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Author Correction: A single-cell atlas of liver metastases of colorectal cancer reveals reprogramming of the tumor microenvironment in response to preoperative ...<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
Abstract
Giant condylomata acuminata of Buschke-Löwenstein (GCBL) is a benign condition with a high recurrence rate and a remote possibility of developing into cancer. It is characterized by excessive proliferation of verrucous lesions on the genitalia and/or perianal region, and is frequently linked to human papillomavirus (HPV) subtypes 6 and 11. With the exception of a few case series, case reports make up the majority of the literature. Despite the literature's support for surgical excision, the current evaluation reveals a lack of clarity regarding the disease's diagnosis and best course of action. Better assessment and management of these patients are necessary to prevent any progression/recurrence of disease.
Here, we present a case of a GCBL of the vulva in an 18-year-old girl, who was effectively treated with a simple vulvectomy and split skin graft reconstruction. The reported case is one of the rarest presentations of Buschke-Löwenstein tumor as it is not associated with any of the HPV subtypes and is seen in an 18-year-old girl, one of the youngest patients reported till date. This case report is followed by a brief review of the literature on GCBL, which will add to our understanding of this entity and the most effective therapy to treat the disease.
Keywords
giant condylomata acuminata - Buschke-Löwenstein tumor - human papillomavirus - adolescent - verrucous hyperplasia
Abstract
Giant condylomata acuminata of Buschke-Löwenstein (GCBL) is a benign condition with a high recurrence rate and a remote possibility of developing into cancer. It is characterized by excessive proliferation of verrucous lesions on the genitalia and/or perianal region, and is frequently linked to human papillomavirus (HPV) subtypes 6 and 11. With the exception of a few case series, case reports make up the majority of the literature. Despite the literature's support for surgical excision, the current evaluation reveals a lack of clarity regarding the disease's diagnosis and best course of action. Better assessment and management of these patients are necessary to prevent any progression/recurrence of disease.
Here, we present a case of a GCBL of the vulva in an 18-year-old girl, who was effectively treated with a simple vulvectomy and split skin graft reconstruction. The reported case is one of the rarest presentations of Buschke-Löwenstein tumor as it is not associated with any of the HPV subtypes and is seen in an 18-year-old girl, one of the youngest patients reported till date. This case report is followed by a brief review of the literature on GCBL, which will add to our understanding of this entity and the most effective therapy to treat the disease.
Keywords
giant condylomata acuminata - Buschke-Löwenstein tumor - human papillomavirus - adolescent - verrucous hyperplasia
Introduction
Condyloma acuminatum, often known as venereal warts, is a common sexually transmitted infection that can affect both sexes.[1] Abraham Buschke and Loewenstein Ludwig published the first description of giant vulvar condyloma, often known as the Buschke-Lowenstein tumor (BLT), in 1925.[2] Giant condyloma acuminata (GCA) of Buschke-Löwenstein (GCBL) is a benign condition with a high recurrence rate and a remote possibility of developing into cancer. It is characterized by excessive proliferation of verrucous lesions on the genitalia and is frequently linked to human papillomavirus (HPV) subtypes 6 and 11.[3]
Due to the rarity of this condition, isolated case reports make up the majority of the literature. Data published till date are mere compilation of prior case reports and analysis of the features mentioned in them, which restricts our understanding of this entity and the most effective treatment.[4] Several therapeutic options have been discussed in case reports,[5] [6] but there are no strong recommendations or evidence for the optimal treatment of patients with GCBL. The goal of this review was to analyze prior research that outlines this disease's characteristics and provide guidance for treatment. Since GCA is resistant to chemotherapy and radiation therapy, curative treatment typically involves local radical excision. Here, we present a case of a GCBL of the vulva who was effectively treated with a simple vulvectomy and split skin graft reconstruction. This is one of the rarest presentations of BLT, as it is not associated with any of the HPV subtypes and is seen in an 18-year-old girl, one of the youngest patients reported till date.
Case Report
An 18-year-old girl presented in the outpatient department with warty growth in her vulval region for 1 year. The growth has been gradually increasing in size over the last 12 months. She was first evaluated in a peripheral hospital, where a biopsy of the mass was done and reported as verrucous hyperplasia in histopathology report. She was from a family with a low socioeconomic background. Upon clinical examination, she was found to be moderately built with a body mass index of 20.8, Eastern Cooperative Oncology Group 0, and mild pallor. Other systems were normal. No signs of any discomfort, mass, or free fluid were present in the abdomen. A large friable growth that involved both of her labia majora and extended anteriorly to the mons pubis and posteriorly to the perianal region was detected during a local examination of her genitalia. ([Fig. 1A]). On the thighs, perianal region, and labia minora, there were a few satellite lesions ([Fig. 1B]). The clitoris, urethra, and external anal sphincter were unaffected. The patient's HPV deoxyribonucleic acid (DNA) test, human immunodeficiency virus (HIV), hepatitis B surface antigen, and screening for sexually transmitted diseases (STDs) were negative. She denied any sexual contact in the past. The patient had not been vaccinated for HPV.
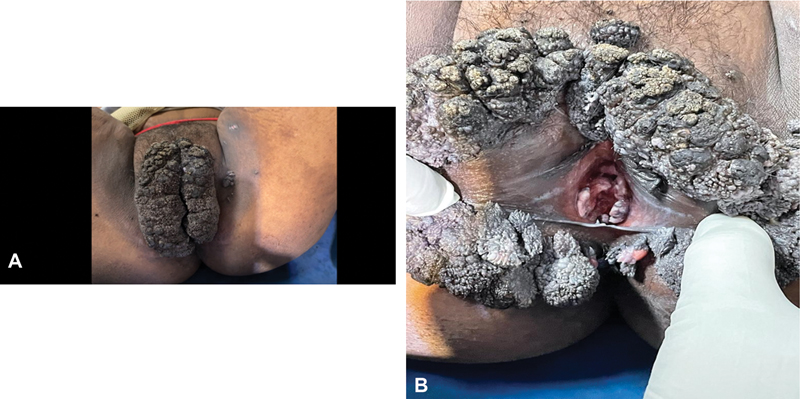
Fig 1: (A, B) Cauliflower-like growth that involved both of her labia majora and extended anteriorly to the mons pubis and posteriorly to the perianal region.
Simple vulvectomy with split skin graft reconstruction was planned after consultation with plastic surgeons. Simple vulvectomy was done ([Fig. 2A]). Vulval reconstruction was performed by harvesting grafts of intermediate thickness from the left thigh and placing them over the excision site ([Fig. 2B]). The plane of dissection was along the line of cleavage. Gross examination of the excised specimen showed a vulval excised flap of 13*9*4 cm with the skin surface showing wart-like growth. The satellite lesions on the thighs, perianal region, and labia minora were separately excised. Postoperative period was uneventful. The diagnosis of condyloma acuminatum with a moderate degree of dysplasia was confirmed by the final histopathology report ([Fig. 3]). Immunohistochemically, it was CD ⅚ positive, p63 positive, and p16 negative. Her functional outcome was good and was disease free even after 13 months postsurgery.
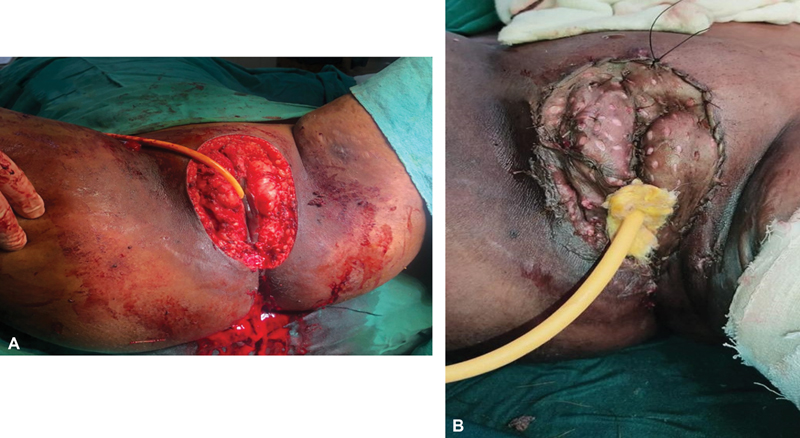
Fig 2 : (A, B) Intraoperative picture. (A) Simple vulvectomy. (B) Split skin grafting done over the defect.
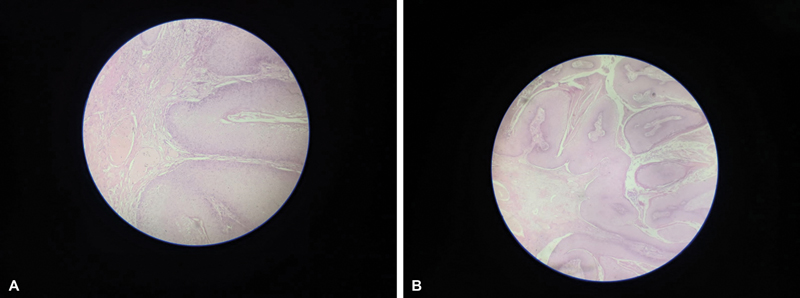
Fig 3 : (A, B) Histopathology image showing papillary proliferation of squamous epithelium with acanthosis and koilocytosis.
Discussion
The results of our analysis demonstrate the low quality of literature published till date. After going through the previous published data, certain trends have become apparent. We attempt to summarize what is currently known regarding these lesions.
Incidence
It is challenging to determine the precise incidence of GCBL due to the lack of standardized diagnostic criteria and the reporting of cases in isolation. However, an estimated prevalence rate of 0.1%. of the general population has been reported till date. The most common age group of presentation is 40 to 60 years. However, in our case, the age of presentation was only 18 years, which constitutes one of the youngest patients reported to date.[7]
Terminology
This uncommon tumor has been variously referred to as gigantic condyloma acuminata, condyloma acuminata with malignant transformation, squamous papillomatosis, and well-differentiated squamous cell carcinoma (SCC), suggesting that the terminology used to describe it is unclear.
A GCBL is a condyloma that exhibits destructive growth but not invasion. These lesions exhibit papillomatosis, parakeratosis, hyperkeratosis, acanthosis, and mild koilocytosis histologically. The cells' cytoplasm is vacuolized and they have big nuclei.[7] [8] Knoblich and Failing[9] discussed the correlations and contrasts between the clinical and histological aspects of classical condyloma acuminatum and giant condyloma acuminatum. The epithelium's orderly growth, thickening, infrequent appearance of mitotic figures in the spiny and basal layers, and regular maturation from the basal layer to the stratum corneum exhibiting parakeratosis and hyperkeratosis are among the similarities. Additionally, GCA differs from SCC, due to its ability to preserve polarity, an intact basement membrane, lack of lymphatic invasion, and lymph node metastases. Superficial plano-cellular carcinoma has been found as the underlying histology of some cases of gigantic condyloma.
Grading
Davis et al have suggested grading of the GCA.[10] The length of the total lesion (or lesions), as well as the diameter of each lesion's base are assessed for GCA grading. To determine the total size of the lesions, it is frequently helpful to measure each one by quadrant.
Grade
5 to 12 cm in total composite length with a base of < 2 cm or occupying > 1/3 the circumference of the penis, vaginal introitus, or anus.
> 12 cm in cumulative size or lesions with a base width of 2 to 3 cm.
> 12 cm or lesions with a base width greater than 3 cm, or any associated abscess or evidence of systemic infections.
Biopsy or excision exhibiting any invasive malignancy.
Risk Factors and Pathogenesis
The primary cause of GCA is HPV, which has been linked to subtypes 6 and 11 in more than 90%. of cases in both immunosuppressed patients and individuals with no other concomitant illnesses.[11] [12] Numerous subtypes have also been found in the same patient. However, in our case we did not find any association with any of the HPV subtypes. Patients with treatment-resistant genital warts and no discernible immunodeficiency have also been identified. Multiple sexual partners, persistent vaginal infections, bad hygiene, and immunocompromised conditions have all been linked to the condition.[4] [5] Despite the fact that 90%. of those infected with HPV will not get genital warts, but individuals who are afflicted can still spread the virus. The majority of HPV infections are successfully repelled by the immune system, which is linked to pronounced local cell-mediated immune responses. However, 10%. of people experience persistent infection, which increases their risk of becoming benign proliferative lesions, high-grade precursor lesions, and ultimately invasive cancers.[6]
These lesions are usually multiple and exhibit HPV DNA. But in our case, we did not find any association with HPV. It is important to thoroughly rule out conditions like epitheliomas, SCC, secondary syphilis, verrucous-vegetative tuberculosis, inguinal granuloma, and STDs like hepatitis B, hepatitis C, and HIV.[13] Due to a recurrence rate of 30 to 70%. that was discovered 6 months after drug administration, treatments for this STD are currently linked with limited efficacy.
Clinicopathological Presentation
In the vaginal or anorectal region, it manifests as a slowly expanding cauliflower-like tumor that infiltrates deeper tissues gradually.[14] The condyloma acuminatum can enlarge to sizes of more than 10 cm in diameter. It may take 2.8 to 9.6 years or longer from the onset of condyloma symptoms to the development of BLT.[15] Although tumor growth is typically moderate, immunocompromised people may experience faster tumor growth.[16] Although there is a chance of nonsexual transmission by fomites, condyloma acuminata and BLT in minors should always raise the possibility of sexual abuse, for which a thorough medical examination and detailed history is necessary.[16] Rapid growth and unusual clinical manifestations of BLT may indicate malignant transformation. Additionally, condyloma lesions can infrequently grow into substantial exophytic masses that can interfere with vaginal delivery, regular urine, and defecation. Patients also present with complaints of hemorrhoids, constipation, difficulty defecation, dysuria, difficulty urinating, abdominal bloating, and tiredness.[17] [18] Areas of benign condyloma may coexist with foci of atypical epithelial cells or well-differentiated SCC in a complicated histological pattern. GCA typically only affects the vaginal area; however, in a small percentage of instances, the tumor may also affect specific anorectal histology zones. Fistulae and abscesses may be seen as a result of the underlying tissue being infiltrated. Reports of extragenital GCA are considerably rare, prefer the folds, and their treatment with resection with disease-free margins is constrained by the potential for developing postsurgical contractures.[17]
Differential Diagnosis
Bowen's disease (dyskeratotic condyloma type), keratotic pseudoepitheliomatous balanitis, and SCC constitute some of its differential diagnosis.[19]
Treatment
Intralesional injection of 5-fluouracil (5-FU), topical chemotherapy (e.g., podophyllin, imiquimod, 5-FU, bleomycin), cryotherapy, interferon, carbon dioxide laser vaporization, curettage, resection alone or with neoadjuvant or adjuvant chemotherapy, radiation therapy, and chemotherapeutic drugs are some of the available treatment options available in the current era.[20] [21] These diverse therapeutic strategies, none of which is scientifically proven to be more effective than the other, highlight the disease's poorly established management and high rate of locoregional recurrences. The size, location, and previous unsuccessful treatments are just a few of the many things that need to be taken into account when choosing the best course of action for treatment. Microscopic examination of the genital tissues for subclinical HPV lesions is necessary for the prompt detection of recurrences and for choosing the optimal mode of management.[22]
Prior to surgery, imaging studies (such as computed tomography and magnetic resonance imaging) are necessary to determine the extent of the local and systemic disease and the best course of action. Although healing per secundum is seen as a better strategy since grafting poses a danger for HPV, wide local resections followed by skin grafts are still widely regarded as the mainstay of therapy.[23] After excision of GCBL, the whole affected genital area must be addressed since HPV is a field infection, where large areas of cells in a particular area are affected by the HPV. Currently, surgical intervention with negative margins is the gold standard and must be performed whenever feasible.[24] Although surgery predominates, there are reports of the successful management of BLT with medical therapy as well. Treatment is individual specific and cannot be generalized. Therefore, management of BLT should be left to the clinician's discretion.
Complications
The most frequent side effects of BLT are necrosis, fistulae, or superinfection.[20] Recurrences, soft tissue infiltration, and other complications such as fistulas, abscesses, bleeding from the surgical incision, soft tissue infection, flap failure, urinary infection, urethral obstruction, anal stenosis, and fecal incontinence are linked to the morbidity of GCBL patients.[4] Overall, mortality is 21%, and it is related to disease recurrences and associated morbidities.[18] Histology in cases of GCBL has no specific indicators for malignancy, such as lymphatic invasion, angioinvasion, basement membrane infiltration, or distant metastases. In 30 to 50%. of cases infiltration of the tumor base, bleeding, or nodal hypertrophy may raise suspicion of a malignant transition.[21]
Conclusion
The available evidence on Buschke-Lowenstein cancers is inconsistent and raises more issues than it answers. The current evaluation reveals a lack of clarity regarding the disease's diagnosis and best course of action. One step that will enable better analysis of this uncommon disease is the development of a multicentric registry and the establishment of a database to enable a more thorough evaluation, documentation, and study.
Conflict of Interest
None declared.
Acknowledgments
We thank Prof. Sushil Kumar Giri for his constant academic and moral support.
Patient's Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity.
References
- Niazy F, Rostami K, Motabar AR. Giant condyloma acuminatum of vulva frustrating treatment challenge. World J Plast Surg 2015; 4 (02) 159-162
- Koutsky L. Epidemiology of genital human papillomavirus infection. Am J Med 1997; 102 (5A): 3-8
- Steffen C. The men behind the eponym–Abraham Buschke and Ludwig Lowenstein: giant condyloma (Buschke-Loewenstein). Am J Dermatopathol 2006; 28 (06) 526-536
- Trottier H, Burchell AN. Epidemiology of mucosal human papillomavirus infection and associated diseases. Public Health Genomics 2009; 12 (5-6): 291-307
-
- Stanley M. Immune responses to human papillomavirus. Vaccine 2006; 24 (Suppl. 01) S16-S22
- von Krogh G, Lacey CJ, Gross G, Barrasso R, Schneider A. European course on HPV associated pathology: guidelines for primary care physicians for the diagnosis and management of anogenital warts. Sex Transm Infect 2000; 76 (03) 162-168
- Frei W. About carcinoma similar pointed condyloma on the penis. Arch Derm Syph 1930; 160: 109-114
- Knoblich R, Failing Jr JF. Giant condyloma acuminatum (Buschke-Löwenstein tumor) of the rectum. Am J Clin Pathol 1967; 48 (04) 389-395
- Davis KG, Barton JS, Orangio G, Bivin W, Krane S. Buschke-Lowenstein tumors: a review and proposed classification system. Sex Transm Dis 2021; 48 (12) e263-e268
- El Bessi M, Dougaz W, Jones M, Jerraya H, Dziri C. A giant anorectal condyloma is not synonym of malignancy. J Gastrointest Cancer 2019; 50 (04) 1026-1028
-
- Ben Kridis W, Werda I, Charfi S. et al. Buschke—Lowenstein anal tumor: an ambiguous entity. Exp Oncol 2019; 41 (02) 182-184
- Chu QD, Vezeridis MP, Libbey NP, Wanebo HJ. Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum 1994; 37 (09) 950-957
- Sandhu R, Min Z, Bhanot N. A gigantic anogenital lesion: Buschke-Lowenstein tumor. Case Rep Dermatol Med 2014; 2014: 650714
- Diani M, Boneschi V, Ramoni S, Gadda F, Del Gobbo A, Cusini M. Rapidly invasive Buschke-Löwenstein tumor associated with human papillomavirus types 6 and 52. Sex Transm Dis 2015; 42 (10) 547-548
- Bastola S, Halalau A, Kc O, Adhikari A. A gigantic anal mass: Buschke-Löwenstein tumor in a patient with controlled HIV infection with fatal outcome. Case Rep Infect Dis 2018; 2018: 7267213
- Chu QD, Vezeridis MP, Libbey NP, Wanebo HJ. Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum 1994; 37 (09) 950-957
- Hicheri J, Jaber K, Dhaoui MR, Youssef S, Bouziani A, Doss N. Giant condyloma (Buschke-Löwenstein tumor). A case report. Acta Dermatovenerol Alp Panonica Adriat 2006; 15 (04) 181-183
- Ahsaini M, Tahiri Y, Tazi MF. et al. Verrucous carcinoma arising in an extended giant condyloma acuminatum (Buschke-Löwenstein tumor): a case report and review of the literature. J Med Case Rep 2013; 7 (273) 273
- Neagu M, Caruntu C, Constantin C. et al. Chemically induced skin carcinogenesis: Updates in experimental models (Review). Oncol Rep 2016; 35 (05) 2516-2528
- Tripoli M, Cordova A, Maggì F, Moschella F. Giant condylomata (Buschke-Löwenstein tumours): our case load in surgical treatment and review of the current therapies. Eur Rev Med Pharmacol Sci 2012; 16 (06) 747-751
- Spinu D, Rădulescu A, Bratu O, Checheriţă IA, Ranetti AE, Mischianu D. -. Giant condyloma acuminatum - Buschke-Lowenstein disease - a literature review. Chirurgia (Bucur) 2014; 109 (04) 445-450
- Papiu HS, Dumnici A, Olariu T. et al. Perianal giant condyloma acuminatum (Buschke-Löwenstein tumor). Case report and review of the literature. Chirurgia (Bucur) 2011; 106 (04) 535-539
Address for correspondence
Publication History
Article published online:
18 July 2024
© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Buschke-Löwenstein Anal Tumour in Children: Two Case ReportsA. Schneider, European Journal of Pediatric Surgery, 2009
- Buschke-Löwenstein Anal Tumour in Children: Two Case ReportsA. Schneider, European Journal of Pediatric Surgery, 2009
- Buschke-Lowenstein tumor in a patient with HIV and PsoriasisJosé Antonio Dias da Cunha e Silva, Journal of Coloproctology, 2020
- Difficulties of diagnosis and treatment in giant condyloma of Buschke and Löwenstein (GCBL) which led to fatal outcome in a womanG. Kovács, Zeitschrift für Gastroenterologie, 2004
- Successfully treated patient with verrucous carcinoma developed from anogenital giant condylomaD Kári, Zeitschrift für Gastroenterologie, 2009
- A phenomenological analysis of the movie “Melancholia” by Lars Von Trier<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Preface to Special Issue: Cancer epidemiology, risk factors and screening<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Extranodal lymphoma: pathogenesis, diagnosis and treatment<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Phaeohyphomycosis caused by Corynespora cassiicola, a plant pathogen worldwide<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Advances in the applications of CRISPR/Cas system for tumor molecular diagnostics<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
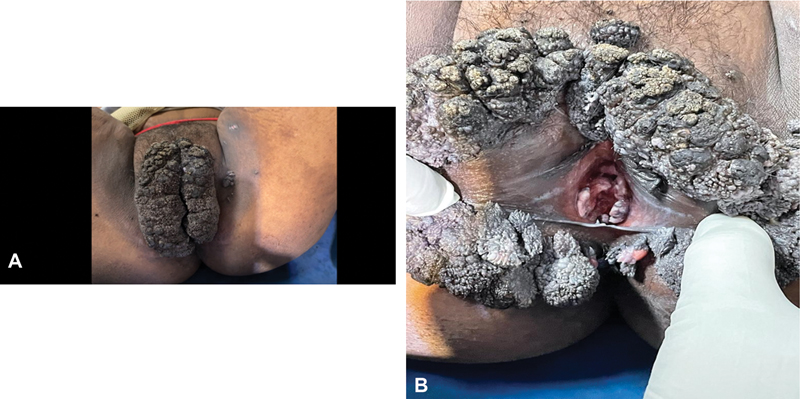
Fig 1: (A, B) Cauliflower-like growth that involved both of her labia majora and extended anteriorly to the mons pubis and posteriorly to the perianal region.
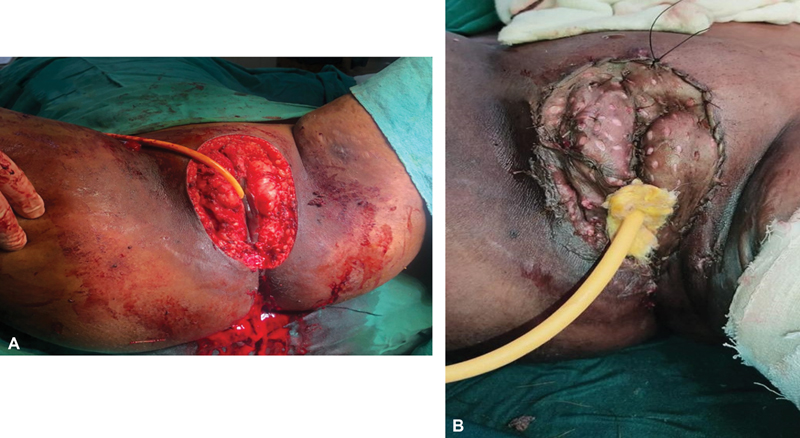
Fig 2 : (A, B) Intraoperative picture. (A) Simple vulvectomy. (B) Split skin grafting done over the defect.
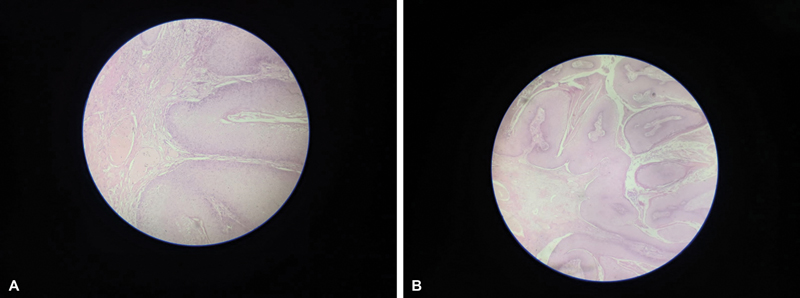
Fig 3 : (A, B) Histopathology image showing papillary proliferation of squamous epithelium with acanthosis and koilocytosis.
References
- Niazy F, Rostami K, Motabar AR. Giant condyloma acuminatum of vulva frustrating treatment challenge. World J Plast Surg 2015; 4 (02) 159-162
- Koutsky L. Epidemiology of genital human papillomavirus infection. Am J Med 1997; 102 (5A): 3-8
- Steffen C. The men behind the eponym–Abraham Buschke and Ludwig Lowenstein: giant condyloma (Buschke-Loewenstein). Am J Dermatopathol 2006; 28 (06) 526-536
- Trottier H, Burchell AN. Epidemiology of mucosal human papillomavirus infection and associated diseases. Public Health Genomics 2009; 12 (5-6): 291-307
-
- Stanley M. Immune responses to human papillomavirus. Vaccine 2006; 24 (Suppl. 01) S16-S22
- von Krogh G, Lacey CJ, Gross G, Barrasso R, Schneider A. European course on HPV associated pathology: guidelines for primary care physicians for the diagnosis and management of anogenital warts. Sex Transm Infect 2000; 76 (03) 162-168
- Frei W. About carcinoma similar pointed condyloma on the penis. Arch Derm Syph 1930; 160: 109-114
- Knoblich R, Failing Jr JF. Giant condyloma acuminatum (Buschke-Löwenstein tumor) of the rectum. Am J Clin Pathol 1967; 48 (04) 389-395
- Davis KG, Barton JS, Orangio G, Bivin W, Krane S. Buschke-Lowenstein tumors: a review and proposed classification system. Sex Transm Dis 2021; 48 (12) e263-e268
- El Bessi M, Dougaz W, Jones M, Jerraya H, Dziri C. A giant anorectal condyloma is not synonym of malignancy. J Gastrointest Cancer 2019; 50 (04) 1026-1028
-
- Ben Kridis W, Werda I, Charfi S. et al. Buschke—Lowenstein anal tumor: an ambiguous entity. Exp Oncol 2019; 41 (02) 182-184
- Chu QD, Vezeridis MP, Libbey NP, Wanebo HJ. Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum 1994; 37 (09) 950-957
- Sandhu R, Min Z, Bhanot N. A gigantic anogenital lesion: Buschke-Lowenstein tumor. Case Rep Dermatol Med 2014; 2014: 650714
- Diani M, Boneschi V, Ramoni S, Gadda F, Del Gobbo A, Cusini M. Rapidly invasive Buschke-Löwenstein tumor associated with human papillomavirus types 6 and 52. Sex Transm Dis 2015; 42 (10) 547-548
- Bastola S, Halalau A, Kc O, Adhikari A. A gigantic anal mass: Buschke-Löwenstein tumor in a patient with controlled HIV infection with fatal outcome. Case Rep Infect Dis 2018; 2018: 7267213
- Chu QD, Vezeridis MP, Libbey NP, Wanebo HJ. Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum 1994; 37 (09) 950-957
- Hicheri J, Jaber K, Dhaoui MR, Youssef S, Bouziani A, Doss N. Giant condyloma (Buschke-Löwenstein tumor). A case report. Acta Dermatovenerol Alp Panonica Adriat 2006; 15 (04) 181-183
- Ahsaini M, Tahiri Y, Tazi MF. et al. Verrucous carcinoma arising in an extended giant condyloma acuminatum (Buschke-Löwenstein tumor): a case report and review of the literature. J Med Case Rep 2013; 7 (273) 273
- Neagu M, Caruntu C, Constantin C. et al. Chemically induced skin carcinogenesis: Updates in experimental models (Review). Oncol Rep 2016; 35 (05) 2516-2528
- Tripoli M, Cordova A, Maggì F, Moschella F. Giant condylomata (Buschke-Löwenstein tumours): our case load in surgical treatment and review of the current therapies. Eur Rev Med Pharmacol Sci 2012; 16 (06) 747-751
- Spinu D, Rădulescu A, Bratu O, Checheriţă IA, Ranetti AE, Mischianu D. -. Giant condyloma acuminatum - Buschke-Lowenstein disease - a literature review. Chirurgia (Bucur) 2014; 109 (04) 445-450
- Papiu HS, Dumnici A, Olariu T. et al. Perianal giant condyloma acuminatum (Buschke-Löwenstein tumor). Case report and review of the literature. Chirurgia (Bucur) 2011; 106 (04) 535-539


 PDF
PDF  Views
Views  Share
Share

